F. PORZSOLT ET AL.
Acad.
teaching
and CME
Real world
outcomes
Clinical
guidelines
Health care
expenditure
Clinical
practice
Approval of
innovation
Clinical
research
Publication
of the results
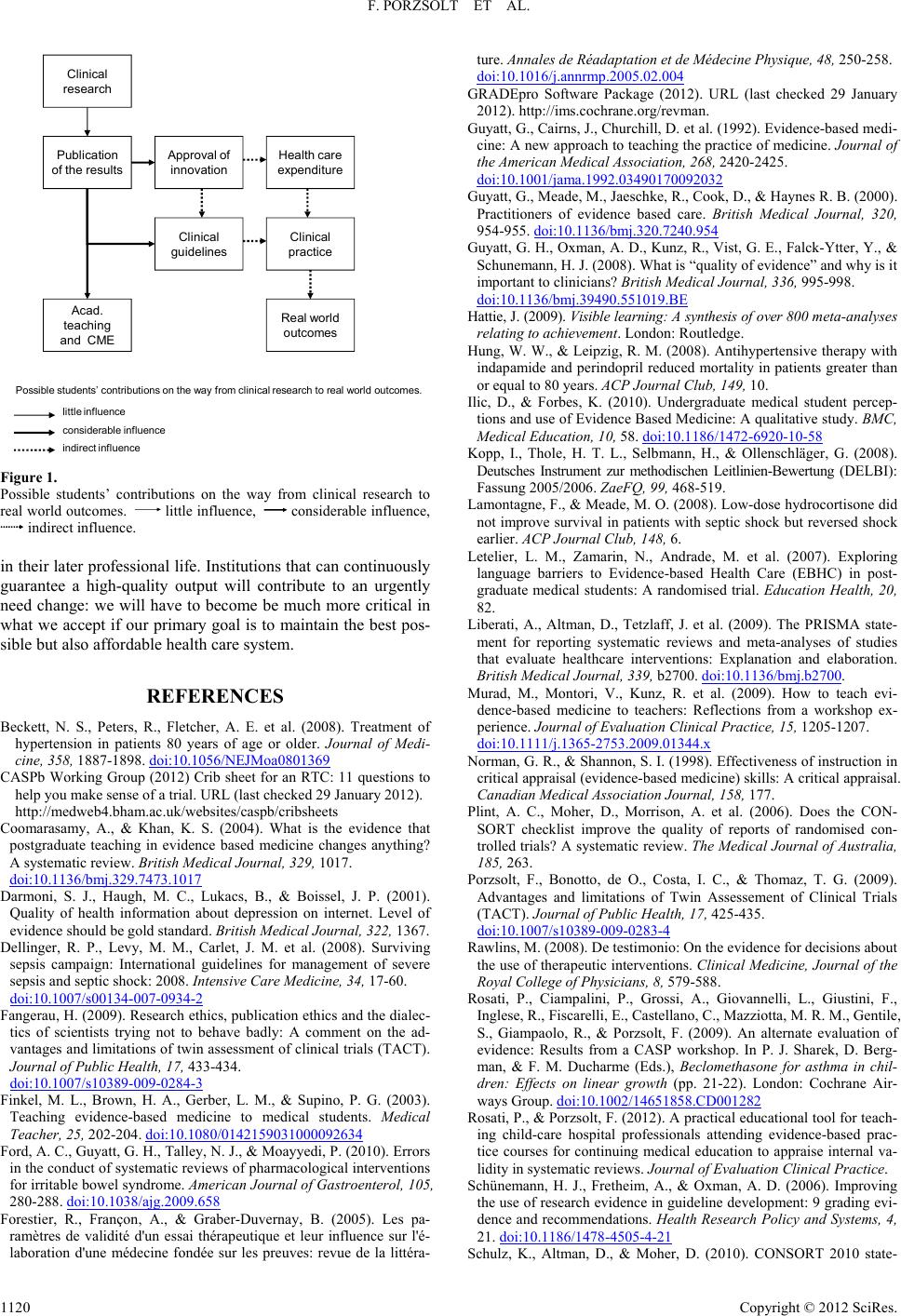
Possible students’ contributions on the way from clinical research to real world outcomes.
little influence
considerable influence
indirect influence
Figure 1.
Possible students’ contributions on the way from clinical research to
real world outcomes. little influence, considerable influence,
indirect influence.
in their later professional life. Institutions that can continuously
guarantee a high-quality output will contribute to an urgently
need change: we will have to become be much more critical in
what we accept if our primary goal is to maintain the best pos-
sible but also affordable health care system.
REFERENCES
Beckett, N. S., Peters, R., Fletcher, A. E. et al. (2008). Treatment of
hypertension in patients 80 years of age or older. Journal of Medi-
cine, 358, 1887-1898. doi:10.1056/NEJMoa0801369
CASPb Working Group (2012) Crib sheet for an RTC: 11 questions to
help you make sense of a trial. URL (last checked 29 January 2012).
http://medweb4.bham.ac.uk/websites/caspb/cribsheets
Coomarasamy, A., & Khan, K. S. (2004). What is the evidence that
postgraduate teaching in evidence based medicine changes anything?
A systematic review. British Medical Journal, 329, 1017.
doi:10.1136/bmj.329.7473.1017
Darmoni, S. J., Haugh, M. C., Lukacs, B., & Boissel, J. P. (2001).
Quality of health information about depression on internet. Level of
evidence should be gold standard. Brit i s h Medical Journal, 322, 1367.
Dellinger, R. P., Levy, M. M., Carlet, J. M. et al. (2008). Surviving
sepsis campaign: International guidelines for management of severe
sepsis and septic shock: 2008. Intensive C ar e M ed ic in e, 3 4, 17-60.
doi:10.1007/s00134-007-0934-2
Fangerau, H. (2009). Research ethics, publication ethics and the dialec-
tics of scientists trying not to behave badly: A comment on the ad-
vantages and limitations of twin assessment of clinical trials (TACT).
Journal of Public Health, 17, 433-434.
doi:10.1007/s10389-009-0284-3
Finkel, M. L., Brown, H. A., Gerber, L. M., & Supino, P. G. (2003).
Teaching evidence-based medicine to medical students. Medical
Teacher, 25, 202-204. doi:10.1080/0142159031000092634
Ford, A. C., Guyatt, G. H., Talley, N. J., & Moayyedi, P. (2010). Errors
in the conduct of systematic reviews of pharmacological interventions
for irritable bowel syndrome. American Journal of Gastroenterol, 105,
280-288. doi:10.1038/ajg.2009.658
Forestier, R., Françon, A., & Graber-Duvernay, B. (2005). Les pa-
ramètres de validité d'un essai thérapeutique et leur influence sur l'é-
laboration d'une médecine fondée sur les preuves: revue de la littéra-
ture. Annales de Réadaptation et de Médecin e Physique, 48, 250-258.
doi:10.1016/j.annrmp.2005.02.004
GRADEpro Software Package (2012). URL (last checked 29 January
2012). http://ims.cochrane.org/revman.
Guyatt, G., Cairns, J., Churchill, D. et al. (1992). Evidence-based medi-
cine: A new approach to teaching the practice of medicine. Journal of
the American Medical Association, 268, 2420-2425.
doi:10.1001/jama.1992.03490170092032
Guyatt, G., Meade, M., Jaeschke, R., Cook, D., & Haynes R. B. (2000).
Practitioners of evidence based care. British Medical Journal, 320,
954-955. doi:10.1136/bmj.320.7240.954
Guyatt, G. H., Ox man, A. D., Kunz, R., Vist , G. E., Falck-Ytter, Y., &
Schunemann, H. J . (2008). What is “quality of evidence” and why is it
important to clinicians? British Medical Journal, 336, 995-998.
doi:10.1136/bmj.39490.551019.BE
Hattie, J. (2009). Visible learning: A synthesis of over 800 meta-analyses
relating to achievement. London: Routledge.
Hung, W. W., & Leipzig, R. M. (2008). Antihypertensive therapy with
indapamide and perindopril reduced mortality in patients greater than
or equal to 80 ye a r s. ACP Journal Club, 149, 10.
Ilic, D., & Forbes, K. (2010). Undergraduate medical student percep-
tions and use of Evidence Based Medicine: A qualitative study. BMC,
Medical Education, 10, 58. doi:10.1186/1472-6920-10-58
Kopp, I., Thole, H. T. L., Selbmann, H., & Ollenschläger, G. (2008).
Deutsches Instrument zur methodischen Leitlinien-Bewertung (DELBI):
Fassung 2005/2006. ZaeFQ, 99, 468-519.
Lamontagne, F., & Meade, M. O. (2008). Low-dose hydrocortisone did
not improve survival in patients with septic shock but reversed shock
earlier. ACP Journal Club, 148, 6.
Letelier, L. M., Zamarin, N., Andrade, M. et al. (2007). Exploring
language barriers to Evidence-based Health Care (EBHC) in post-
graduate medical students: A randomised trial. Education Health, 20,
82.
Liberati, A., Altman, D., Tetzlaff, J. et al. (2009). The PRISMA state-
ment for reporting systematic reviews and meta-analyses of studies
that evaluate healthcare interventions: Explanation and elaboration.
British Medical Journal, 339, b2700. doi:10.1136/bmj.b2700.
Murad, M., Montori, V., Kunz, R. et al. (2009). How to teach evi-
dence-based medicine to teachers: Reflections from a workshop ex-
perience. Journal of Evaluation Clini c a l Practice, 15, 1205-1207.
doi:10.1111/j.1365-2753.2009.01344.x
Norman, G. R., & Shannon, S. I. (1998). Effectiveness of instruction in
critical appraisal (evidence-based medicine) skills: A critical appraisal.
Canadian Medical Association Journal, 158, 177.
Plint, A. C., Moher, D., Morrison, A. et al. (2006). Does the CON-
SORT checklist improve the quality of reports of randomised con-
trolled trials? A systematic review. The Medical Journal of Australia,
185, 263.
Porzsolt, F., Bonotto, de O., Costa, I. C., & Thomaz, T. G. (2009).
Advantages and limitations of Twin Assessement of Clinical Trials
(TACT). Journal of Public Health, 17, 425-435.
doi:10.1007/s10389-009-0283-4
Rawlins, M. (2008). De testimonio: On the e vi de nc e f or decisions about
the use of therapeutic interventions. Clinical Medicine, Journal of the
Royal College of Physicians, 8, 579-588.
Rosati, P., Ciampalini, P., Grossi, A., Giovannelli, L., Giustini, F.,
Inglese, R., Fiscarelli, E., Castellano, C., Mazziotta, M. R. M., Gentile,
S., Giampaolo, R., & Porzsolt, F. (2009). An alternate evaluation of
evidence: Results from a CASP workshop. In P. J. Sharek, D. Berg-
man, & F. M. Ducharme (Eds.), Beclomethasone for asthma in chil-
dren: Effects on linear growth (pp. 21-22). London: Cochrane Air-
ways Group. doi:10.1002/14651858.CD001282
Rosati, P., & Porzsolt, F. (2012). A practical educational tool for teach-
ing child-care hospital professionals attending evidence-based prac-
tice courses for continuing medical education to appraise internal va-
lidity in systematic reviews. Journal of Evaluation Clinical Practice.
Schünemann, H. J., Fretheim, A., & Oxman, A. D. (2006). Improving
the use of research evidence in guideline development: 9 grading evi-
dence and recommendations. Health Research Policy and Systems, 4,
21. doi:10.1186/1478-4505-4-21
Schulz, K., Altman, D., & Moher, D. (2010). CONSORT 2010 state-
Copyright © 2012 SciRes.
1120