Open Journal of Stomatology
Vol.4 No.5(2014), Article ID:45888,6 pages DOI:10.4236/ojst.2014.45034
A Case of Giant Epidermoid Cyst in the Floor of the Mouth That Caused Severe Obstructive Sleep Apnea Syndrome
Norimichi Nakamoto1,2, Tsuyoshi Sato2, Yoshie Sano2, Makoto Kabeya2, Yuichiro Enoki2, Yasuaki Sakata2, Tetsuya Yoda2
1Division of Oral and Maxillofacial Biopathological Surgery, Tottori University Faculty of Medicine, Yonago, Japan
2Department of Oral and Maxillofacial Surgery, Saitama Medical School, Moroyama, Japan
Email: ae86nory@yahoo.co.jp
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 25 March 2014; revised 29 April 2014; accepted 6 May 2014
ABSTRACT
We describe here, a case with a giant epidermoid cyst in the floor of the mouth that caused severe obstructive sleep apnea syndrome (OSAS). A 37-year-old man was referred to our clinic because of a swelling in the floor of his mouth and sleep apnea syndrome. The occurrence of breathing disorders and daytime drowsiness was monitored to evaluate his OSAS 1 day before and 7 days after surgery. Before surgery, the apnea-hyponea index (AHI) and Epworth Sleepiness Scale (ESS) were 45.7 and 22, respectively. The clinical diagnosis was a dermoid or an epidermoid cyst that caused severe OSAS. Under general anesthesia, the patient underwent intraoral surgical removal of the cyst, along with aspiration to reduce the mass. After surgery, his sleep apnea syndrome was significantly improved. The postoperative AHI and ESS were 5.5 and 7, respectively. As of 2 years after the operation, there was no evidence of recurrence.
Keywords:Epidermoid Cyst, Obstructive Sleep Apnea Syndrome, Apnea-Hyponea Index

1. Introduction
Epidermoid and dermoid cysts are benign lesions encountered throughout the body, with 7% occurring in the head and neck region and 1.6% within the oral cavity [1] . They represent <0.01% of all oral cavity cysts [2] . The cysts can be defined as epidermoid if the lining is comprised of only epithelium, dermoid if skin adnexa are found, and teratoid if other tissues such as muscle, cartilage, and bone are present [3] . The pathogenesis of midline cysts of the floor of the mouth is not well established, and dysontogenetic, traumatic, and thyroglossal anomaly theories have been suggested. Dermoid cysts in the floor of the mouth generally present with slow and progressive growth, so they frequently reach a large size [4] . Such a swelling on the floor of the mouth can occasionally cause serious swallowing, speaking and breathing problems [5] [6] .
2. Case Report
In February 2011, a 37-year-old male patient was admitted to our hospital with complaints of a mass in the oral cavity and snoring while sleeping for the past 10 years. He also noticed difficulty breathing while asleep. The swelling had been present since he was in high school. There was no relevant past medical, dental, or surgical history. A physical examination revealed a height of 178 cm, weight of 83.3 kg, and body mass index (BMI) of 26.3 g/m2.
A large swelling involving the submental and sublingual areas was revealed. The mass was not freely movable. The tongue was elevated to the extent of the soft palate, and the tip of the tongue could not be visualized (Figure 1(a) and Figure 1(b)).
A T2-weighted magnetic resonance image (MRI) showed a sharply circumscribed, high-intensity, 83 × 36 × 63 mm cystic mass that extended inferomedially to the genioglossus muscle and inferiorly to the mylohyoid muscle (Figure 2).
A polysomnographic (PSG) study demonstrated an apnea hypopnea index (AHI) of 45.7/h and a minimal SpO2 of 79%. He presented with an Epworth Sleepiness Scale (ESS) of 22. He was diagnosed with a dermoid cyst or an epidermoid cyst that caused severe OSAS (Table 1).
Under general anesthesia, with nasotracheal intubation, the patient underwent surgical removal of the cyst. An
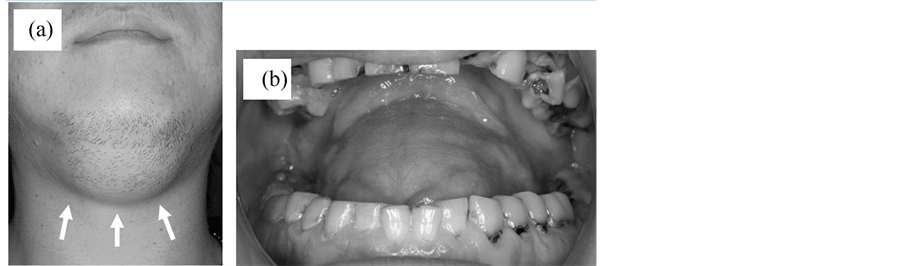
Figure 1. (a) Clinical pre-operative presentation of submental swelling; (b) Intraoral swelling in the floor of the mouth.
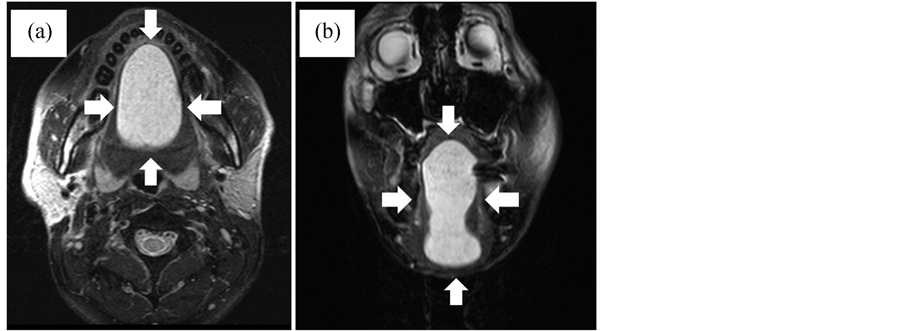
Figure 2. Pre-opeartive MR images (T2 weighted, SE 467/87) (a) Horizontal view; (b) Coronal view.
intraoral midline incision was created from the base of the tongue to the floor of the mouth. Blunt dissection was done to separate the submucosa and cyst capsule. The cyst was almost exposed, and upon evaluation, a partial caudal herniation through the mylohyoid muscle was seen (Figure 3(a)). Aspiration of the swelling was done to reduce the mass. The aspirate was a cream cheese-like material. The whole capsule was removed. The lingual nerve was not exposed.
A vacuum drain was placed in the submandibular region, and the oral mucosa was sutured with a 3 - 0 absorbable suture. The drain was left in situ for a day.
The postoperative period was without any complications and the tongue returned to its normal position a week after the operation (Figure 4(a) and Figure 4(b)). A week the after operation, a PSG study showed a significant improvement in his OSAS, demonstrating an AHI of 5.5/h and a minimal SpO2 of 93%. The ESS score was 7 (Table 1). The patient was discharged 10 days after the operation. A postoperative MRI (Figure 5(a) and Figure 5(b)) obtained 2 weeks after the operation showed that the cystic space had resolved. The patient did well postoperatively, and no recurrence was noticed at a 2-years follow up.
Grossly, the lesion was cystic, well demarcated, and measured 70 × 45 × 35 mm (Figure 3(b)). The surgical
Table 1. Scores of PSG and ESS (AI: arousals per hour, CA: central apnea per hour, OA: obstructive apnea per hour, HYP: hyponea per hour).
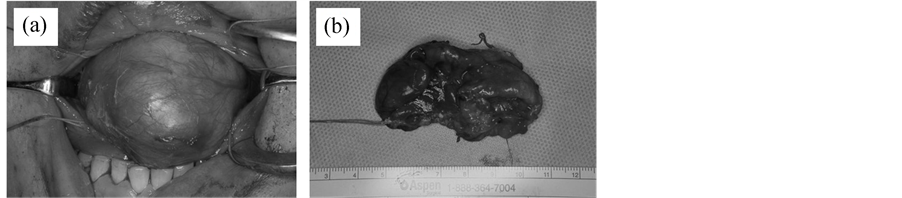
Figure 3. (a) Intraoral midline excision from the base of the tongue to the fllor of the mouth; (b) The whole capsule was removed.
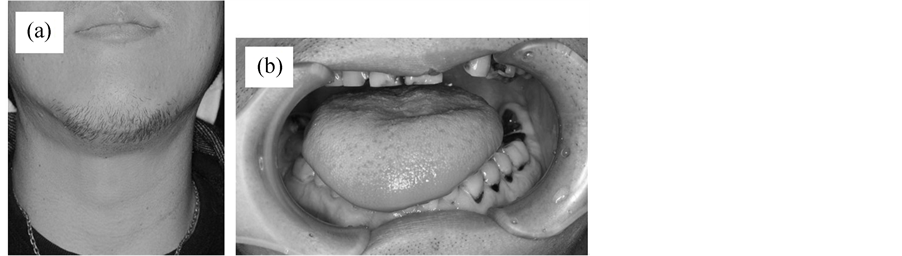
Figure 4. Clinical a weekpost-operative presentation (a) Extraoral view; (b) Intraoral view.
specimen was submitted for a histopathologic examination. The histopathology showed areas of both stratified squamous and pseudostratified columnar epithelia in a cystic lining without any skin appendages that was consistent and confirmatory of an epidermoid cyst diagnosis (Figure 6).
3. Discussion
OSAS caused by a complete or partial obstruction of the upper airway that produces apnea or hypopnea is a sleep disorder characterized by a repetitive cessation of breathing while sleeping [7] [8] .
It is an independent risk factor for many diseases such as hypertension, heart failure, heart attack, cardiovascular events, and arrhythmias [9] . The most widely used technique for evaluating sleep and diagnosing OSAS is PSG [10] , which monitors the sleeping state, respiration, electrocardiogram, leg movements, oximetry, and snoring. PSG also provides the AHI; in this context, apnea is very serious and can only be treated surgically with an AHI of >30, while an AHI of 15 - 30 defines moderate apnea and an AHI of <15 indicates mild apnea. The ESS is intended to measure the single factor somnoficity. The instrument requests that subjects rate the likelihood that they would “doze off or fall asleep” in eight different common daily living situations “in recent times”, such as “sitting and reading” or “watching TV.” The ESS requests that respondents “try to work out how they
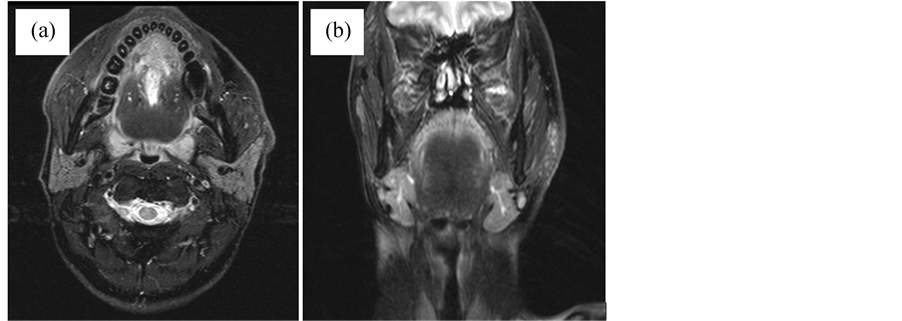
Figure 5. MR images taken two weeks after operation (T2 weighted, SE 467/87) (a) Horizontal view; (b) Coronal view.
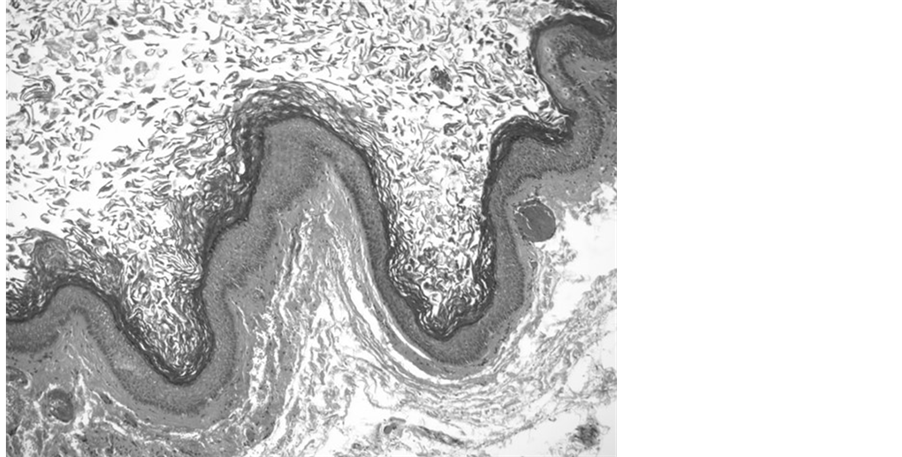
Figure 6. Histopathological images H & E stain (×100) showing both stratified squamous and pseudostratified columnar epithelium.
would have affected you” even if the respondents have not performed a given activity recently. However, the ESS has a fault: low reproducibility.
Our case complained of difficulty with swallowing, speaking, and snoring as well as apnea while sleeping. Obesity, a principal risk factor of OSAS, had not been shown in this case and was considered to have a low relation with the symptoms. Thus, we believed the increasing mass on the floor of the mouth had caused an upper airway obstruction and decided to perform a total removal of the cyst under general anesthesia. These alterations decreased the tongue space, causing it to lie in a more posterior position, where it caused obstruction of the upper airway during sleep. Comparison of the preand postoperative PSG results showed a significant improvement in our case. We believed the upper airway obstruction improved as a result of the tongue returning to its original position.
The surgical approach for an epidermoid cyst in the floor of the mouth is determined in accordance with its localization and size [11] . Several techniques are reported in medical literature that may be divided into intraoral and extraoral techniques depending on which approach is used [3] . An extraoral approach is generally preferred in the case of median geniohyoid or very large sublingual cysts, whereas an intraoral approach is typically used for smaller sublingual cysts [12] . For an extraoral incision, it is necessary to consider the risk of a facial nerve injury, scaring of the submental skin, and an intra-extraoral fistula. Prognosis for dermoid cysts in the floor of the mouth is very good, with a very low incidence of relapse. Malignant changes have been recorded in dermoid cysts by New and Erich, but not in the floor of the mouth. The epidermoid cystic cavity is usually lined with thick squamous epithelium, and dissection to separate the adjacent structures is easy. Thus, if applying an intraoral approach, aspiration of a giant epidermoid cyst to reduce the mass provides a sufficient field of view for surgeons, enabling them to remove the cyst completely.
Considering the above-mentioned issues, an intraoral approach is the most useful and effective treatment for large lesions and leads to very good cosmetic and functional results [13] [14] , whereas an extraoral incision is necessary if dissection is difficult.
4. Conclusion
We experienced a case of a giant epidermoid cyst causing severe OSAS. After using an intraoral surgical approach, along with aspiration to reduce the mass, the whole cyst was removed. A pre and postoperative evaluation of the AHI suggested that an increasing mass in the floor of mouth caused an upper airway obstruction, and removal of the cyst was effective for the improvement of OSAS.
References
- Turetschek, K., Hospodka, H. and Steiner, E. (1995) Case Report: Epidermoid Cyst of the Floor of the Mouth: Diagnostic Imaging by Sonography, Computed Tomography and Magnetic Resonance Imaging. The British Journal of Radiology, 68, 205-207. http://dx.doi.org/10.1259/0007-1285-68-806-205
- Rajayogeswaran, V. and Eveson, J.W. (1989) Epidermoid Cyst of the Buccal Mucosa. Oral Surgery, Oral Medicine, Oral Pathology, 67, 181-184. http://dx.doi.org/10.1016/0030-4220(89)90326-5
- Calderon, S. and Kaplan, I. (1993) Concomitant Sublingual and Submentalepidermoid Cysts: A Case Report. Journal of Oral and Maxillofacial Surgery, 51, 790-792. http://dx.doi.org/10.1016/S0278-2391(10)80425-2
- Walstad, W.R., Solomon, J.M., Schow, S.R. and Ochs, M.W. (1998) Midline Cystic Lesion of the Floor of the Mouth. Journal of Oral and Maxillofacial Surgery, 56, 70-74. http://dx.doi.org/10.1016/S0278-2391(98)90919-3
- Koca, H., Seckin, T., Sipahi, A. and Kazanc, A. (2007) Epidermoid Cyst in the Floor of the Mouth: Report of a Case. Quintessence International, 38, 473-477.
- Bitar, M.A. and Kumar, S. (2003) Plunging Congenital Epidermoid Cyst of the Oral Cavity. European Archives of Oto-Rhino-Laryngology, 260, 223-225.
- Guilleminault, C. and Eldridge, F.L. (1973) Insomnia with Sleep Apnea: A New Syndrome. Science, 181, 856-858. http://dx.doi.org/10.1126/science.181.4102.856
- Strollo, P.J. and Rogers, R.M. (1996) Obstructive Sleep Apnea. The New England Journal of Medicine, 334, 99-104. http://dx.doi.org/10.1056/NEJM199601113340207
- Laube, I., Seeger, R., Russi, E.W. and Bloch, K.E. (1998) Accidents Related to Sleepiness: Review of Medical Causes and Prevention with Special Reference to Switzerland. Schweizerische Medizinische Wochenschrift, 128, 1487-1499.
- Kushida, C.A., Littner, M.R., Morgenthaler, T., Alessi, C.A., Bailey, D. and Coleman Jr., J. (2005) Practice Parameters for the Indications for Polysomnography and Related Procedures: An Update for 2005. Sleep, 28, 499-521.
- Longo, F., Maremonti, P., Mangone, G.M., De Maria, G. and Califano, L. (2003) Midline (Dermoid) Cysts of the Floor of the Mouth: Report of 16 Cases and Review of Surgical Techniques. Plastic & Reconstructive Surgery, 112, 1560- 1565. http://dx.doi.org/10.1097/01.PRS.0000086735.56187.22
- Lowry, R.E., Tempero, R.M. and Davis, L.F. (1979) Epidermoid Cyst of the Floor of the Mouth. Journal of Oral Surgery, 37, 271-273.
- Akao, I., Nobukiyo, S., Kobayashi, T., Kikuchi, H. and Koizuka, I. (2003) A Case of Large Dermoid Cyst in the Floor of the Mouth. Auris Nasus Larynx, 30, 137-139. http://dx.doi.org/10.1016/S0385-8146(02)00121-9
- El-Hakim, I.E. and Alyamani, A. (2008) Alternative Surgical Approaches for Excision of Dermoid Cyst of the Floor of Mouth. International Journal of Oral and Maxillofacial Surgery, 37, 497-499. http://dx.doi.org/10.1016/j.ijom.2007.12.004


