I. Yokoyama / J. Biomedical Science and Engineering 6 (2013) 232-235
234
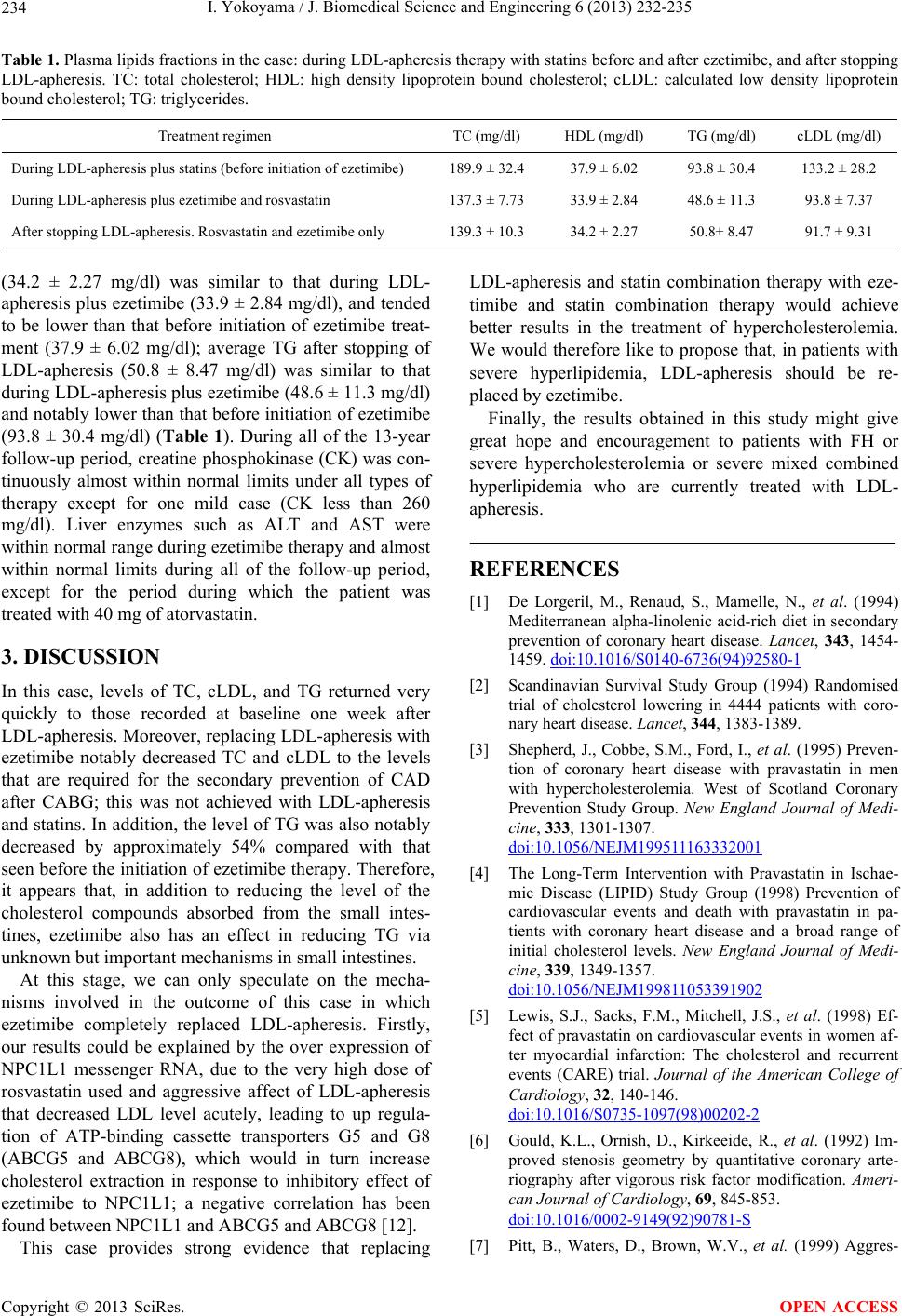
Table 1. Plasma lipids fractions in the case: during LDL-apheresis therapy with statins before and after ezetimibe, and after stopping
LDL-apheresis. TC: total cholesterol; HDL: high density lipoprotein bound cholesterol; cLDL: calculated low density lipoprotein
bound cholesterol; TG: triglycerides.
Treatment regimen TC (mg/dl) HDL (mg/dl) TG (mg/dl) cLDL (mg/dl)
During LDL-apheresis plus statins (before initiation of ezetimibe) 189.9 ± 32.4 37.9 ± 6.02 93.8 ± 30.4 133.2 ± 28.2
During LDL-apheresis plus ezetimibe and rosvastatin 137.3 ± 7.73 33.9 ± 2.84 48.6 ± 11.3 93.8 ± 7.37
After stopping LDL-apheresis. Rosvastatin and ezetimibe only 139.3 ± 10.3 34.2 ± 2.27 50.8± 8.47 91.7 ± 9.31
(34.2 ± 2.27 mg/dl) was similar to that during LDL-
apheresis plus ezetimibe (33.9 ± 2.84 mg/dl), and tended
to be lower than that before initiation of ezetimibe treat-
ment (37.9 ± 6.02 mg/dl); average TG after stopping of
LDL-apheresis (50.8 ± 8.47 mg/dl) was similar to that
during LDL-apheresis plus ezetimibe (48.6 ± 11.3 mg/dl)
and notably lower than that before initiation of ezetimibe
(93.8 ± 30.4 mg/dl) (Table 1). During all of the 13-year
follow-up period, creatine phosphokinase (CK) was con-
tinuously almost within normal limits under all types of
therapy except for one mild case (CK less than 260
mg/dl). Liver enzymes such as ALT and AST were
within normal range dur ing ezetimibe therapy and almost
within normal limits during all of the follow-up period,
except for the period during which the patient was
treated with 40 mg of atorvastatin.
3. DISCUSSION
In this case, levels of TC, cLDL, and TG returned very
quickly to those recorded at baseline one week after
LDL-apheresis. Moreover, replacing LDL-apheresis with
ezetimibe notably decreased TC and cLDL to the levels
that are required for the secondary prevention of CAD
after CABG; this was not achieved with LDL-apheresis
and statins. In addition, the level of TG was also notably
decreased by approximately 54% compared with that
seen before the initiation of ezetimibe therapy. Therefore,
it appears that, in addition to reducing the level of the
cholesterol compounds absorbed from the small intes-
tines, ezetimibe also has an effect in reducing TG via
unknown but important mechanisms in small intestines.
At this stage, we can only speculate on the mecha-
nisms involved in the outcome of this case in which
ezetimibe completely replaced LDL-apheresis. Firstly,
our results could be explained by the over expression of
NPC1L1 messenger RNA, due to the very high dose of
rosvastatin used and aggressive affect of LDL-apheresis
that decreased LDL level acutely, leading to up regula-
tion of ATP-binding cassette transporters G5 and G8
(ABCG5 and ABCG8), which would in turn increase
cholesterol extraction in response to inhibitory effect of
ezetimibe to NPC1L1; a negative correlation has been
found between NPC1L1 and ABCG5 and ABCG8 [12].
This case provides strong evidence that replacing
LDL-apheresis and statin combination therapy with eze-
timibe and statin combination therapy would achieve
better results in the treatment of hypercholesterolemia.
We would therefore like to propose that, in patients with
severe hyperlipidemia, LDL-apheresis should be re-
placed by ezetimibe.
Finally, the results obtained in this study might give
great hope and encouragement to patients with FH or
severe hypercholesterolemia or severe mixed combined
hyperlipidemia who are currently treated with LDL-
apheresis.
REFERENCES
[1] De Lorgeril, M., Renaud, S., Mamelle, N., et al. (1994)
Mediterranean alpha-linolenic acid-rich diet in secondary
prevention of coronary heart disease. Lancet, 343, 1454-
1459. doi:10.1016/S0140-6736(94)92580-1
[2] Scandinavian Survival Study Group (1994) Randomised
trial of cholesterol lowering in 4444 patients with coro-
nary heart disease. Lancet, 344, 1383-1389.
[3] Shepherd, J., Cobbe, S.M., Ford, I., et al. (1995) Preven-
tion of coronary heart disease with pravastatin in men
with hypercholesterolemia. West of Scotland Coronary
Prevention Study Group. New England Journal of Medi-
cine, 333, 1301-1307.
doi:10.1056/NEJM199511163332001
[4] The Long-Term Intervention with Pravastatin in Ischae-
mic Disease (LIPID) Study Group (1998) Prevention of
cardiovascular events and death with pravastatin in pa-
tients with coronary heart disease and a broad range of
initial cholesterol levels. New England Journal of Medi-
cine, 339, 1349-1357.
doi:10.1056/NEJM199811053391902
[5] Lewis, S.J., Sacks, F.M., Mitchell, J.S., et al. (1998) Ef-
fect of pravastatin on cardiovascular events in women af-
ter myocardial infarction: The cholesterol and recurrent
events (CARE) trial. Journal of the American College of
Cardiology, 32, 140-146.
doi:10.1016/S0735-1097(98)00202-2
[6] Gould, K.L., Ornish, D., Kirkeeide, R., et al. (1992) Im-
proved stenosis geometry by quantitative coronary arte-
riography after vigorous risk factor modification. Ameri-
can Journal of Cardiology, 69, 845-853.
doi:10.1016/0002-9149(92)90781-S
[7] Pitt, B., Waters, D., Brown, W.V., et al. (1999) Aggres-
Copyright © 2013 SciRes. OPEN ACCESS