The Preauricular Sinus: A Novel Approach for Complete
Bilateral Excision via a Modified Face-Lift Incision
78
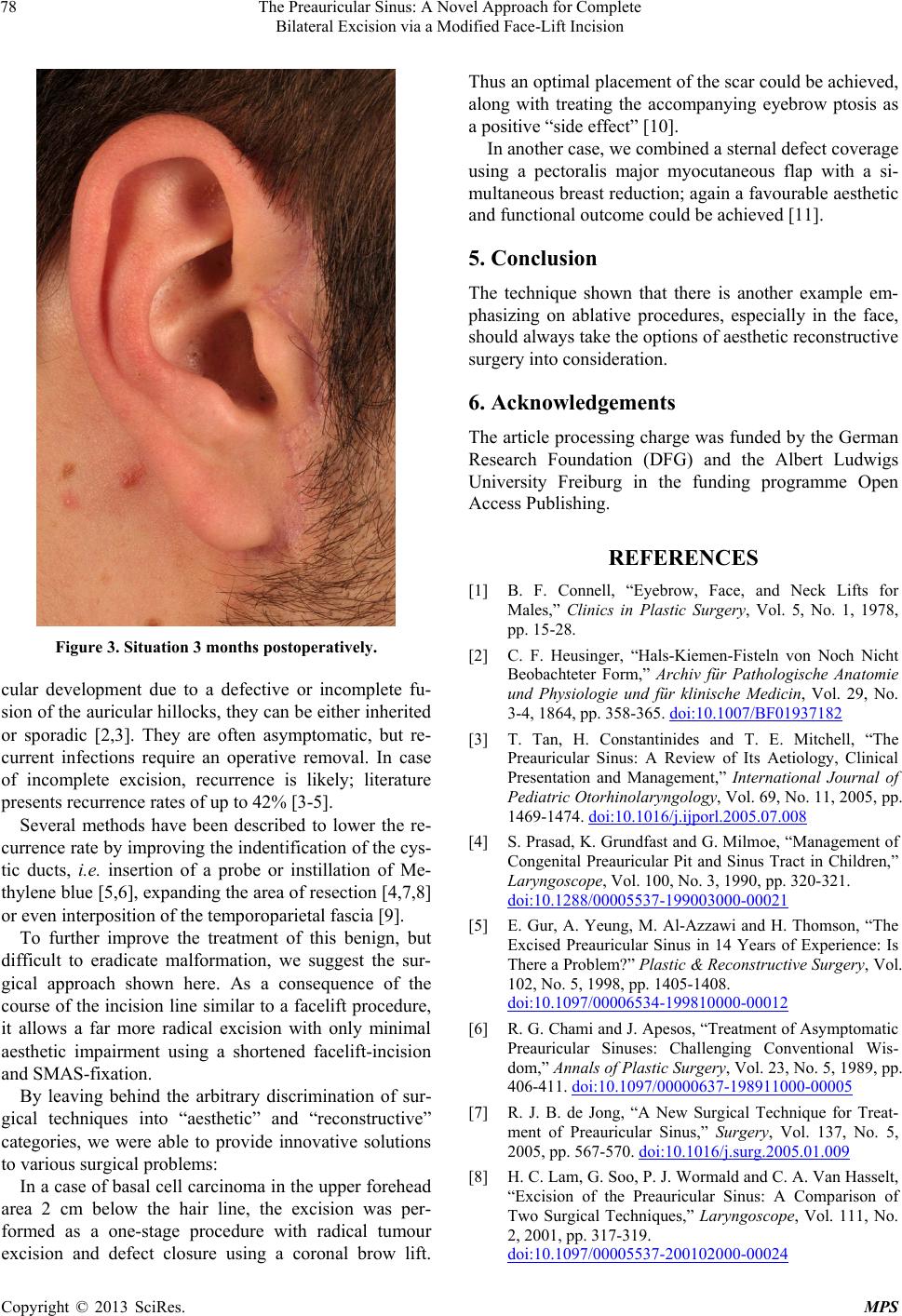
Figure 3. Situation 3 months postoperatively.
cular development due to a defective or incomplete fu-
sion of the auricular hillocks, they can be either inherited
or sporadic [2,3]. They are often asymptomatic, but re-
current infections require an operative removal. In case
of incomplete excision, recurrence is likely; literature
presents recurrence rates of up to 42% [3-5].
Several methods have been described to lower the re-
currence rate by improving the indentification of the cys-
tic ducts, i.e. insertion of a probe or instillation of Me-
thylene blue [5,6], expanding the area of resection [4,7,8]
or even interposition of the temporoparietal fascia [9].
To further improve the treatment of this benign, but
difficult to eradicate malformation, we suggest the sur-
gical approach shown here. As a consequence of the
course of the incision line similar to a facelift procedure,
it allows a far more radical excision with only minimal
aesthetic impairment using a shortened facelift-incision
and SMAS-fixation.
By leaving behind the arbitrary discrimination of sur-
gical techniques into “aesthetic” and “reconstructive”
categories, we were able to provide innovative solutions
to various surgical problems:
In a case of basal cell carcinoma in the upper forehead
area 2 cm below the hair line, the excision was per-
formed as a one-stage procedure with radical tumour
excision and defect closure using a coronal brow lift.
Thus an optimal placement of the scar could be achieved,
along with treating the accompanying eyebrow ptosis as
a positive “side effect” [10].
In another case, we combined a sternal defect coverage
using a pectoralis major myocutaneous flap with a si-
multaneous breast reduction; again a favourable aesthetic
and functional outcome could be achieved [11].
5. Conclusion
The technique shown that there is another example em-
phasizing on ablative procedures, especially in the face,
should always take the options of aesthetic reconstru ctive
surgery into consideration.
6. Acknowledgements
The article processing charge was funded by the German
Research Foundation (DFG) and the Albert Ludwigs
University Freiburg in the funding programme Open
Access Publishing .
REFERENCES
[1] B. F. Connell, “Eyebrow, Face, and Neck Lifts for
Males,” Clinics in Plastic Surgery, Vol. 5, No. 1, 1978,
pp. 15-28.
[2] C. F. Heusinger, “Hals-Kiemen-Fisteln von Noch Nicht
Beobachteter Form,” Archiv für Pathologische Anatomie
und Physiologie und für klinische Medicin, Vol. 29, No.
3-4, 1864, pp. 358-365. doi:10.1007/BF01937182
[3] T. Tan, H. Constantinides and T. E. Mitchell, “The
Preauricular Sinus: A Review of Its Aetiology, Clinical
Presentation and Management,” International Journal of
Pediatric Otorhinolaryngology, Vol. 69, No. 11, 2005, pp.
1469-1474. doi:10.1016/j.ijporl.2005.07.008
[4] S. Prasad, K. Grundfast and G. Milmoe, “Management of
Congenital Preauricular Pit and Sinus Tract in Children,”
Laryngoscope, Vol. 100, No. 3, 1990, pp. 320-321.
doi:10.1288/00005537-199003000-00021
[5] E. Gur, A. Yeung, M. Al-Azzawi and H. Thomson, “The
Excised Preauricular Sinus in 14 Years of Experience: Is
There a Problem?” Plastic & Reconstructive Surgery, Vol.
102, No. 5, 1998, pp. 1405-1408.
doi:10.1097/00006534-199810000-00012
[6] R. G. Chami and J. Apesos, “Treatment of Asymptomatic
Preauricular Sinuses: Challenging Conventional Wis-
dom,” Annals of Plastic Surgery, Vol. 23, No. 5, 1989, pp.
406-411. doi:10.1097/00000637-198911000-00005
[7] R. J. B. de Jong, “A New Surgical Technique for Treat-
ment of Preauricular Sinus,” Surgery, Vol. 137, No. 5,
2005, pp. 567-570. doi:10.1016/j.surg.2005.01.009
[8] H. C. Lam, G. Soo, P. J. Wormald and C. A. Van Hasselt,
“Excision of the Preauricular Sinus: A Comparison of
Two Surgical Techniques,” Laryngoscope, Vol. 111, No.
2, 2001, pp. 317-319.
doi:10.1097/00005537-200102000-00024
Copyright © 2013 SciRes. MPS