Open Journal of Epidemiology
Vol. 2 No. 4 (2012) , Article ID: 24724 , 4 pages DOI:10.4236/ojepi.2012.24014
Risk factors distribution and cardiovascular disease prevalence in the Italian population: The CHECK study
![]()
1Epidemiology and Preventive Pharmacology Centre (SEFAP), University of Milano, Milano, Italy
2Italian Society of General Medicine (SIMG), Firenze, Italy
3Kingston University, Kingston upon Thames, UK
4IRCCS Multimedica, Sesto S. Giovanni, Milano, Italy
Email: *alberico.catapano@unimi.it
Received 5 August 2012; revised 15 September 2012; accepted 8 December 2012
Keywords: Italian Population; Epidemiological Study; Cardiovascular Risk Factors; Prevalence of Cardiovascular Disease
ABSTRACT
Objective: To evaluate the distribution of cardiovascular risk factors and the prevalence of cardiovascular disease in a sample of the Italian population. Methods: CHECK (Cholesterol and Health: Education, Control and Knowledge) is a cross-sectional observational study in a randomised sample of the Italian adult population aged 40 - 79 years, in the setting of general practice. Results: 5846 subjects (50.3% male) were included in the analysis. The mean age [±SD] of the observed cohort was 57.8 (±10.3) years. One out of five subjects smoked cigarettes and almost 80% didn’t engage in regular leisure-time physical activity. The mean blood pressure was 132.0 [±14.7]/81.2 [±7.9] mmHg. The total and LDL-cholesterol levels were respectively 205.3 [±35.9] mg/dL and 124.9 [±29.9] mg/dL. The mean glucose concentration was 98.3 [±28.2] mg/dL. The prevalence rate of hypertension, hypercholesterolemia, and type 2 diabetes were respectively 51.8%, 55.6%, and 13.0%. 8.9% of the observed subjects had a history of cardiovascular events, while in the primary prevention group the 10-yearrisk of coronary heart disease (Framingham algorithm) was 10.1% [±8.3%] and of cardiovascular disease (CUORE algorithm) was 5.2% [±5.9%]. Conclusion: The CHECK study provides a detailed description of a randomised sample of the Italian population, contributing to evaluate the prevalence of cardiovascular risk factors and the main cardiovascular disease in Italy and to provide a baseline to set priorities and objectives for future intervention of health policy.
1. INTRODUCTION
Cardiovascular diseases (CVD), a group of disorders of the heart and blood vessels, including coronary heart disease, cerebrovascular disease, peripheral arterial disease, are the leading cause of morbidity, disability and mortality worldwide, showing a continue increasing trend. In 2008, CVD caused 17 million deaths (47.2% of noncommunicable diseases deaths, 29.8% of total deaths in the world) [1]; in particular, 7.6 million deaths were due to ischemic heart disease and 5.7 million to stroke [2].
CVD remains the first cause of death and disability in Italy although a slow and stepwise reduction of incidence has been observed since the mid seventies [3,4].
The subjects who survive acute cardiovascular events are likely to become chronic patients. CVD compromise patients’ quality of life and represent a significant economic burden to the national health system. Cardiovascular drugs account for about 26.4% of the Italian Pharmaceutical expenditure [5].
The CHECK (Cholesterol and Health: Education, Control and Knowledge) study was designed to provide information on the distribution of the main CVD risk factors in Italy setting the stage for addressing questions relative to the plausibility and feasibility of interventions on the principal risk factors for CVD in an European country.
CHECK is the first randomised Italian epidemiological study performed in primary care. Its main objective was to evaluate the distribution of cardiovascular risk factors and the prevalence of cardiovascular disease in a representative sample of the Italian adult population aged 40 - 79 years. Other aims were 1) to perform a follow-up study to determine the incidence of cardiovascular events and other main pathologies, 2) to create plasma and DNA banks to design ad-hoc nested case-control studies, 3) to disseminate information about cardiovascular risk factors to increase physicians and patients awareness and contribute to the implementation of evidences supporting health policies and preventive strategies in the population.
In this paper we describe baseline characteristics of enrolled subjects.
2. MATERIAL AND METHODS
The study was conducted in accordance to the Declaration of Helsinki, Guidelines for Good Clinical practice, and the Italian bioethics regulations and laws. The study was approved by the local Ethic Committee and all subjects gave written informed consent to the study (protocol code SEFAP/Pr. 0003).
2.1. Study Design
The Italian Society of General Medicine (SIMG) identified 54 general practitioners (coordinators) that were active at local level and distributed throughout the Italian territory (both rural and urban areas) in proportion to the regional population density. Each coordinator had to contact other general practitioners (GPs) who were operating on the same territory, to reach a group of 14 GPs.
Overall, 764 GPs were invited to participate to the study as investigators. They had to meet all the following pre-requisites:
• age: <52 years;
• practice size: >1000 subjects;
• computerised patient records system;
• access to the web.
The GPs who adhered to the proposal had to registered in the project website and to provide some personal information and their patients number. Each investigator was required to enrol 16 subjects aged 40 to 79 years, randomly selected among his patients, following a random number list generated by the coordinating Centre in Milan based on self-reported number of patients. The patient selection procedure was subject to random control by the local coordinators. Subjects who didn’t give their consensus or who were not eligible for practical reasons (e.g. subjects with walking disabilities, severe handicap, or suffering from an invaliding disease or a severe mental illness) were excluded from the randomized sample. The subjects’ enrolment started in March 2002 and ended in June 2005.
2.2. Data Collection
Subjects’ clinical history and clinical information were collected during a standardised visit performed by the investigating physician.
Information about smoking habit, physical activity, alcohol use and chronic drug treatments were collected directly from the patient during the same examination. Smoking habit was classified as current (patient smoking at least one cigarette per day) or former (at least one year from smoking cessation). Self-reported leisure-time physical activity was classified as present or non-present. The use of alcohol was evaluated by adding the consumption of red and/or white wine, beer and liquors. Information on chronic therapies was also collected.
Weight and height measures, obtained from lightly clothed patients, were expressed in terms of body mass index (BMI, weight in kilos divided by the square value of height, in meters).
The measurement of blood pressure (BP) was performed with the patient in sitting position, after 4 minute of rest, applying the appropriate cuff on the right arm. Systolic and diastolic blood pressure was identified at the beginning of the first and the fifth phase of the Korotkoff sounds, using a mercury sphygmomanometer with the appropriate cuff. Three consecutive readings were recorded and their mean was considered for the analysis. Heart rate was assessed as beats per minute after the last measurement of BP.
The presence of angina pectoris or of a history of myocardial infarction, coronary artery bypass graft or coronary angioplasty, stroke, transient ischemic attacks, claudicatio and left ventricular hypertrophy were assessed by retrieving the medical records of the subject and by direct inquiry. Subjects with a history of cardiovascular events (excluding left ventricular hypertrophy) were considered in secondary prevention.
Family history for premature cardiovascular diseases was determined when episodes of stroke and/or myocardial infarction were reported for one or more first-degree relatives, <55 years old for men and <65 years old for women. Family history for hypertension, dislipidemia, and diabetes was also evaluated.
All relevant subject records were entered in a computerized patient chart directly by the investigating physician and then sent to a central server via web.
Blood samples were drawn at the beginning of the enrolment visit. Blood was obtained between 8 to 10 am, from the antecubital vein, in sitting position, after 12 hours of fasting and alcohol abstinence. Blood samples were then collected in EDTA or monoiodine-acetate (only for glucose assessment) coated tubes and shipped by courier at 4˚C temperature to the central laboratory (Fleming SpA, in Brescia, Italy) within 24 hours, where the biochemical parameters were determined. The biochemical evaluation was performed following the criteria of the World Health Organization Lipid Reference Laboratories.
Upon arrival, the samples were centrifuged to obtain the plasma. Levels of total cholesterol (TC), glucose and triglycerides (TG) were measured by a chromatometric enzymatic method; the plasma levels of apolipoprotein B by a latex enhanced turbidimetric immuno-assay. Plasma HDL cholesterol levels (HDL-C) were measured after the precipitation of the apolipoprotein B containing lipoproteins with dextran-magnesium-chloride. All determinations were performed by an automatic analyzer (ADVIA 1650; Bayer, Germany). Fibrinogen plasma levels (1.8 - 3.5 g/L) were assessed by a turbidimetric method with Nefelometro BNA 100 (Boehring, Italia). The low density lipoprotein cholesterol (LDL-C) values were calculated using the Friedewald formula (TC minus HDL-C minus 1/5 TG).
Serum 1 mL aliquots (4 - 5 for each sample) were frozen at −80˚C for further biochemical evaluation. White cells were frozen at −20˚C for polymorphism search/ genetic research.
Criteria used for specific diagnosis were:
• Hypercholesterolemia: plasma levels of TC ≥ 200 mg/dL or LDL-C ≥130 mg/dL or pharmacological treatment with statins and/or simvastatin + ezetimibe.
• Hypertriglyceridemia: plasma levels of TG ≥ 170 mg/ dL or pharmacological treatment with fibrates and/or omega-3.
• Mixed dyslipidemia: hypercholesterolemia and hypertriglyceridemia, as defined above.
• Hypertension: recorded diagnosis by physician or systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg or currently taking medication to lower high BP (NHANES criteria [6]).
• Type 2 diabetes mellitus: recorded diagnosis by physician or fasting blood glucose levels ≥ 126 mg/dL or currently taking antidiabetic drugs (oral hypoglycaemic medication and/or insulin).
• Overweight: body mass index (BMI) ≥ 25 and <30 kg/m2;
• Obesity: BMI ≥ 30 kg/m2;
• Metabolic Syndrome (MetS): presence of at least 3 of 5 of the listed characteristics [7]: abdominal obesity, given as waist circumference, men > 102 cm, women > 88 cm; triglycerides ≥ 150 mg/dL; HDL cholesterol, men < 40 mg/dL, women < 50 mg/dL; blood pressure ≥ 130/85 mmHg; fasting glucose ≥ 110 mg/dL. BMI was used as a surrogate of waist circumference, men ≥ 28 kg/m2, women ≥ 25 kg/m2 (approach validated in a subgroup of about 1000 subjects: assignment to MetS/noMetS consistent in 92% of cases in males and 97% in females).
The coronary heart disease risk (CHD risk % in 10 years) was calculated using the Framingham algorithm [8], as recommended at the time of the study by the Italian regulatory Agency (AIFA) for the prescription of statin drugs [9]; the global cardiovascular risk (CVD risk % in 10 years) was evaluated using the CUORE algorithm [10], developed from epidemiological data obtained in Italy, as reported by Italian recommendations since 2003 [11]. Based on Framingham or CUORE scores, subjects were stratified in four risk classes (<5% low-risk; 5% - 10% mild-risk; 10% - 20% moderaterisk; ≥20% high risk).
2.3. Statistical Analysis
Normally distributed variables are presented as mean values [±standard deviation, SD] and not normally distribute variables as median [interquartile range, IQR], while qualitative variables are presented as frequencies. Comparisons between continuous variables across sex groups were performed by using the t-test for independent sample. Comparisons between proportions across sex groups for categorical (and qualitative) variables were performed by using non-parametric tests. All reported p-values are based on two-sided tests and compared to a significance level of 5%.
All statistical analyses were performed using the Windows 16.0 version of SPSS (SPSS, Inc., Chicago, Illinois).
3. RESULTS
432 GPs participated to the CHECK study (mean age 47.8 years, 80.1% male; 56.5% participation rate). Each of them enrolled up to 16 subjects, following the randomised sampling procedure. Overall, 6890 subjects were enrolled; 1044 (15.1%) of them did not attend the medical visit and were excluded from the study sample; the blood samples of 131 subjects (1.9%) were not processable, although their anamnestic data were included in the analysis.
5846 subjects were included in the final analysis (Figure 1). Men were 49.7% of the cohort. The mean age was 57.8 years (58.2 years for men and 57.4 for women). Comparison between the Check demographics and the latest available census data [12] showed small difference: women were slightly under-represented in the CHECK sample (50.3% vs. 52.6% respectively); the 50 - 59 and 60 - 69 age groups, conversely, were slightly over-represented (30.5% vs. 27.0% and 28.0% vs. 24.6%, respectively).
The main outcomes of the study are shown in Tables 1-4. The average level of education is quite low: 33.0% of subjects achieved only primary education, but this percentage was higher in women (36.7% vs. 29.2%). 32.9% reported to be retired, with a high proportion of men (65.8%); 23.3% were housewives (45.8% of the female sample). Smoke habit and alcohol consumption were more prevalent in men (24.3% vs. 18.6% and 62.4% vs. 28.4%, respectively), whereas physical inac-
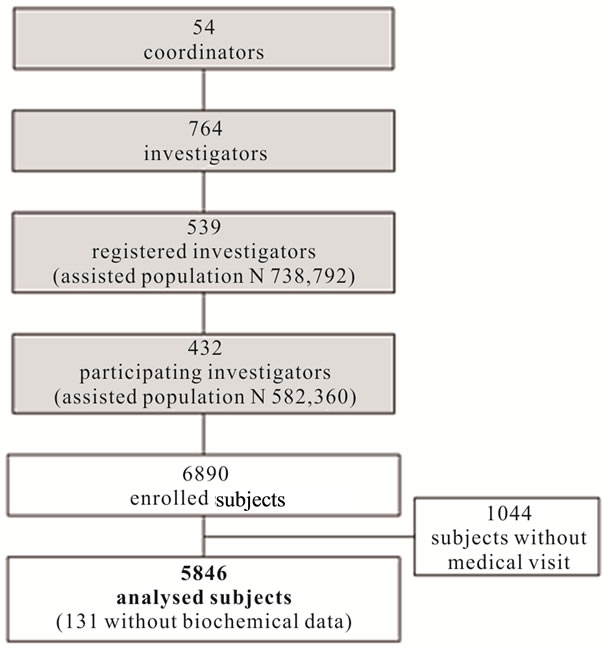
Figure 1. Flow chart of the study.
tivity was more present in women (84.1% vs. 75.0%) (Table 1).
Mean BMI (±SD) was 26.5 ± 4.3 kg/m2, putting the sample in the overweight range; this was observed in both genders. Mean SBP/DPB values were (132.0 ± 14.7)/(81.2 ± 7.9) mm Hg, slightly higher than cut off for pre-hypertension. Mean total cholesterol was 205.3 ± 35.9 mg/dL, while LDL-cholesterol was 124.9 ± 29.9 mg/dL, the former just higher and the latter slightly lower than desirable levels, due to HDL-cholesterol values (54.8 ± 12.2 mg/dL) (Table 2).
As shown in Table 3, 51.8% of subjects were hypertensive, 13.0% were diabetic, and 55.6%/20.8% were hypercholesterolemic/hypertriglyceridemic. 8.6% had a history of cardiovascular events and thus could be defined as in secondary CV prevention. The 65.0% of the remaining subjects had a global CV risk in 10 years (calculated with CUORE algorithm) lower than 5%, with a remarkable difference between genders (mean values: 7.8% ± 7.1% in men vs. 2.8% ± 3.1% in women) (Table 4).
4. DISCUSSION
The main objective of the CHECK study was to evaluate the cross-sectional prevalence of CVD and cardiovascular risk factors in a cohort of randomly selected Italian subjects, aged 40 to 79 years.
The CHECK sample proved to be representative of the Italian population in the same age range. The differences observed by comparing the Check demographics to the latest available census data [12] are small, and of limited relevance. This was probably due to a larger participation to the study of subjects in a non-working age or condition.
The CHECK study provided a detailed and in depth description of the prevalence of cardiovascular risk factors and the main cardiovascular pathologies in the Italian population. In order to put our findings into a wider context, we compare them with other national surveys, while maintaining a worldwide perspective.
Smoking is estimated to cause nearly 10% of cardiovascular disease (5.4 millions of deaths) [13]. Currently, there are about 1 billion smokers worldwide [14]. The proportion of smoking subjects in the CHECK sample was 21.4% (men 24.3% and women 18.6%). These figures were slightly lower than the official census data (24.5% in 2003, 22.6% in 2004) [15]; the Check cohort excluded the 25 - 34 age group, the one with the highest prevalence of smokers (31.4%), especially among men. The reduced prevalence of smokers in the CHECK cohort, as compared to previous epidemiological data [16], could also reflect the declining smoking habits in the Italian population, as a result of educational programs and smoking restrictions enforced in public buildings.
Physical inactivity is one of the leading risk factors for mortality and is estimated to cause about 30% of ischaemic heart disease burden [13]. Globally, around 31% of adults are insufficiently active (men 28% and women 34%) [17]. Concerning leisure-time physical activity, the self-reported information obtained from the CHECK cohort were less favourable than the data derived from other studies. The prevalence of physical inactivity was 75% in men and 84% in women, vs. 34% in men and 46% in women observed, as an example, in the Atlante study [18].
Overweight and obesity lead to adverse metabolic effects on blood pressure, cholesterol, triglycerides and insulin resistance [13]; all over the world, 2.8 million people die each year as a result of being overweight [13]. A total of more than half a billion adults worldwide are obese [19]. The mean BMI of the CHECK cohort was 26.5 kg/m2, well within the overweight range. 17.4% of the cohort subjects were obese, with a higher prevalence in women than in men (18.8% vs. 16.0%, respectively). In the PASSI study, a national survey (self-reported information) conducted on younger people aged 18 - 69 years [20], 32% of Italians are overweight, while one in ten is obese [21].
Raised blood pressure is the leading risk factor for cardiovascular disease mortality, causing more than 7 million deaths every year worldwide. Globally, prevalence of hypertension in adults is around 40% [13]. In our study, the mean blood pressure value was 132.0/81.2 mmHg. Hypertension was present in more than half of the sample, with a higher prevalence in men (54.1% M vs. 49.5% W). The CHECK mean SBP values were comparable to those obtained in other Italian observational
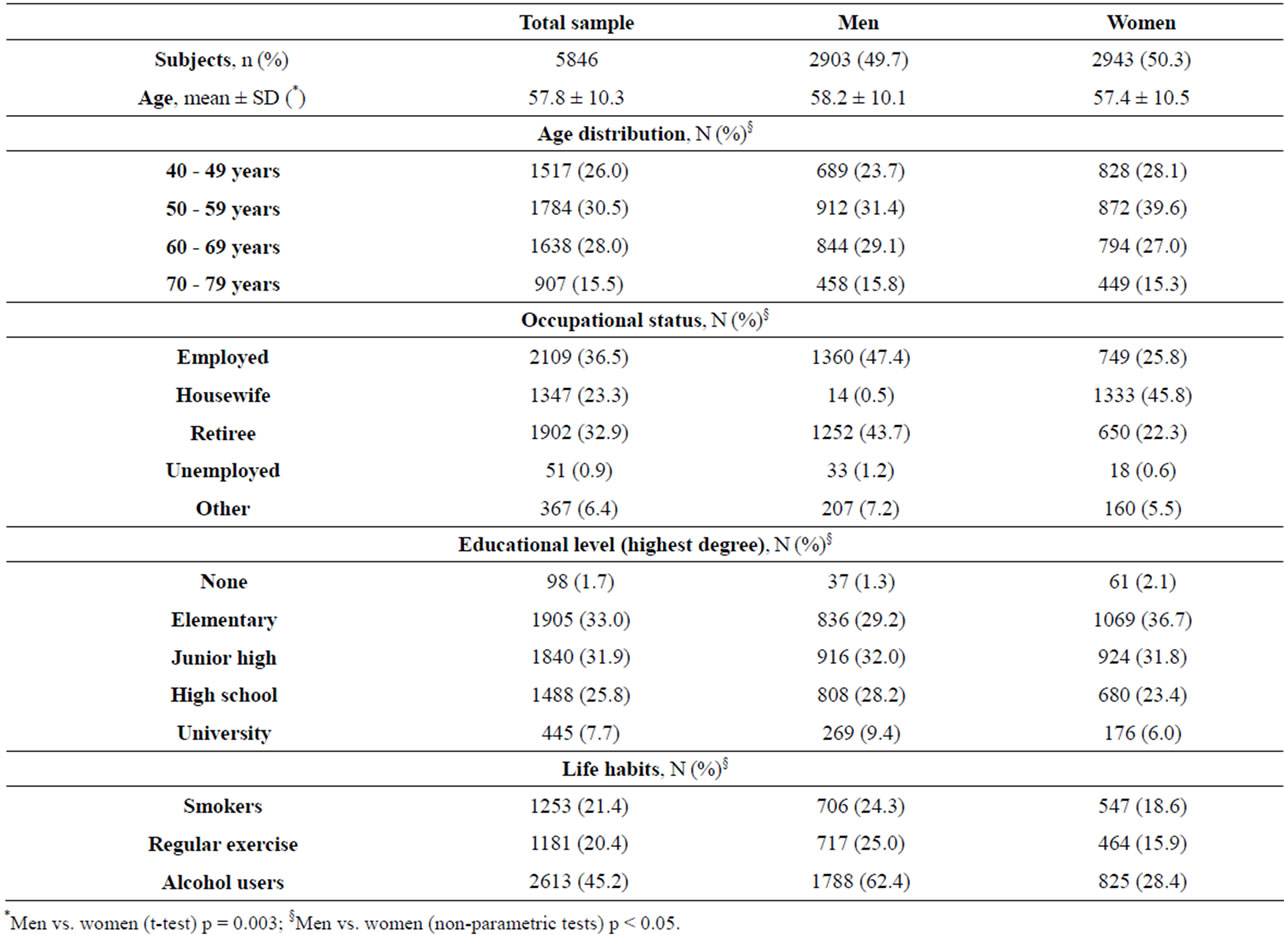
Table 1. Sociodemographic and lifestyle characteristics in total and sex-stratified sample.

Table 2. Anthropometric, vital and biochemical parameters in total and sex-stratified sample, mean ± SD.

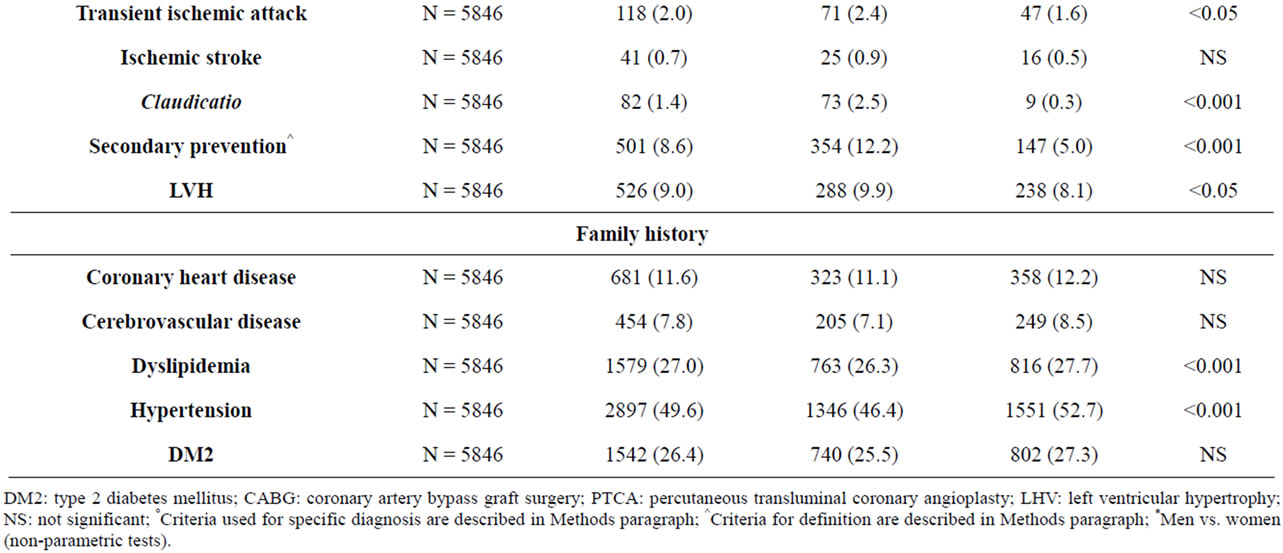
Table 3. Prevalence of cardiovascular disease and related comorbidities in total and sex-stratified sample, N (%).
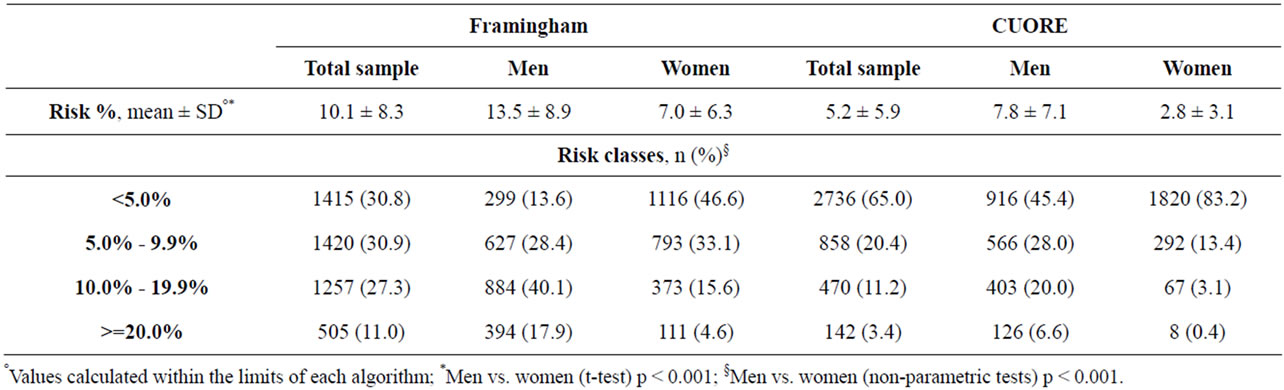
Table 4. CHD-risk classes and CVD-risk classes in total and sex stratified sample.
studies, while the DBP values resulted slightly lower (82 - 86 mmHg) [18]. Compared to the population sample observed in the Atlante study, the CHECK cohort showed a higher overall incidence of hypertensive subjects (52% M vs. 45% W), possibly due to a higher prevalence of older subjects in the CHECK sample.
Raised total cholesterol is a major cause of disease burden as a risk factor for ischaemic heart disease and stroke. Overall, it is estimated to cause 2.6 million deaths (4.5% of total). The global prevalence of hypercholesterolemia among adults is about 39% [13]. The mean plasma total cholesterol levels in the CHECK cohort were 205.3 mg/dL. The prevalence of hypercholesterolemia was 55.6%. Hypertriglyceridemia and mixed dyslipidemia were identified in 20.8% and 14.8% of the enrolled subjects, respectively. Lipid data observed in the CHECK and in the Atlante study showed relevant similarities: in both cohorts, women showed a higher level of TC, LDL-C, and HDL-C than the same level reported for men, but lower TG values. TC mean values observed in the CUORE population [22], on the other hand, were significantly higher than those found in CHECK (CUORE 225.4 mg/dL M and 229.0 mg/dL W vs. CHECK 202.5 mg/dL M and 208.0 mg/dL W). This difference is consistent with the trend of progressive reduction of blood TC levels observed over the last decades in Italy.
Impaired glucose tolerance and impaired fasting glycaemia are risk categories for future development of diabetes and cardiovascular disease [23]. A 2004 survey showed that more than 3 million people died from consequences of high blood sugar [24]. The global prevalence of diabetes is estimated to be 10% [13]. In the CHECK cohort, the mean level of fasting glucose was 98.3 mg/dL (101.7 M vs. 94.9 W). Based on GPs diagnosis and/or presence of anti-diabetes therapies and/or plasma glucose levels ≥ 126 mg/dL, type II diabetes prevalence was 13.0%. This prevalence was higher than that observed in the Health Search GP’s database of Italian general practice [25] for similar age (10% - 11%; unpublished observation). This difference can be partially explained by different diagnostic criteria (based on at least two assessments in clinical practice compared to the single time determination in the CHECK study protocol), or by the identification of previously unknown cases in the CHECK sample, due to the generalised screening. In the Atlante cohort, the mean fasting glucose levels was lower (93 mg/dL M vs. 87 mg/dL W), leading to a lower prevalence of type II diabetes (Atlante 9% M and 6% W vs. CHECK 15.6% M and 10.4% W). This difference could be partially explained by the different timeframe of the two studies (Atlante from 1998 vs. CHECK from 2001): over the last years, a generalised increase in the prevalence of type II diabetes in Western populations has been observed. Moreover, in the Atlante study the blood glucose level was estimated from a sample of capillary blood, where glucose concentrations are on average significantly lower than in plasma.
Cardiovascular disease is the number one cause of death globally. In Italy, an estimated almost 240,000 people died from CVDs in 2008, representing 41% of all total deaths [26]. A clinical history of previous cardiovascular events was observed in 8.6% of the individuals included in the CHECK sample. The prevalence of such diagnosis was twice as high in men than in women. The prevalence of a clinical history of myocardial infarction was higher in the CHECK than in the Atlante study, especially in men (CHECK 5.3% M and 0.9% W vs. Atlante 1.5% M and 0.4% W). The difference could be explained by the different methodological approach (information collected in a GP interview vs. hospital validation) and age differences.
The risk of future fatal and non-fatal cardiovascular events was assessed using two different algorithms, based on the outcomes of the Framingham and the Cuore cohorts. The mean coronary risk at 10 years, calculated with the Framingham algorithm, was 10.1%, while the cardiovascular risk calculated with the CUORE algorithm showed an average value of 5.2%. This difference was expected, since the Framingham algorithm is known to over-estimate the coronary risk of the Italian population [27]. Compared to the CUORE population data [28], the mean cardiovascular risk for the CHECK cohort was slightly lower (CUORE 7.8% M and 2.8% W vs. CHECK 8.7% M and 3.3% W).
The innovative design of the CHECK study responded to the emerging need of determining the prevalence of cardiovascular risk factors directly from primary care, following a rigorous and unbiased research methodology. The randomisation of the sample, the web-based data collection of primary data, the territorial quality control operated by local coordinators, and the centralised laboratory procedures increase the external validity of the study, conferring a general significance to the epidemiological outcomes.
A follow-up of the cardiovascular events (fatal and nonfatal) occurred to all enrolled subjects is currently ongoing. It will provide the opportunity to evaluate the underlying prevalence of factors predisposing the onset of cardiovascular disease. Moreover, frozen samples provide the possibility of further biochemical evaluations, as the characterization of specific population subgroups through polymorphism search/genetic research.
The assessment of the gap between risk factor levels and recommended targets will provide evidence to aid clinical decision making about tailored non pharmacological and pharmacological interventions and to achieve optimal resources allocation.
The CHECK study has some methodological limitations, previously described. Importantly, the prevalence of cardiovascular events could have been underestimated, as the participating general practitioners reported those events at best of their knowledge, simply transcribing the diagnose related groups (DRG) codification of the events as reported by the hospital discharge letter, without any form of control on the appropriateness of the diagnoses. In addition, the peculiar design of the study, with progressive steps of GPs involvement, determined a participation rate lower than expected. The fact that local investigators did not participate in the enrolment meetings with the coordinating Centre, but were trained by their coordinators, may have weakened their motivation. However, no significant differences have been found between actively participating GPs and those who did not complete the preliminary steps.
5. CONCLUSIONS
The CHECK study confirmed the significant burden caused by the cardiovascular disease to the health care system and to society. In the randomised cohort observed, 1 out of 2 subjects was suffering from high blood pressure or high cholesterol, 1 out of 5 was obese and 1 out of 10 was a type 2 diabetic. The elevated prevalence of lifestyle risk factors observed in the Italian population raises the issue of moral hazard: the limited willingness of subjects covered by the National Healthcare System to take action and modify behavioural risks, in favour of deferring the issue to pharmacological prevention or treatment of the cardiovascular events at a later stage. While this normative issue is well known in economics of public health, the CHECK findings on the prevalence and co-occurrence of key behavioural and clinical risk factors is an emerging concern and it demands further research. Despite the fact that most subjects included in the study had been followed-up by general practitioners for years, the vast majority of them still showed the presence of one or more risk factors.
The high proportion of subjects with multiple risk factors in combination with the elevated prevalence of cardiovascular disease projects a shadow on the effectiveness of current cardiovascular prevention policies in primary care. The epidemiological outcomes of this study could be used as a baseline to set priorities and objectives for future intervention, as well as a benchmark, against which the effectiveness of the implementation of future prevention policies in primary care should be measured. The further development of the CHECK study is aimed to facilitate the recognition and to improve the management of cardiovascular diseases in the Italian general practice.
6. ACKNOWLEDGEMENTS
The CHECK study was supported in part by an unconditioned educational grant from AstraZeneca SpA. Thanks to Maria Grazia Lanfranco and Elena Loggia for their assistance in completing our survey.
REFERENCES
- Alwan, A., Maclean, D.R., Riley L.M., et al. (2010) Monitoring and surveillance of chronic non-communicable diseases: Progress and capacity in high-burden countries. Lancet, 376, 1861-1868. doi:10.1016/S0140-6736(10)61853-3
- Fuster, V. and Kelly, B.B. (2010) Promoting Cardiovascular Health in the Developing World: A Critical Challenge to Achieve Global Health. Committee on Preventing the Global Epidemic of Cardiovascular Disease: Meeting the Challenges in Developing Countries. Institute of Medicine. National Academies Press, Washington.
- ERA (2009) Epidemiologia e Ricerca Applicata. http://www.atlantesanitario.it/index.php?option=com_content&view=article&id=82&Itemid=93
- ISTAT (2012) GeoDEMO. http://demo.istat.it/unitav/index.html?lingua=ita
- AIFA (2012) Rapporti OsMed—L’uso dei farmaci in Italia. http://www.agenziafarmaco.gov.it/it/content/rapporti-osmed-luso-dei-farmaci-italia
- CDC (2011) National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/nhanes.htm
- Adult Treatment Panel III (2001) Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Journal of the American Medical Association, 285, 2486-2497. doi:10.1001/jama.285.19.2486
- Anderson, K.M., Wilson, P.W., Odell, P.M. and Kannel, W.B. (1991) An updated coronary risk profile. A statement for health professionals. Circulation, 83, 356-362. doi:10.1161/01.CIR.83.1.356
- AIFA (2012) Le nuove note CUF. BIF 5-6/2000. http://www.agenziafarmaco.gov.it/it/content/bif-5-62000
- Palmieri, L., Panico, S., Vanuzzo, D., et al. (2004) Evaluation of the global cardiovascular absolute risk: The Progetto CUORE individual score. Ann Ist Super Sanita, 40, 393-399.
- AIFA (2012) Le note. BIF 2/2004. http://www.agenziafarmaco.gov.it/it/content/bif-22004
- ISTAT (2012) 14 censimento generale della popolazione e delle abitazioni. http://dawinci.istat.it/MD/
- WHO (2009) Global health risks mortality and burden of disease attributable to selected major risks. World Health Organization, Geneva.
- WHO (2012) Tobacco. http://www.who.int/mediacentre/factsheets/fs339/en/index.html
- ISTAT (2012) Condizioni di salute e ricorso ai servizi sanitari: I fumatori in Italia. http://www3.istat.it/salastampa/comunicati/non_calendario/20060110_00/
- Zuccaro, P., Pacifici, R., Giampaoli, S., et al. (2001) Fumo: Il contesto epidemiologico nazionale. Ital Heart Journal, 2, 13-18.
- WHO (2012) Physical inactivity: A global public health problem. http://www.who.int/dietphysicalactivity/factsheet_inactivity/en/
- OEC (2004) Atlante italiano delle malattie cardiovascolari—Second edition. Ital Heart Journal, 5, 1S-101S.
- Finucane, M.M., Stevens, G.A., Cowan, M.J., et al. (2011) National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet, 377, 557-567. doi:10.1016/S0140-6736(10)62037-5
- Baldissera, S., Campostrini, S., Binkin, N., et al. (2011) Features and initial assessment of the Italian Behavioral Risk Factor Surveillance System (PASSI), 2007-2008. Preventing Chronic Disease, 8, A24.
- Trinito, M., Bertozzi, N., Bietta, C., et al., (2006) Analisi di alcuni fattori di rischio cardiovascolari nella popolazione delle ASL partecipanti allo studio PASSI. Notiziario dell’Istituto Superiore di Sanità, 19, iii-iv.
- ISS (2012) Il Progetto CUORE: Assetto lipidico. http://www.cuore.iss.it/fattori/colesterolemia.asp
- Levitan, E.B., Song, Y., Ford, E.S. and Liu, S. (2004) Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Archives of Internal Medicine, 164, 2147-2155. doi:10.1001/archinte.164.19.2147
- WHO (2012) Diabetes. http://www.who.int/mediacentre/factsheets/fs312/en/
- Filippi, A., Vanuzzo, D. Bignamini, A.A., Sessa, E. Brignoli, O. and Mazzaglia, G. (2005) Computerized general practice databases provide quick and cost-effective information on the prevalence of angina pectoris. Ital Heart Journal, 6, 49-51.
- WHO (2011) Noncommunicable diseases country profiles. World Health Organization, Geneva.
- Menotti, A., Puddu, P.E. and Lanti, M. (2000) Comparison of the Framingham risk function-based coronary chart with risk function from an Italian population study. European Heart Journal, 21, 365-370. doi:10.1053/euhj.1999.1864
- ISS (2012) Il Progetto CUORE: Rischio cardiovascolare globale assoluto. http://www.cuore.iss.it/fattori/RischioGlobaleAssoluto.asp
Appendix
Participating Investigators in the CHECK Study Group (Bold Type for Coordinators)
Aalders Maria Anna Abbate Giuseppe Agati Riccardo Alano Raffaele Alba Mauro Alemagna Silvia Alunni Massimo Alvaro Antonio Amato Fabio Ammendola Erminia Amodeo Vincenzo Amoretti Giovanni Andrani Alberto Antiga Ivo Appolonia Giorgio Aramini Enrico Arisi Marco Emilio Artebani Adriano Atzei Massimiliano Azzolini Micheline Bachetti Francesco Bagagli Franco Baldicchi Lorella Banzi Roberta Barba Ettore Maria Barbato Pasquale Claudio Barral Gino Battaggia Alessandro Battigelli Doriano Baudi Marina Bellumori Giovanni Beltrami Giuseppe Benincasa Anna Maria Berardi Mario Berlengiero Claudio Bernardelli Stefano Bernardi Giuseppe Bertelle Evandro Bettini Gianluca Bevacqua Giuseppe Bevilacqua Stefano Bianconi Giuseppe Biggioggero Giovanni Bini Vincenzo Bocchino Giancarlo Boccone Nicolfranco Boito Giancarlo Bollo Alberto Maria Boncompagni Salvatore Bond Giuseppe Bonesi Maria Grazia Bono Gianfranco Boscaro Federica Bossi Paolo Bozza Giulio Bracone Enrico Brandodoro Lucio Brasesco Pierclaudio Breviario Adele Brizzi Antonio Brugnetta Maurizio Bruno Giuseppe Buemi Giuseppe Bufano Carmine Bugli Tiziano Burigo Daniela Buzzatti Agostino Caccamo Orazio Antonio Cadamosti Danilo Cagliesi Francesco Caleffa Manuela Cammisa Nicolo’
Campo Franceso Campobello Margherita Caputo Stanislao Caraccio Nicola Cardi Silvio Cardinale Fulvio Caregnato Massimo Cariola Gianni Carlino Saverio Carminati Luisa Angela Carnelli Feliciano Carnesalli Franco Caruso Ciro Casale Ezio Casini Marcella Cassanelli Marco Castiello Maria Luisa Castriotta Antonio Catalano Domenico
Cataldi Maria Elvira Ceccarini Agostino Celebrano Mario Celora Amedeo Cerracchio Alessandro Cesaro Andrea Cesaro Federico Chiriatti Alberto Cipriani Rosa Collura Giuseppe Colombo Valter Coluccia Salvatore Conte Sergio Corda Andrea Costa Roberto Cottani Antonio Crivellenti Giuseppe D’Ambrosio Gaetano D’Angelo Massimo Dalla Rosa Rosanna Damico Giansanto De Andreis Bessone Pier Luigi De Benedictis Antonio De Conto Umberto De Mola Cosimo De Rosa Antonio De Tommasi Roberto Del Nero Barbara Della Briotta Ivana Dell’Orco Mario Domenico Dell’Orco Mario Lucio Di Candia Giuseppe Di Carlo Vittorio Di Febo Enrico Di Feo Antonio Di Fraia Giovanni Di Fulvio Aristide Di Nardo Dionisio Dolmetta Franco Donzelli Luigi Dughiero Fausto Durando Andrea Ercolino Luigi Fabbri Stelania Fabrizio Nicola Falchi Raffaello Fariello Ciro Fascendini Emilvio Fasulo Serenella Federici Laura Ferioli Paolo Ferrari Vincenzo Fidelbo Melchiorre Filetti Giuseppe Filippini Giovanni Fogher Michele Franchini Carlo Andrea Frascati Angelo Frignani Patrizia Fronteddu Pier Francesco Gadaleta Caldarola Gennaro Galantini Giovanna Gallicchio Nicola Gallina Franco Gallo Silvano Gambino Fortunato Gambuzza Guglielmo Garaffa Elio Garagiola Alberto Garofalo Remigio Garrone Alfonsino Gatta Luigi Gennari Massimo Gerace Antonio Geremia Maria Alessandra Germini Fabrizio Giacci Luciano Giannini Olivia Giordano Stefano Giovannelli Umberto Giuffré Giuseppe Giunti Giuliana Glaviano Bruno Gorletta Giovanni Grand Paola Grassini Giovanni Grasso Anna Maria Grasso Giuseppe Grasso Maria Filomena Greco Agostino Grifagni Marcello Grilli Piero Grimaldi Emanuela Grimaldi Nicola Grosso Marco Guarnera Lucia Guerra Antonio Guillaro Bruno Gussoni Barbara Rita Ianiro Gabriella Ilardi Salvatore Imbalzano Pasquale Inguscio Cherubino Invernizzi Giovanni Iocca Tommaso Kos Egidia La Mattina Rosolino La Torre Angelo Lacava Cosimo Lalli Pasqualino Lamera Giorgio Lanza Gerardo Lardo Gerardo Laringe Matteo Lattanzio Giuseppe Le Foche Luca Leo Rosanna Leuzzi Giacomo Lipari Antonino Lipari Francesco Lippa Luciano Lo Conte Maurizio Lo Giudice Domenico Lonati Rossella Lorenzina Enrico Magi Lorenzo Magliozzo Francesco Mallamo Luciano Mantovani Licia Marcenaro Alessandro Marchetti Anna Rosa Mariano Carlo Marino Antonino Mariuz Manuela Maroni Achille Martori Ampelio Masoch Gigliola Mattioli Carlo Mattioli Mauro Maurici Vincenzo Mauro Nicola Mazzardi Lidia Mazzi Wainer Mazzocchetti Alvaro Mazzoleni Francesco Mazzorana Michela Medagliani Giorgio Medea Gerardo Merlino Giovanni Merone Laura Metrucci Antonio Mezzano Silvio Micchi Alessio Micheli Pietro Severo Milazzo Vito Minafra Francesco Minetti Luca Mirandola Cipriano Monari Gianluigi Mongiello Claudio Montano Giovanni Montera Carmine Moretti Marino Morgana Ignazio Morganti Mauro Mormile Annunziata Moro Roberto Mostacciolo Francesco Mourglia Danilo Murari Tiziana Muratore Alessandro Murgia Rosalba Naccari Massimo Napoli Luigi Nardacci Giuseppe Nebiacolombo Cristina Negri Fabrizio Nicolini Gianfranco Nigro Antonio Noia Emanuela Nuti Claudio Pietro Olivani Enrico Orlando Celestina Padovan Letizia Padula Maria Stella Pagan Maurizio Pannacci Valerio Pantalone Vincenzo Paolini Italo Papandrea Giampaolo Papini Giovanni Papulino Francesco Paradisi Enza Parisi Carmela Parretti Damiano Pasculli Domenico Pasinelli Pietro Carlo Pasqualetto Salvatore Passamonti Marco Passaro Vincenzo Pederzani Fabio Pedrazzoli Giuliano Pelizzari Pier Carlo Pernici Pierrenato Pesaresi Carlo Pesce Gian Luigi Petrucci Marco Petrucci Mauro Petrulli Carmela Petti Stefano Piccinocchi Gaetano Picciotto Rinaldo Piccolo Francesco Pierobon Ivo Pilone Rita Piva Roberto Pizzillo Carlo Plebani Franco Polistina Stefano Pontari Antonino Poppi Maria Cristina Portanti Carla Prencipe Giovanni Prestifilippo Alessandro Procopio Antonio Profeta Gaetano Proietti Carlo Quattrocchi Pietro Raciti Teodoro Ragazzoni Anna Rattini Emanuela Reale Emanuela Redaelli Dario Reggiani Claudio Ricotta Giuseppe Rigamonti Rodolfo Righini Velella Rinaldi Vanna Rista Pierangela Romano Salvatore Romei Federico Rossi Alberto Rossi Angelo Rossi Francesco Rossi Gianluca Rosso Lucia Rovazzani Massimo Rovelli Monica Rovescala Pietroclaudio Rubicini Giuseppe Rubini Stefano Russo Carolina Russo Vincenzo Sala Massimo Salurso Daniele Salvaderi Maria Dionice Salvato Alberto Salvetti Andrea Salvio Giuliano Samani Fabio Sammarco Renato Santoiemma Luigi Santoro Michele Sassarini Graziano Savino Andrea Scaglione Matteo Scarano Libero Schiavone Ciro Scola Vincenzo Scorpiniti Anna Scotto D’Antuono Antonio Scovotto Maria Antonietta Scuri Maurizio Giovanni Scuteri Antonio Sebastianelli Giuliano Sebben Maurizio Sforza Pasqualino Sfragara Ignazio Sicari Giuseppe Simonini Giorgio Soldani Miriam Soverina Patrizio Spagnolo Beatrice Sperandio Massimo Spezzano Alfredo Steri Lia Storni Paolo Strada Sonia Stramenga Carlo Tagliabue Paola Fausta Tarabini Legnoaura Tarallo Nicola Tei Alessandro Tei Gian Paolo Testi Sergio Testolin Ennio Tibo Angela Titone Nicolò
Tomasello Antonino Tondi Lidia Torti Giorgio Tommaso Toscano Emanuele Tota Maria Fiorenza Tozzoli Alfonso Travaglini Rita Trois Paolo Trotta Gaetano Tuia Bruno Turbil Enrico Ughetti Claudio Urru Cesare Valdevit Maria Valente Fabio Valenti Marco Valle Lucia Valletta Domenico Valore Salvatore Varriale Antonio Varrica Gaetano Ventriglia Giuseppe Venturelli Antonio Vesco Giuseppe Vezzosi Angelo Viola Dario Viscusi Bruno Vita Salvatore Vitali Franco Vittozzi Dante Sergio Vivona Giacomo Volpe Augusto Volponi Damiano Antonio Voza Italo Zadra Alessandro Zaninetti Piero Zanini Riccardo Zennaro Walter Zingaro Angelo Zito Alfonso Zollino Luciana Zovi Maria Carla Zunino Roberto
NOTES
*Corresponding author.
#As presented in Appendix.

