Mucormycosis: A Review on Environmental Fungal Spores and Seasonal Variation of Human Disease
Copyright © 2012 SciRes. AID
80
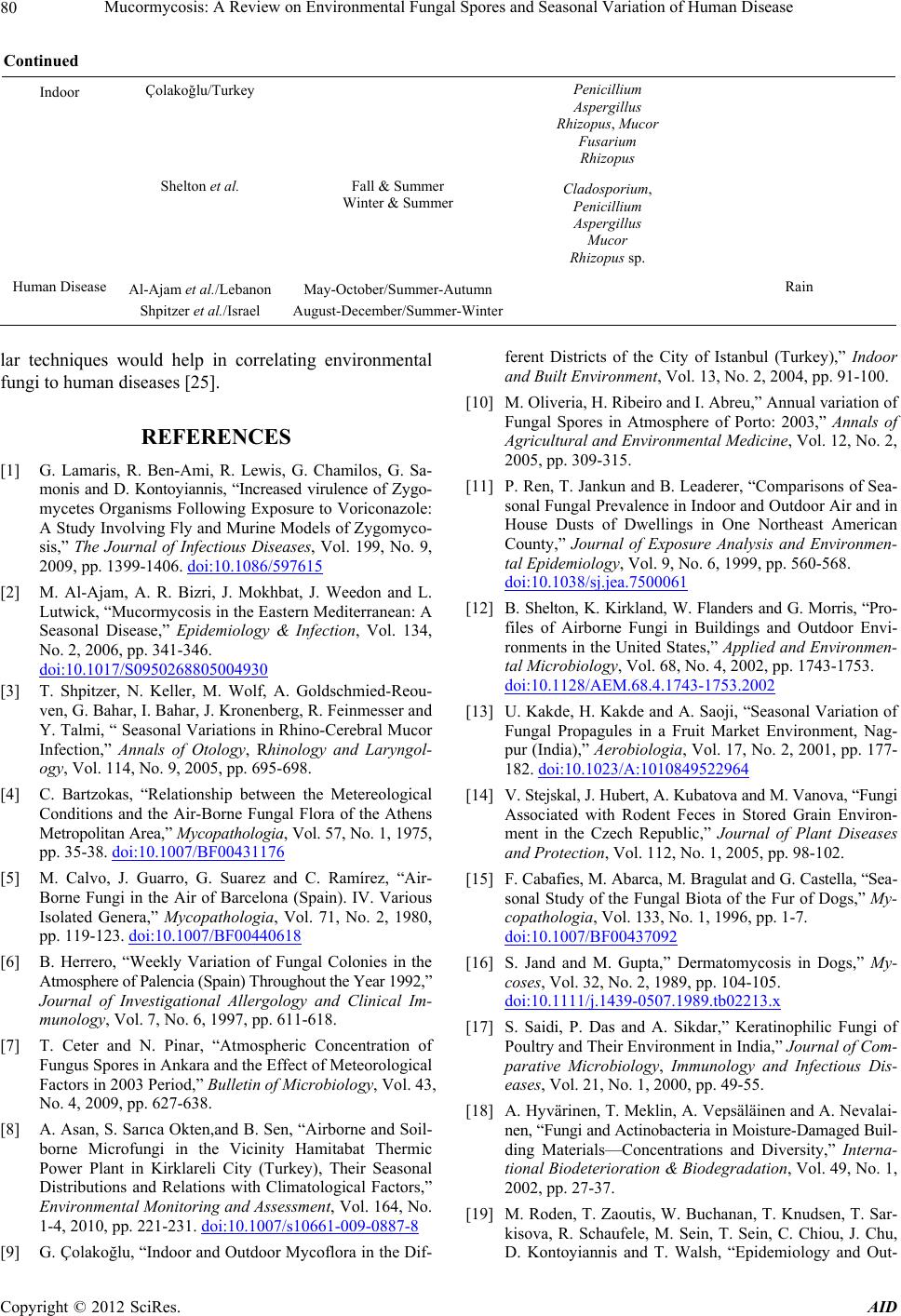
Continued
Indoor Çolakoğlu/Turkey Penicillium
Aspergillus
Rhizopus, Mucor
Fusarium
Rhizopus
Shelton et al. Fall & Summer
Winter & Summer Cladosporium,
Penicillium
Aspergillus
Mucor
Rhizopus sp.
Human Disease Al-Ajam et al./Lebanon May-October/Summer-Autumn Rain
Shpitzer et al./Israel August-December/Summer-Winter
lar techniques would help in correlating environmental
fungi to human diseases [25].
REFERENCES
[1] G. Lamaris, R. Ben-Ami, R. Lewis, G. Chamilos, G. Sa-
monis and D. Kontoyiannis, “Increased virulence of Zygo-
mycetes Organisms Following Exposure to Voriconazole:
A Study Involving Fly and Murine Models of Zygomyco-
sis,” The Journal of Infectious Diseases, Vol. 199, No. 9,
2009, pp. 1399-1406. doi:10.1086/597615
[2] M. Al-Ajam, A. R. Bizri, J. Mokhbat, J. Weedon and L.
Lutwick, “Mucormycosis in the Eastern Mediterranean: A
Seasonal Disease,” Epidemiology & Infection, Vol. 134,
No. 2, 2006, pp. 341-346.
doi:10.1017/S0950268805004930
[3] T. Shpitzer, N. Keller, M. Wolf, A. Goldschmied-Reou-
ven, G. Bahar, I. Bahar, J. Kronenberg, R. Feinmesser and
Y. Talmi, “ Seasonal Variations in Rhino-Cerebral Mucor
Infection,” Annals of Otology, Rhinology and Laryngol-
ogy, Vol. 114, No. 9, 2005, pp. 695-698.
[4] C. Bartzokas, “Relationship between the Metereological
Conditions and the Air-Borne Fungal Flora of the Athens
Metropolitan Area,” Mycopathologia, Vol. 57, No. 1, 1975,
pp. 35-38. doi:10.1007/BF00431176
[5] M. Calvo, J. Guarro, G. Suarez and C. Ramírez, “Air-
Borne Fungi in the Air of Barcelona (Spain). IV. Various
Isolated Genera,” Mycopathologia, Vol. 71, No. 2, 1980,
pp. 119-123. doi:10.1007/BF00440618
[6] B. Herrero, “Weekly Variation of Fungal Colonies in the
Atmosphere of Palencia (Spain) Throughout the Year 1992,”
Journal of Investigational Allergology and Clinical Im-
munology, Vol. 7, No. 6, 1997, pp. 611-618.
[7] T. Ceter and N. Pinar, “Atmospheric Concentration of
Fungus Spores in Ankara and the Effect of Meteorological
Factors in 2003 Period,” Bulletin of Microbiology, Vol. 43,
No. 4, 2009, pp. 627-638.
[8] A. Asan, S. Sarıca Okten,and B. Sen, “Airborne and Soil-
borne Microfungi in the Vicinity Hamitabat Thermic
Power Plant in Kirklareli City (Turkey), Their Seasonal
Distributions and Relations with Climatological Factors,”
Environmental Monitoring and Assessment, Vol. 164, No.
1-4, 2010, pp. 221-231. doi:10.1007/s10661-009-0887-8
[9] G. Çolakoğlu, “Indoor and Outdoor Mycoflora in the Dif-
ferent Districts of the City of Istanbul (Turkey),” Indoor
and Built Environment, Vol. 13, No. 2, 2004, pp. 91-100.
[10] M. Oliveria, H. Ribeiro and I. Abreu,” Annual variation of
Fungal Spores in Atmosphere of Porto: 2003,” Annals of
Agricultural and Environmental Medicine, Vol. 12, No. 2,
2005, pp. 309-315.
[11] P. Ren, T. Jankun and B. Leaderer, “Comparisons of Sea-
sonal Fungal Prevalence in Indoor and Outdoor Air and in
House Dusts of Dwellings in One Northeast American
County,” Journal of Exposure Analysis and Environmen-
tal Epidemiology, Vol. 9, No. 6, 1999, pp. 560-568.
doi:10.1038/sj.jea.7500061
[12] B. Shelton, K. Kirkland, W. Flanders and G. Morris, “Pro-
files of Airborne Fungi in Buildings and Outdoor Envi-
ronments in the United States,” Applied and Environmen-
tal Microbiology, Vol. 68, No. 4, 2002, pp. 1743-1753.
doi:10.1128/AEM.68.4.1743-1753.2002
[13] U. Kakde, H. Kakde and A. Saoji, “Seasonal Variation of
Fungal Propagules in a Fruit Market Environment, Nag-
pur (India),” Aerobiologia, Vol. 17, No. 2, 2001, pp. 177-
182. doi:10.1023/A:1010849522964
[14] V. Stejskal, J. Hubert, A. Kubatova and M. Vanova, “Fungi
Associated with Rodent Feces in Stored Grain Environ-
ment in the Czech Republic,” Journal of Plant Diseases
and Protection, Vol. 112, No. 1, 2005, pp. 98-102.
[15] F. Cabafies, M. Abarca, M. Bragulat and G. Castella, “Sea-
sonal Study of the Fungal Biota of the Fur of Dogs,” My-
copathologia, Vol. 133, No. 1, 1996, pp. 1-7.
doi:10.1007/BF00437092
[16] S. Jand and M. Gupta,” Dermatomycosis in Dogs,” My-
coses, Vol. 32, No. 2, 1989, pp. 104-105.
doi:10.1111/j.1439-0507.1989.tb02213.x
[17] S. Saidi, P. Das and A. Sikdar,” Keratinophilic Fungi of
Poultry and Their Environment in India,” Journal of Com-
parative Microbiology, Immunology and Infectious Dis-
eases, Vol. 21, No. 1, 2000, pp. 49-55.
[18] A. Hyvärinen, T. Meklin, A. Vepsäläinen and A. Nevalai-
nen, “Fungi and Actinobacteria in Moisture-Damaged Buil-
ding Materials—Concentrations and Diversity,” Interna-
tional Biodeterioration & Biodegradation, Vol. 49, No. 1,
2002, pp. 27-37.
[19] M. Roden, T. Zaoutis, W. Buchanan, T. Knudsen, T. Sar-
kisova, R. Schaufele, M. Sein, T. Sein, C. Chiou, J. Chu,
D. Kontoyiannis and T. Walsh, “Epidemiology and Out-