Paper Menu >>
Journal Menu >>
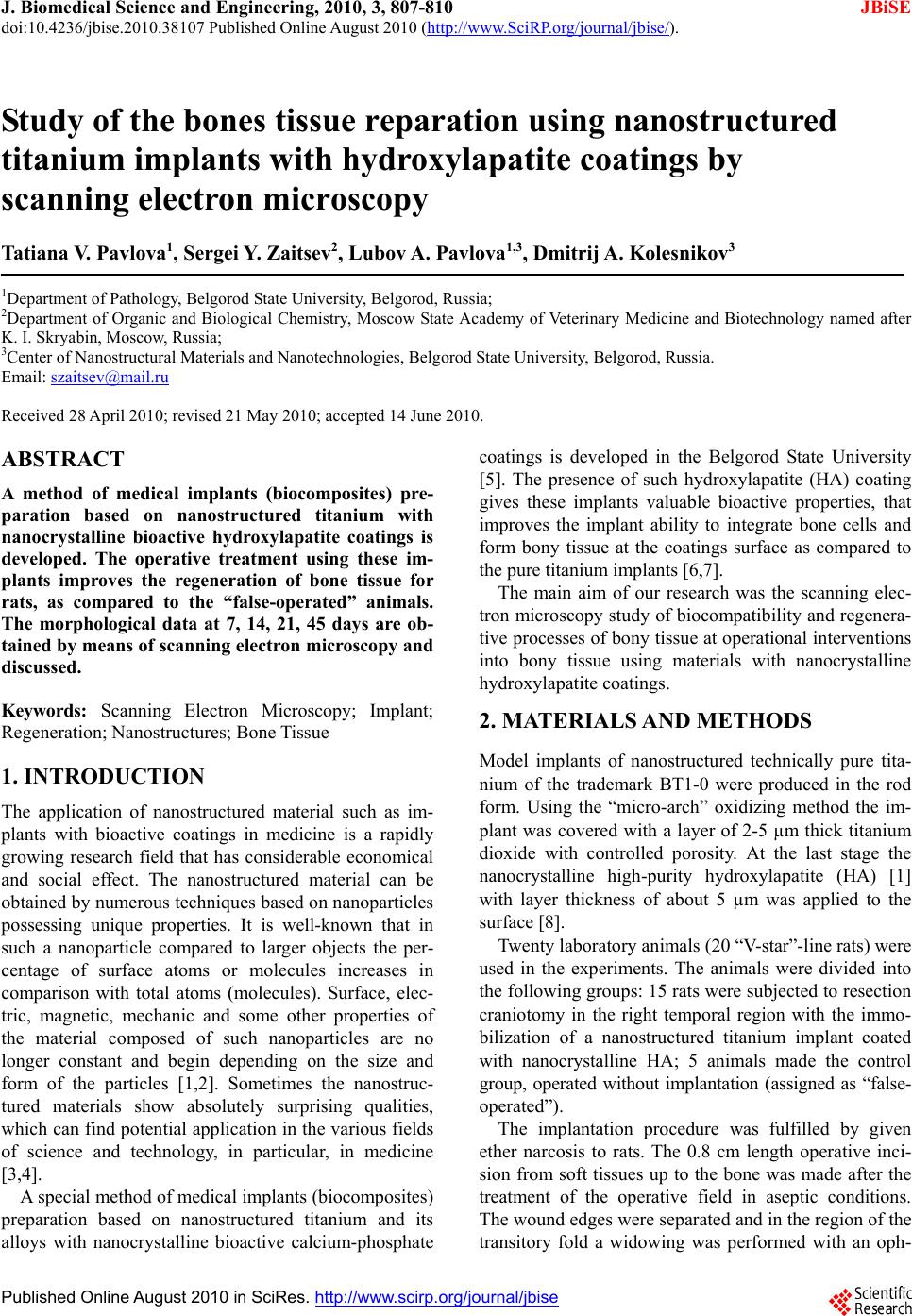 J. Biomedical Science and Engineering, 2010, 3, 807-810 JBiSE doi:10.4236/jbise.2010.38107 Published Online August 2010 (http://www.SciRP.org/journal/jbise/). Published Online August 2010 in SciRes. http:// www. scirp. org/journal/jbise Study of the bones tissue reparation using nanostructured titanium implants with hydroxylapatite coatings by scanning electron microscopy Tatian a V. Pavlova1, Sergei Y. Zaitsev2, Lubov A. Pavlova1,3, Dmitrij A. Kolesnikov3 1Department of Pathology, Belgorod State University, Belgorod, Russia; 2Department of Organic and Biological Chemistry, Moscow State Academy of Veterinary Medicine and Biotechnology named after K. I. Skryabin, Moscow, Russia; 3Center of Nanostructural Materials and Nanotechnologies, Belgorod State University, Belgorod, Russia. Email: szaitsev@mail.ru Received 28 April 2010; revised 21 May 2010; accepted 14 June 2010. ABSTRACT A method of medical implants (biocomposites) pre- paration based on nanostructured titanium with nanocrystalline bioactive hydroxylapatite coatings is developed. The operative treatment using these im- plants improves the regeneration of bone tissue for rats, as compared to the “false-operated” animals. The morphological data at 7, 14, 21, 45 days are ob- tained by means of scanning electron microscopy and discussed. Keywords: Scanning Electron Microscopy; Implant; Regeneration; Nan ost r uctu res ; Bone Tissue 1. INTRODUCTION The application of nanostructured material such as im- plants with bioactive coatings in medicine is a rapidly growing research field that has considerable economical and social effect. The nanostructured material can be obtained by numerous techniques based on nanoparticles possessing unique properties. It is well-known that in such a nanoparticle compared to larger objects the per- centage of surface atoms or molecules increases in comparison with total atoms (molecules). Surface, elec- tric, magnetic, mechanic and some other properties of the material composed of such nanoparticles are no longer constant and begin depending on the size and form of the particles [1,2]. Sometimes the nanostruc- tured materials show absolutely surprising qualities, which can find potential applicatio n in the various fields of science and technology, in particular, in medicine [3,4]. A special method of medical implants (biocomposites) preparation based on nanostructured titanium and its alloys with nanocrystalline bioactive calcium-phosphate coatings is developed in the Belgorod State University [5]. The presence of such hydroxylapatite (HA) coating gives these implants valuable bioactive properties, that improves the implant ability to integrate bone cells and form bony tissue at the coatings surface as compared to the pure titanium implants [6,7]. The main aim of our research was the scanning elec- tron microscopy study of biocompatibility and regenera- tive processes of bony tissue at op erational interventions into bony tissue using materials with nanocrystalline hydroxylapatite coatings. 2. MATERIALS AND METHODS Model implants of nanostructured technically pure tita- nium of the trademark BT1-0 were produced in the rod form. Using the “micro-arch” oxidizing method the im- plant was covered with a layer of 2-5 µm thick titanium dioxide with controlled porosity. At the last stage the nanocrystalline high-purity hydroxylapatite (HA) [1] with layer thickness of about 5 µm was applied to the surface [8]. Twenty laboratory animals (20 “V-star”-line rats) were used in the experiments. The animals were divided into the following groups: 15 rats were subjected to resection craniotomy in the right temporal region with the immo- bilization of a nanostructured titanium implant coated with nanocrystalline HA; 5 animals made the control group, operated without implantation (assigned as “false- operated”). The implantation procedure was fulfilled by given ether narcosis to rats. The 0.8 cm length operative inci- sion from soft tissues up to the bone was made after the treatment of the operative field in aseptic conditions. The wound edges were separated and in the region of the transitory fold a widowing was performed with an oph- 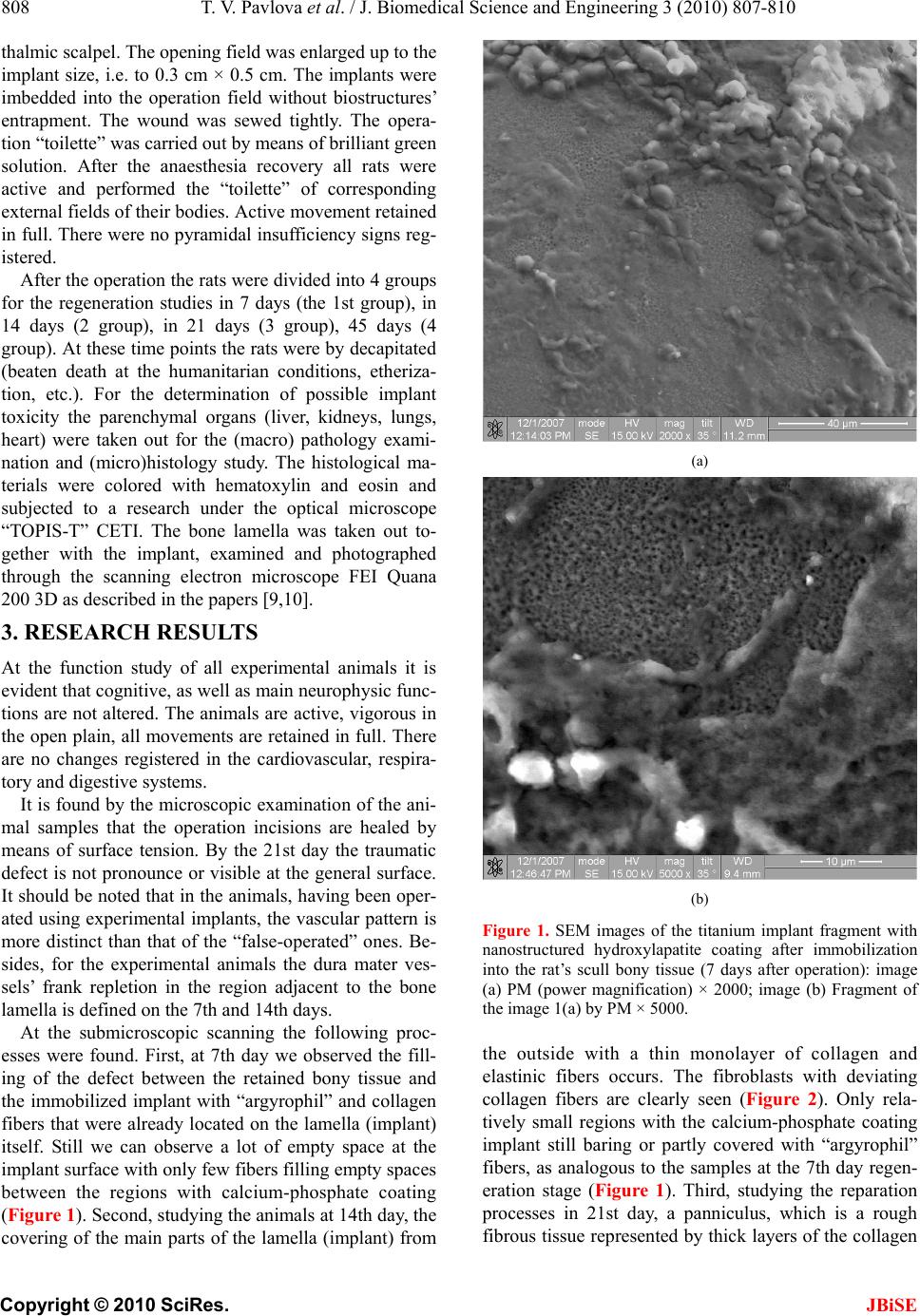 808 T. V. Pavlova et al. / J. Biomedical Science and Engineering 3 (2010) 807-810 Copyright © 2010 SciRes. JBiSE thalmic scalpel. The opening field was enlarged up to the implant size, i.e. to 0.3 cm × 0.5 cm. The implants were imbedded into the operation field without biostructures’ entrapment. The wound was sewed tightly. The opera- tion “toilette” was carried out by means of brilliant green solution. After the anaesthesia recovery all rats were active and performed the “toilette” of corresponding external fields of their bodies. Active movement retained in full. There were no pyramidal insufficiency signs reg- istered. After the operation the rats were divided into 4 groups for the regeneration studies in 7 days (the 1st group), in 14 days (2 group), in 21 days (3 group), 45 days (4 group). At these time points the rats were by decapitated (beaten death at the humanitarian conditions, etheriza- tion, etc.). For the determination of possible implant toxicity the parenchymal organs (liver, kidneys, lungs, heart) were taken out for the (macro) pathology exami- nation and (micro)histology study. The histological ma- terials were colored with hematoxylin and eosin and subjected to a research under the optical microscope “TOPIS-T” CETI. The bone lamella was taken out to- gether with the implant, examined and photographed through the scanning electron microscope FEI Quana 200 3D as described in the papers [9,10]. 3. RESEARCH RESULTS At the function study of all experimental animals it is evident that cog nitive, as well as main neuroph ysic func- tions are not altered. The animals are active, vigorous in the open plain, all movements are retained in full. There are no changes registered in the cardiovascular, respira- tory and digestive systems. It is found by the microscopic examination of the ani- mal samples that the operation incisions are healed by means of surface tension. By the 21st day the traumatic defect is not pronounce or visible at the general surface. It should be noted that in the animals, having been oper- ated using experimental implants, the vascular pattern is more distinct than that of the “false-operated” ones. Be- sides, for the experimental animals the dura mater ves- sels’ frank repletion in the region adjacent to the bone lamella is defined on the 7th and 14th days. At the submicroscopic scanning the following proc- esses were found. First, at 7th day we observed the fill- ing of the defect between the retained bony tissue and the immobilized implant with “argyrophil” and collagen fibers that were already located on the lamella (implant) itself. Still we can observe a lot of empty space at the implant surface with only few fibers filling empty spaces between the regions with calcium-phosphate coating (Figure 1). Second, studying the animals at 14th day, the covering of the main parts of the lamella (implant) from (a) (b) Figure 1. SEM images of the titanium implant fragment with nanostructured hydroxylapatite coating after immobilization into the rat’s scull bony tissue (7 days after operation): image (a) PM (power magnification) × 2000; image (b) Fragment of the image 1(a) by PM × 5000. the outside with a thin monolayer of collagen and elastinic fibers occurs. The fibroblasts with deviating collagen fibers are clearly seen (Figure 2). Only rela- tively small regions with the calcium-phosphate coating implant still baring or partly covered with “argyrophil” fibers, as analogous to the samples at the 7th day regen- eration stage (Figure 1). Third, studying the reparation processes in 21st day, a panniculus, which is a rough fibrous tissue represen ted by thick layers of the collagen 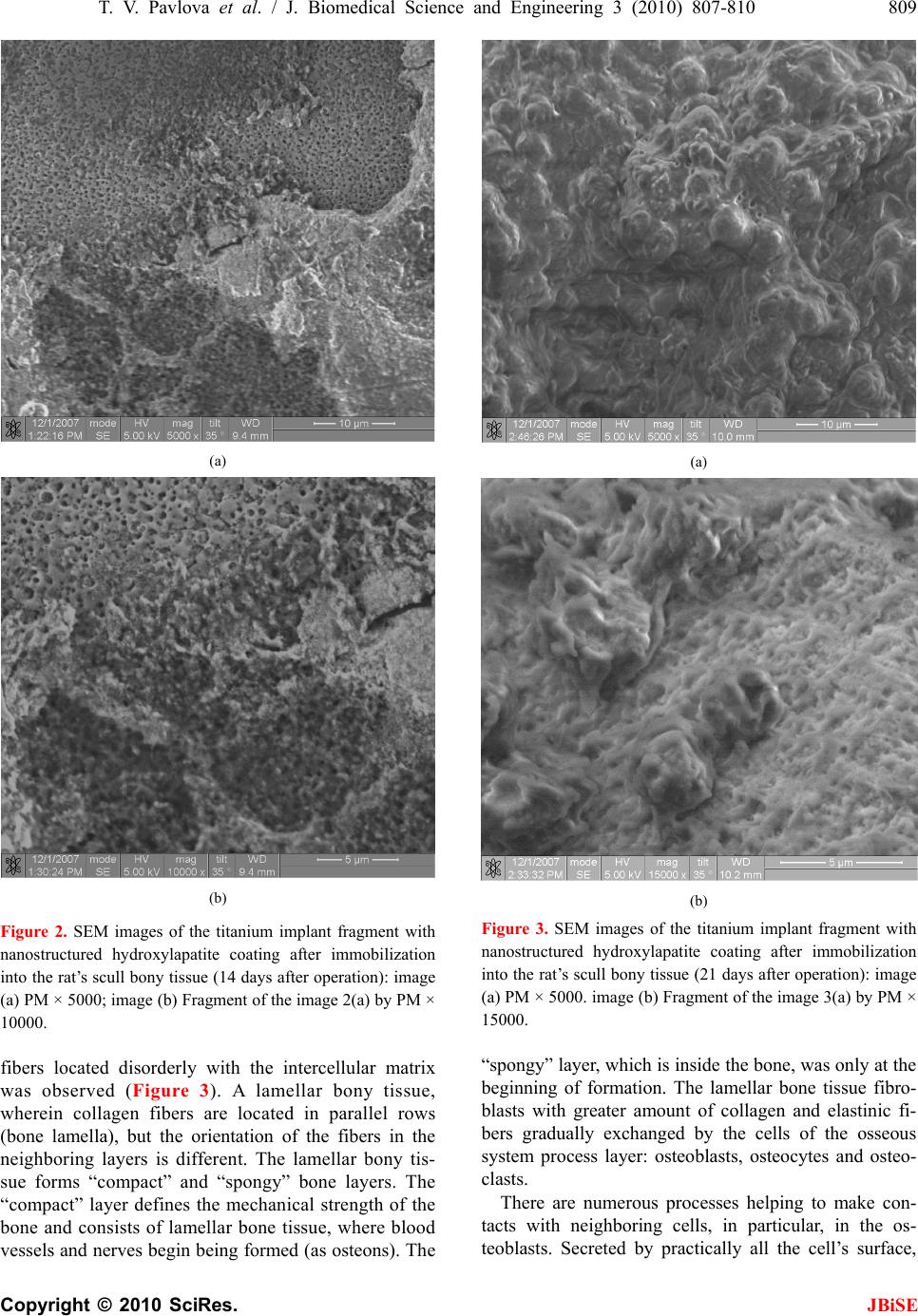 T. V. Pavlova et al. / J. Biomedical Science and Engineering 3 (2010) 807-810 809 Copyright © 2010 SciRes. JBiSE (a) (b) Figure 2. SEM images of the titanium implant fragment with nanostructured hydroxylapatite coating after immobilization into the rat’s scull bony tissue (14 days after operation): image (a) PM × 5000; image (b) Fragment of the image 2(a) by PM × 10000. fibers located disorderly with the intercellular matrix was observed (Figure 3). A lamellar bony tissue, wherein collagen fibers are located in parallel rows (bone lamella), but the orientation of the fibers in the neighboring layers is different. The lamellar bony tis- sue forms “compact” and “spongy” bone layers. The “compact” layer defines the mechanical strength of the bone and consists of lamellar bone tissue, where blood vessels and nerves begin being formed (as osteons). The (a) (b) Figure 3. SEM images of the titanium implant fragment with nanostructured hydroxylapatite coating after immobilization into the rat’s scull bony tissue (21 days after operation): image (a) PM × 5000. image (b) Fragment of the image 3(a) by PM × 15000. “spongy” layer, which is inside the b one, was on ly at the beginning of formation. The lamellar bone tissue fibro- blasts with greater amount of collagen and elastinic fi- bers gradually exchanged by the cells of the osseous system process layer: osteoblasts, osteocytes and osteo- clasts. There are numerous processes helping to make con- tacts with neighboring cells, in particular, in the os- teoblasts. Secreted by practically all the cell’s surface, 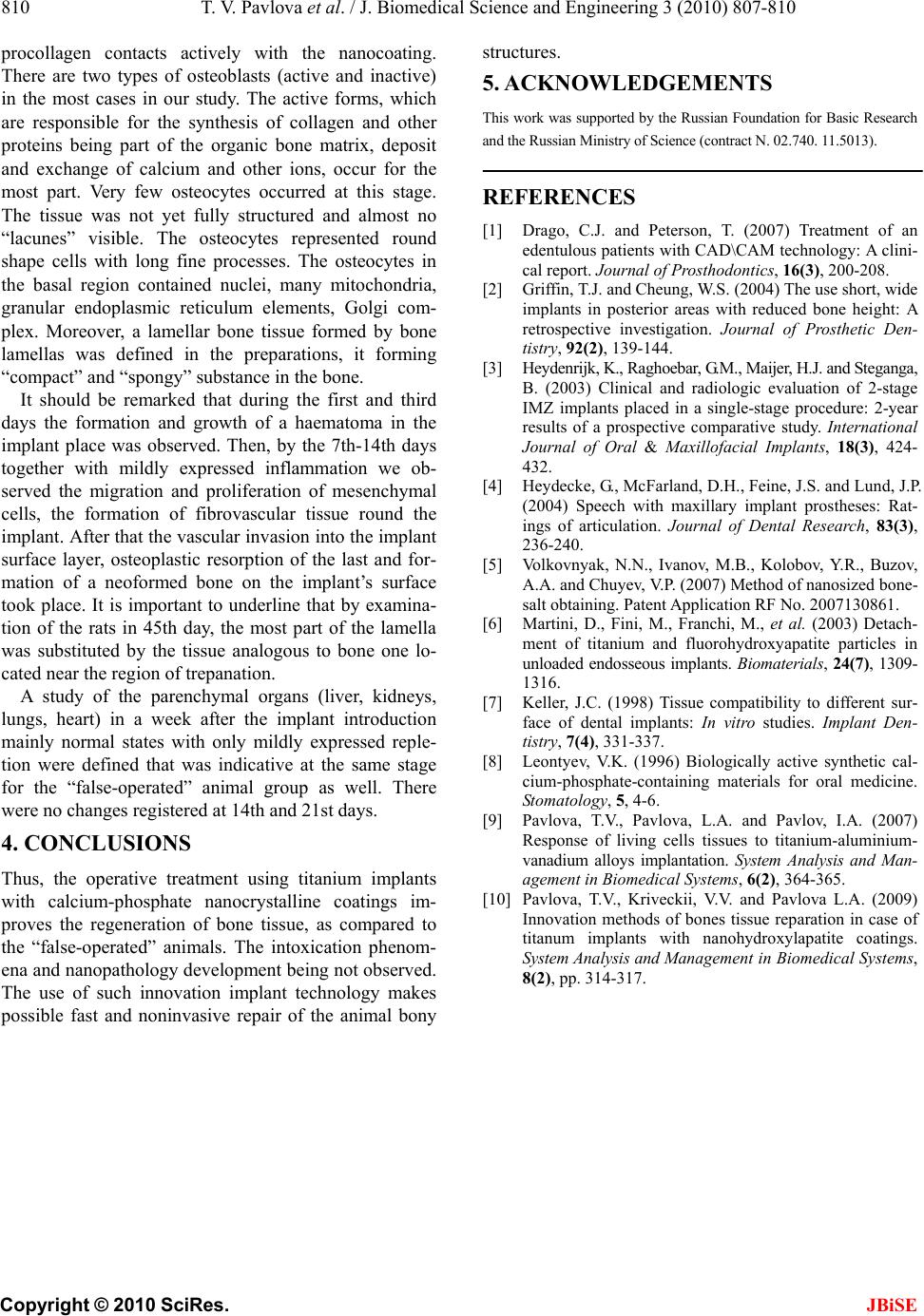 810 T. V. Pavlova et al. / J. Biomedical Science and Engineering 3 (2010) 807-810 Copyright © 2010 SciRes. JBiSE procollagen contacts actively with the nanocoating. There are two types of osteoblasts (active and inactive) in the most cases in our study. The active forms, which are responsible for the synthesis of collagen and other proteins being part of the organic bone matrix, deposit and exchange of calcium and other ions, occur for the most part. Very few osteocytes occurred at this stage. The tissue was not yet fully structured and almost no “lacunes” visible. The osteocytes represented round shape cells with long fine processes. The osteocytes in the basal region contained nuclei, many mitochondria, granular endoplasmic reticulum elements, Golgi com- plex. Moreover, a lamellar bone tissue formed by bone lamellas was defined in the preparations, it forming “compact” and “spongy” substance in the bone. It should be remarked that during the first and third days the formation and growth of a haematoma in the implant place was observed. Then, by the 7th-14th days together with mildly expressed inflammation we ob- served the migration and proliferation of mesenchymal cells, the formation of fibrovascular tissue round the implant. After that the vascular invasion into the implant surface layer, osteoplastic resorption of the last and for- mation of a neoformed bone on the implant’s surface took place. It is important to underline that by examina- tion of the rats in 45th day, the most part of the lamella was substituted by the tissue analogous to bone one lo- cated near the region of trepanation. A study of the parenchymal organs (liver, kidneys, lungs, heart) in a week after the implant introduction mainly normal states with only mildly expressed reple- tion were defined that was indicative at the same stage for the “false-operated” animal group as well. There were no changes registered at 14th and 21st days. 4. CONCLUSIONS Thus, the operative treatment using titanium implants with calcium-phosphate nanocrystalline coatings im- proves the regeneration of bone tissue, as compared to the “false-operated” animals. The intoxication phenom- ena and nanopathology development being not observed. The use of such innovation implant technology makes possible fast and noninvasive repair of the animal bony structures. 5. ACKNOWLEDGEMENTS This work was supported by the Rus sian Foundation for Basic R esearch and the Russian Ministry of Science (contract N. 02.740. 11. 5013). REFERENCES [1] Drago, C.J. and Peterson, T. (2007) Treatment of an edentulous patients with CAD\CAM technology: A clini- cal report. Journal of Prosthodontics, 16(3), 200-208. [2] Griffin, T.J. and Cheung, W.S. (2004) The use short, wide implants in posterior areas with reduced bone height: A retrospective investigation. Journal of Prosthetic Den- tistry, 92(2), 139-144. [3] Heydenrijk, K., Raghoebar, G. M., Maijer, H.J. and Steganga, B. (2003) Clinical and radiologic evaluation of 2-stage IMZ implants placed in a single-stage procedure: 2-year results of a prospective comparative study. International Journal of Oral & Maxillofacial Implants, 18(3), 424- 432. [4] Heydecke, G., McFarland, D.H., Feine, J.S. and Lund, J.P. (2004) Speech with maxillary implant prostheses: Rat- ings of articulation. Journal of Dental Research, 83(3), 236-240. [5] Volkovnyak, N.N., Ivanov, M.B., Kolobov, Y.R., Buzov, A.A. and Chuyev, V.P. (2007) Method of nanosized bone- salt obtaining. Patent Application RF No. 2007130861. [6] Martini, D., Fini, M., Franchi, M., et al. (2003) Detach- ment of titanium and fluorohydroxyapatite particles in unloaded endosseous implants. Biomaterials, 24(7), 1309- 1316. [7] Keller, J.C. (1998) Tissue compatibility to different sur- face of dental implants: In vitro studies. Implant Den- tistry, 7(4), 331-337. [8] Leontyev, V.K. (1996) Biologically active synthetic cal- cium-phosphate-containing materials for oral medicine. Stomatology, 5, 4-6. [9] Pavlova, T.V., Pavlova, L.A. and Pavlov, I.A. (2007) Response of living cells tissues to titanium-aluminium- vanadium alloys implantation. System Analysis and Man- agement in Biomedical Systems, 6(2), 364-365. [10] Pavlova, T.V., Kriveckii, V.V. and Pavlova L.A. (2009) Innovation methods of bones tissue reparation in case of titanum implants with nanohydroxylapatite coatings. System Analysis and Manag em en t in Bi ome di ca l S yst em s, 8(2), pp. 314-317. |

