Paper Menu >>
Journal Menu >>
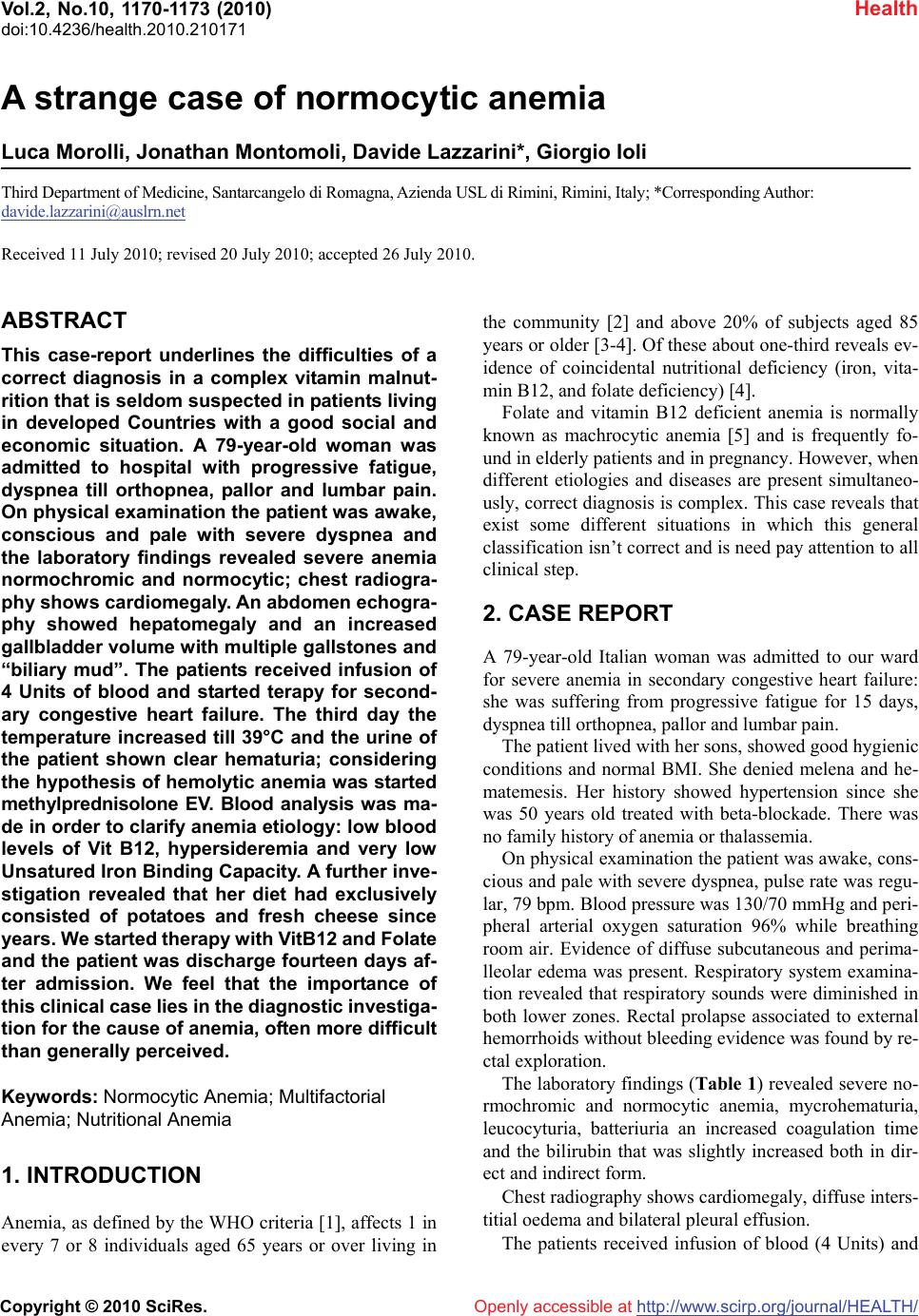 Vol.2, No.10, 1170-1173 (2010) Health doi:10.4236/health.2010.210171 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ A strange case of normocytic anemia Luca Morolli, Jonathan Montomoli, Davide Lazzarini*, Giorgio Ioli Third Department of Medicine, Santarcangelo di Romagna, Azienda USL di Rimini, Rimini, Italy; *Corresponding Author: davide.lazzarini@auslrn.net Received 11 July 2010; revised 20 July 2010; accepted 26 July 2010. ABSTRACT This case-report underlines the difficulties of a correct diagnosis in a complex vitamin malnut- rition that is seldom suspected in patients living in developed Countries with a good social and economic situation. A 79-year-old woman was admitted to hospital with progressive fatigue, dyspnea till orthopnea, pallor and lumbar pain. On physical examination the patient was awake, conscious and pale with severe dyspnea and the laboratory findings revealed severe anemia normochromic and normocytic; chest radiogra- phy shows cardiomegaly. An abdomen echogra- phy showed hepatomegaly and an increased gallbladder volume with multiple gallstones and “biliary mud”. The patients received infusion of 4 Units of blood and started terapy for second- ary congestive heart failure. The third day the temperature increased till 39°C and the urine of the patient shown clear hematuria; considering the hypothesis of hemolytic anemia was started methylprednisolone EV. Blood analysis was ma- de in order to clarify anemia etiology: low blood levels of Vit B12, hypersideremia and very low Unsatured Iron Binding Capacity. A further inve- stigation revealed that her diet had exclusively consisted of potatoes and fresh cheese since years. We started therapy with VitB12 and Folate and the patient was discharge fourteen days af- ter admission. We feel that the importance of this clinical case lies in the diagnostic investiga- tion for the cause of anemia, often more difficult than generally perceived. Keywords: Normocytic Anemia; Multifactorial Anemia; Nutritional Anemia 1. INTRODUCTION Anemia, as defined by the WHO criteria [1], affects 1 in every 7 or 8 individuals aged 65 years or over living in the community [2] and above 20% of subjects aged 85 years or older [3-4]. Of these about one-third reveals ev- idence of coincidental nutritional deficiency (iron, vita- min B12, and folate deficiency) [4]. Folate and vitamin B12 deficient anemia is normally known as machrocytic anemia [5] and is frequently fo- und in elderly patients and in pregnancy. However, when different etiologies and diseases are present simultaneo- usly, correct diagnosis is complex. This case reveals that exist some different situations in which this general classification isn’t correct and is need pay attention to all clinical step. 2. CASE REPORT A 79-year-old Italian woman was admitted to our ward for severe anemia in secondary congestive heart failure: she was suffering from progressive fatigue for 15 days, dyspnea till orthopnea, pallor and lumbar pain. The patient lived with her sons, showed good hygienic conditions and normal BMI. She denied melena and he- matemesis. Her history showed hypertension since she was 50 years old treated with beta-blockade. There was no family history of anemia or thalassemia. On physical examination the patient was awake, cons- cious and pale with severe dyspnea, pulse rate was regu- lar, 79 bpm. Blood pressure was 130/70 mmHg and peri- pheral arterial oxygen saturation 96% while breathing room air. Evidence of diffuse subcutaneous and perima- lleolar edema was present. Respiratory system examina- tion revealed that respiratory sounds were diminished in both lower zones. Rectal prolapse associated to external hemorrhoids without bleeding evidence was found by re- ctal exploration. The laboratory findings (Table 1) revealed severe no- rmochromic and normocytic anemia, mycrohematuria, leucocyturia, batteriuria an increased coagulation time and the bilirubin that was slightly increased both in dir- ect and indirect form. Chest radiography shows cardiomegaly, diffuse inters- titial oedema and bilateral pleural effusion. The patients received infusion of blood (4 Units) and  L. Morolli et al. / Health 2 (2010) 1170-1173 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 117 1171 started furosemide (20 mg EV/die), metoprolol (25 mg/ die) and Vit K (5 drops/die). After three days the patient getting physically better: oedema and dyspnea were improved, but blood cell cou- nt, bilirubin, platelets and kaliemia worsened (Table 2). Table 1. Blood test screening upon admission. Normal value WBC (109/l) Neu (%) Lyn (%) Mon (%) Eos (%) Bas (%) 7.49 78.0 16.8 3.7 1.5 0.0 4.00 – 10.00 RBC (1012/l) 1.52 4.00 – 5.20 Hb (g/dl) 4.1 12.0 – 15.5 Hct (%) 13.0 37.0 – 47.0 MCV (fl) 85.5 80.0 – 95.0 MCH (pg) 27.0 27.0 – 32.0 MCHC (g/dl) 31.5 32.0 – 36.0 PLT (109/L) 266 140 – 400 Glycaemia (mg/dl) 120 60 – 110 Total Bilirubin (mg/dl) 2.04 < 1.00 Direct Bilirubin (mg/dl) 0.87 < 0.30 AST/GOT (UI/l) 28 < 37 ALT/GPT (UI/l) 10 < 40 GGT (UI/l) 10 5 – 36 Serum Creatinine (mg/dl) 0.9 0.70 – 1.20 Serum Sodium (mEq/l) 138 135 – 146 Serum Potassium (mEq/l) 3.6 3.5 – 5.3 Serum Clorum (mEq/l) 106 98 – 110 Total serum Calcium (mg/dl) 7.7 8.6 – 10.2 Total Cholesterol (mg/dl) 53 < 200 HDL (mg/dl) 16 > 40 Triglyceride (mg/dl) 97 < 170 C-reactive protein CRP(mg/l) 2.1 < 5.0 Total serum Protein (g/l) 68 66 – 87 Protein Electrophoresis (%) Albumin Alfa 1 globulin Alfa 2 globulin Beta 1 globulin Beta 2 globulin Gamma globulin 58.1 4.1 6.8 5.5 5.1 20.4 55.8 – 66.1 2.9 – 4.9 7.1 – 11.8 4.7 – 7.2 3.2 – 6.5 11.1 – 18.8 TSH (mU/l) 1.34 0.270 – 4.200 CEA (ug/l) 1.96 < 4.0 CA 125 (KU/l) 12 < 35.0 Table 2. Blood test following appearance of oedema and dysp- nea. Normal value RBC (1012/L) 2.64 4.00 – 5.20 HB (g/dL) 8.4 12.0 – 15.5 PLT (109/L) 81 140 – 400 Total Bilirubin (mg/dL) 5.81 < 1.00 Direct Bilirubin (mg/dL) 2.23 < 0.30 Potassium (mEq/L) 2.7 3.5 – 5.3 During the afternoon of the third day a temperature ap- peared with shiver that increased during the night till 39°C and the urine of the patient showed clear hematuria. Hemocoltures were negative but urinocolture reveals urinary tract infection caused by E. Coli. Blood samples showed a decreasing of Hb (7 g/dl) and an increasing of PCR (33.3 mg/l -nv < 5-) and of LDH (2340 UI/l -nv 230/460-). Aptoglobin was normal (0.3 g/l -nv 0.30/2.00-). Considering the hypothesis of hemolytic anemia was also started a methylprednisolone 40 mg/die EV. An ab- domen echography showed hepatomegaly with dyshomo- geneous parenchyma, remarkable increase gallbladder volume with multiple gallstones and and “biliary mud”. Biliray tract wasn’t dilated, spleen, pancreas, kidneys, uterus and other genital organs were normal. Right pleu- ral effusion was confirmed at ultrasonography. Thorax-abdomen TC excluded thoracic, abdominal and pelvic masses and revealed discreet bilateral pleural ef- fusion, dilatation of cardiac cavities, gallbladder stones and calcification of aorta and renal artery. Patient refu- sed gastrointestinal endoscopy. Other blood analysis sh- owed an unexpected pattern (Table 3). In order to clarify the exact anemia etiology we re-co- llected the medical history and discovered that the patie- nt’s diet have exclusively consisted of potatoes and fresh cheese since years. We started therapy with VitB12 (1000 mg IM/die for a week), folate (1 injection/week for 3 months) and Pre- dnisone (0,5 mg/Kg/die) for 30 days then gradual taper- ing. Patient was discharge fourteen days after admission in fairly good condition with an appropriate home ther- apy. Table 4 shows laboratory analysis at the follow-up examination executed 2 years after the hospital dischar- ge. 3. DISCUSSION We consider this case report a good example of a multi- Table 3. Blood test prior to dismissal. Normal value Vit. B12 (ng/l) 52 197 – 866 Folate (ng/l) 2.59 3.1 – 17.5 PTH (ng/l) 85 10 – 75 Vit. D ng/ml < 7 fecal occult blood tests negative Negative Serum Fe (μg/dl) 239 40 – 145 Ferritin (ng/ml) 70 30 – 300 Total Iron Binding Capacity (μg/dl) 248 228 – 428 Unsatured Iron Binding Capacity (μg/dl) 9 150 – 340 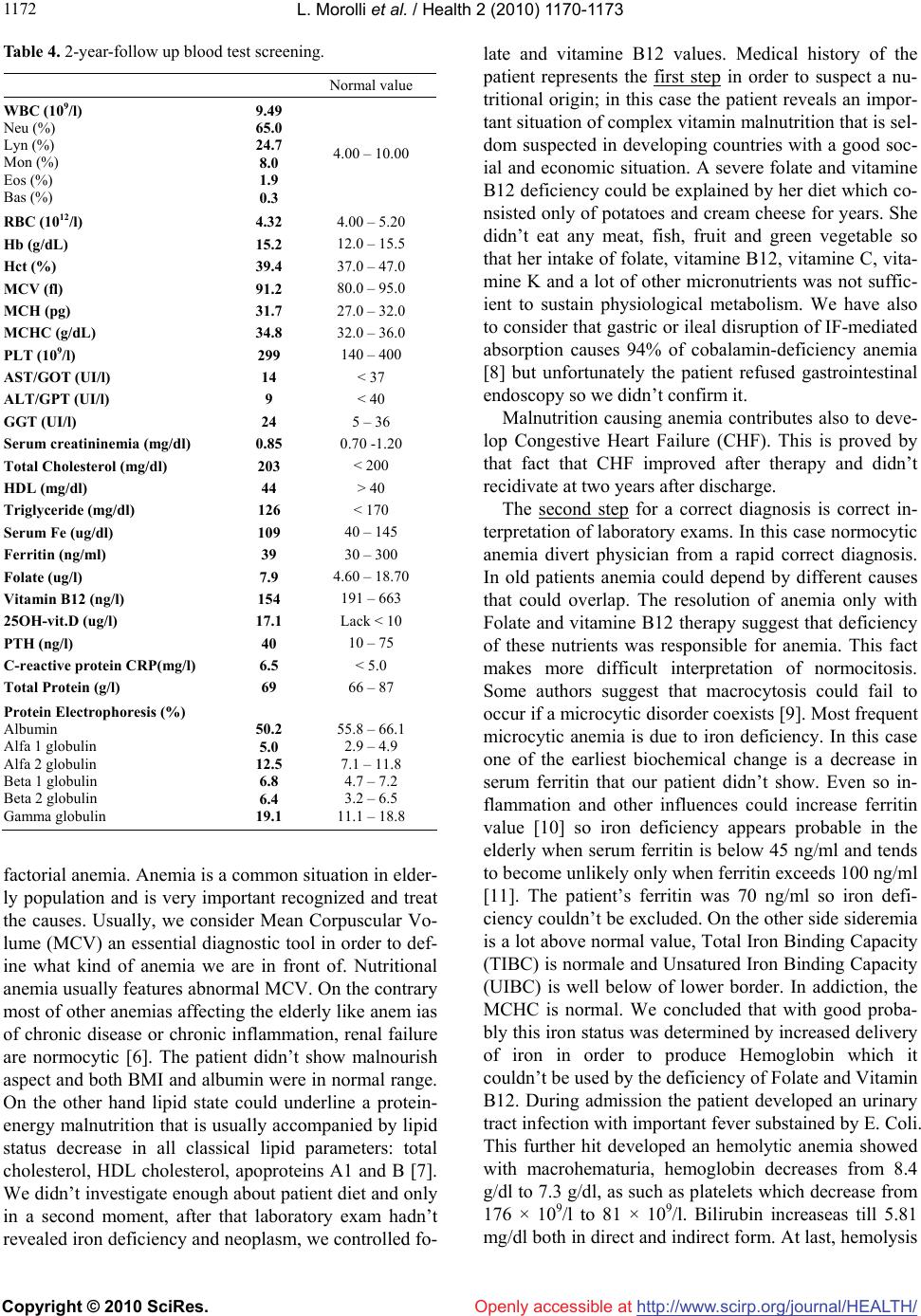 L. Morolli et al. / Health 2 (2010) 1170-1173 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 1172 Table 4. 2-year-follow up blood test screening. Normal value WBC (109/l) Neu (%) Lyn (%) Mon (%) Eos (%) Bas (%) 9.49 65.0 24.7 8.0 1.9 0.3 4.00 – 10.00 RBC (1012/l) 4.32 4.00 – 5.20 Hb (g/dL) 15.2 12.0 – 15.5 Hct (%) 39.4 37.0 – 47.0 MCV (fl) 91.2 80.0 – 95.0 MCH (pg) 31.7 27.0 – 32.0 MCHC (g/dL) 34.8 32.0 – 36.0 PLT (109/l) 299 140 – 400 AST/GOT (UI/l) 14 < 37 ALT/GPT (UI/l) 9 < 40 GGT (UI/l) 24 5 – 36 Serum creatininemia (mg/dl) 0.85 0.70 -1.20 Total Cholesterol (mg/dl) 203 < 200 HDL (mg/dl) 44 > 40 Triglyceride (mg/dl) 126 < 170 Serum Fe (ug/dl) 109 40 – 145 Ferritin (ng/ml) 39 30 – 300 Folate (ug/l) 7.9 4.60 – 18.70 Vitamin B12 (ng/l) 154 191 – 663 25OH-vit.D (ug/l) 17.1 Lack < 10 PTH (ng/l) 40 10 – 75 C-reactive protein CRP(mg/l) 6.5 < 5.0 Total Protein (g/l) 69 66 – 87 Protein Electrophoresis (%) Albumin Alfa 1 globulin Alfa 2 globulin Beta 1 globulin Beta 2 globulin Gamma globulin 50.2 5.0 12.5 6.8 6.4 19.1 55.8 – 66.1 2.9 – 4.9 7.1 – 11.8 4.7 – 7.2 3.2 – 6.5 11.1 – 18.8 factorial anemia. Anemia is a common situation in elder- ly population and is very important recognized and treat the causes. Usually, we consider Mean Corpuscular Vo- lume (MCV) an essential diagnostic tool in order to def- ine what kind of anemia we are in front of. Nutritional anemia usually features abnormal MCV. On the contrary most of other anemias affecting the elderly like anem ias of chronic disease or chronic inflammation, renal failure are normocytic [6]. The patient didn’t show malnourish aspect and both BMI and albumin were in normal range. On the other hand lipid state could underline a protein- energy malnutrition that is usually accompanied by lipid status decrease in all classical lipid parameters: total cholesterol, HDL cholesterol, apoproteins A1 and B [7]. We didn’t investigate enough about patient diet and only in a second moment, after that laboratory exam hadn’t revealed iron deficiency and neoplasm, we controlled fo- late and vitamine B12 values. Medical history of the patient represents the first step in order to suspect a nu- tritional origin; in this case the patient reveals an impor- tant situation of complex vitamin malnutrition that is sel- dom suspected in developing countries with a good soc- ial and economic situation. A severe folate and vitamine B12 deficiency could be explained by her diet which co- nsisted only of potatoes and cream cheese for years. She didn’t eat any meat, fish, fruit and green vegetable so that her intake of folate, vitamine B12, vitamine C, vita- mine K and a lot of other micronutrients was not suffic- ient to sustain physiological metabolism. We have also to consider that gastric or ileal disruption of IF-mediated absorption causes 94% of cobalamin-deficiency anemia [8] but unfortunately the patient refused gastrointestinal endoscopy so we didn’t confirm it. Malnutrition causing anemia contributes also to deve- lop Congestive Heart Failure (CHF). This is proved by that fact that CHF improved after therapy and didn’t recidivate at two years after discharge. The second step for a correct diagnosis is correct in- terpretation of laboratory exams. In this case normocytic anemia divert physician from a rapid correct diagnosis. In old patients anemia could depend by different causes that could overlap. The resolution of anemia only with Folate and vitamine B12 therapy suggest that deficiency of these nutrients was responsible for anemia. This fact makes more difficult interpretation of normocitosis. Some authors suggest that macrocytosis could fail to occur if a microcytic disorder coexists [9]. Most frequent microcytic anemia is due to iron deficiency. In this case one of the earliest biochemical change is a decrease in serum ferritin that our patient didn’t show. Even so in- flammation and other influences could increase ferritin value [10] so iron deficiency appears probable in the elderly when serum ferritin is below 45 ng/ml and tends to become unlikely only when ferritin exceeds 100 ng/ml [11]. The patient’s ferritin was 70 ng/ml so iron defi- ciency couldn’t be excluded. On the other side sideremia is a lot above normal value, Total Iron Binding Capacity (TIBC) is normale and Unsatured Iron Binding Capacity (UIBC) is well below of lower border. In addiction, the MCHC is normal. We concluded that with good proba- bly this iron status was determined by increased delivery of iron in order to produce Hemoglobin which it couldn’t be used by the deficiency of Folate and Vitamin B12. During admission the patient developed an urinary tract infection with important fever substained by E. Coli. This further hit developed an hemolytic anemia showed with macrohematuria, hemoglobin decreases from 8.4 g/dl to 7.3 g/dl, as such as platelets which decrease from 176 × 109/l to 81 × 109/l. Bilirubin increaseas till 5.81 mg/dl both in direct and indirect form. At last, hemolysis  L. Morolli et al. / Health 2 (2010) 1170-1173 Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/ 117 1173 was confirmed by increase of inflammatory indexes like C-reactive protein (CRP), LDH and by low value of ap- toglobin. REFERENCES [1] Blanc, B., Finch, C.A., Hallberg, L., et al. (1968) Nutri- tional anaemias: Report of a WHO scientific group. WHO Technical Report Series, 405, 1-40. [2] Endres, H.G., Wedding, U., Pittrow, D., Thiem, U., Trampisch, H.J. and Diehm, C. (2009) Prevalence of anemia in elderly patients in primary care: Impact on 5-year mortality risk and differences between men and women. Current Medical Research and Opinion, 25(5), 1143-1158. [3] Beghé, C., Wilson, A. and Ershler, W.B. (2004) Preva- lence and outcomes of anemia in geriatrics. American Journal of Medicine, 116(Suppl. 7A), S3-S10. [4] Guralnik, J.M., Eisenstaedt, R.S., Ferrucci, L., Klein, H.G. and Woodman, R.C. (2004) Prevalence of anemia in persons 65 years and older in the United States: Evi- dence for a high rate of unexplained anemia. Blood, 104(8), 2263-2268. [5] Megaloblastic anemias. In: Fauci, Braunwald, Kasper, Hauser, Longo, Jameson, Loscalzo, Eds., Harrison’s Pr- inciples of Internal Medicine, 17th Edition, Mc Graw- Hill Medical Publishing Division, New York. [6] Carmel, R. (2008) Nutritional anemias and the eldery. Semin Hematol, 45(4), 225-234. [7] Monarque-Favard, C., Garcia, I., Abidi, H., Bannier, E., Riviere, J., Drai, J. and Bonnefoy, M. (2002) Malnour- ished elderly people and lipid status. Journal of Nutrition, Health & Aging, 6(6), 370-374. [8] Savage, D.G., Lindenbaum, J., Stabler, S.P. and Allen, R.H. (1994) Sensitivity of serum methylmalonic acid and total homocysteine determinations for diagnosing co- balamin and folate deficiencies. American Journal of Medicine, 96(3), 239-246. [9] Chan, C.W., Liu, S.Y., Kho, C.S., Lau, K.H., Liang, Y.S., Chu, W.R. and Ma, S.K. (2007) Diagnostic clues to megaloblastic anaemia without macrocytosis. Interna- tional Journal of Laboratory Hematology, 29(3), 163- 171. [10] Beutler, E. (2006) Disorders of iron metabolism. In: Lichtman, M.A., Beutler, E., Kipps, T.J., Selingsohn, U., Kaushansky, K. and Prchal, J.T., Eds., Williams Hema- tology, 7th Edition, McGraw-Hill, New York. [11] Guyatt, G.H., Patterson, C., Ali, M., Singer, J., Levine, M., Turpie, I. and Meyer, R. (1990) Diagnosis of iron- deficiency anemia in the elderly. American Journal of Medicine, 88(3), 205-209. |

