Assessing Injection Techniques in the Treatment of Trigger Finger 85
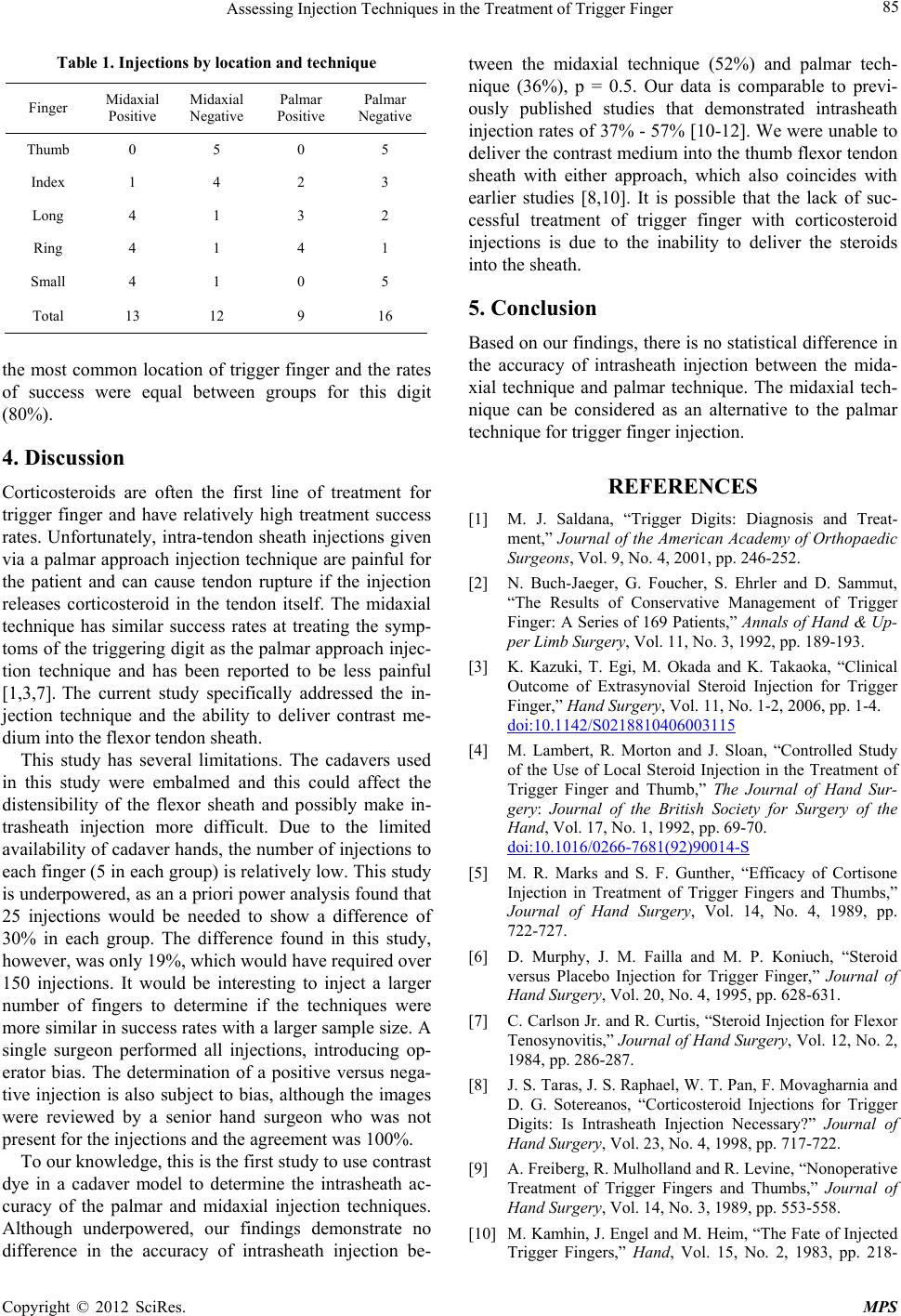
Table 1. Injections by loca tion and technique
Finger Midaxial
Positive Midaxial
Negative Palmar
Positive Palmar
Negative
Thumb 0 5 0 5
Index 1 4 2 3
Long 4 1 3 2
Ring 4 1 4 1
Small 4 1 0 5
Total 13 12 9 16
the most common location of trigger finger and the rates
of success were equal between groups for this digit
(80%).
4. Discussion
Corticosteroids are often the first line of treatment for
trigger finger and have relatively high treatment success
rates. Unfortunately, intra-tendon sheath injections given
via a palmar approach injection technique are painful for
the patient and can cause tendon rupture if the injection
releases corticosteroid in the tendon itself. The midaxial
technique has similar success rates at treating the symp-
toms of the triggering d igit as the palmar approach injec-
tion technique and has been reported to be less painful
[1,3,7]. The current study specifically addressed the in-
jection technique and the ability to deliver contrast me-
dium into the flexor tendo n sheath.
This study has several limitations. The cadavers used
in this study were embalmed and this could affect the
distensibility of the flexor sheath and possibly make in-
trasheath injection more difficult. Due to the limited
availability of cadaver hand s, the number of injections to
each finger (5 in each group) is relatively low. This study
is underpowered, as an a priori power analysis found that
25 injections would be needed to show a difference of
30% in each group. The difference found in this study,
however, was only 19%, which would have required over
150 injections. It would be interesting to inject a larger
number of fingers to determine if the techniques were
more similar in success rates with a larger sample size. A
single surgeon performed all injections, introducing op-
erator bias. The determination of a positive versus nega-
tive injection is also subject to bias, although the images
were reviewed by a senior hand surgeon who was not
present for the injections and the agreement was 100%.
To our knowledge, this is the first study to use contrast
dye in a cadaver model to determine the intrasheath ac-
curacy of the palmar and midaxial injection techniques.
Although underpowered, our findings demonstrate no
difference in the accuracy of intrasheath injection be-
tween the midaxial technique (52%) and palmar tech-
nique (36%), p = 0.5. Our data is comparable to previ-
ously published studies that demonstrated intrasheath
injection rates of 37% - 57% [10-12]. We were unable to
deliver the contrast medium into the thumb flexor tendon
sheath with either approach, which also coincides with
earlier studies [8,10]. It is possible that the lack of suc-
cessful treatment of trigger finger with corticosteroid
injections is due to the inability to deliver the steroids
into the sheath.
5. Conclusion
Based on our findings, there is no statistical difference in
the accuracy of intrasheath injection between the mida-
xial technique and palmar technique. The midaxial tech-
nique can be considered as an alternative to the palmar
technique for trigger finger injection.
REFERENCES
[1] M. J. Saldana, “Trigger Digits: Diagnosis and Treat-
ment,” Journal of the American Academy of Orthopaedic
Surgeons, Vol. 9, No. 4, 2001, pp. 246-252.
[2] N. Buch-Jaeger, G. Foucher, S. Ehrler and D. Sammut,
“The Results of Conservative Management of Trigger
Finger: A Series of 169 Patients,” Annals of Hand & Up-
per Limb Surgery, Vol. 11, No. 3, 1992, pp. 189-193.
[3] K. Kazuki, T. Egi, M. Okada and K. Takaoka, “Clinical
Outcome of Extrasynovial Steroid Injection for Trigger
Finger,” Hand Surgery, Vol. 11, No. 1-2, 2006, pp. 1-4.
doi:10.1142/S0218810406003115
[4] M. Lambert, R. Morton and J. Sloan, “Controlled Study
of the Use of Local Steroid Injection in the Treatment of
Trigger Finger and Thumb,” The Journal of Hand Sur-
gery: Journal of the British Society for Surgery of the
Hand, Vol. 17, No. 1, 1992, pp. 69-70.
doi:10.1016/0266-7681(92)90014-S
[5] M. R. Marks and S. F. Gunther, “Efficacy of Cortisone
Injection in Treatment of Trigger Fingers and Thumbs,”
Journal of Hand Surgery, Vol. 14, No. 4, 1989, pp.
722-727.
[6] D. Murphy, J. M. Failla and M. P. Koniuch, “Steroid
versus Placebo Injection for Trigger Finger,” Journal of
Hand Surgery, Vol. 20, No. 4, 1995, pp. 628-631.
[7] C. Carlson Jr. and R. Curtis, “Steroid Injection for Flexor
Tenosynovitis,” Journal of Hand Surgery, Vol. 12, No. 2,
1984, pp. 286-287.
[8] J. S. Taras, J. S. Rapha el, W. T. Pan, F. Movagharnia and
D. G. Sotereanos, “Corticosteroid Injections for Trigger
Digits: Is Intrasheath Injection Necessary?” Journal of
Hand Surgery, Vol. 23, No. 4, 1998, pp. 717-722.
[9] A. Freiberg, R. Mulholland and R. Levine, “Nonoperative
Treatment of Trigger Fingers and Thumbs,” Journal of
Hand Surgery, Vol. 14, No. 3, 1989, pp. 553-558.
[10] M. Kamhin, J. Engel and M. Heim, “The Fate of Injected
Trigger Fingers,” Hand, Vol. 15, No. 2, 1983, pp. 218-
Copyright © 2012 SciRes. MPS