T. Ricon / HEALTH 2 (2010) 685-691
Copyright © 2010 SciRes. Openly accessible at http://www.scirp.org/journal/HEALTH/
691
691
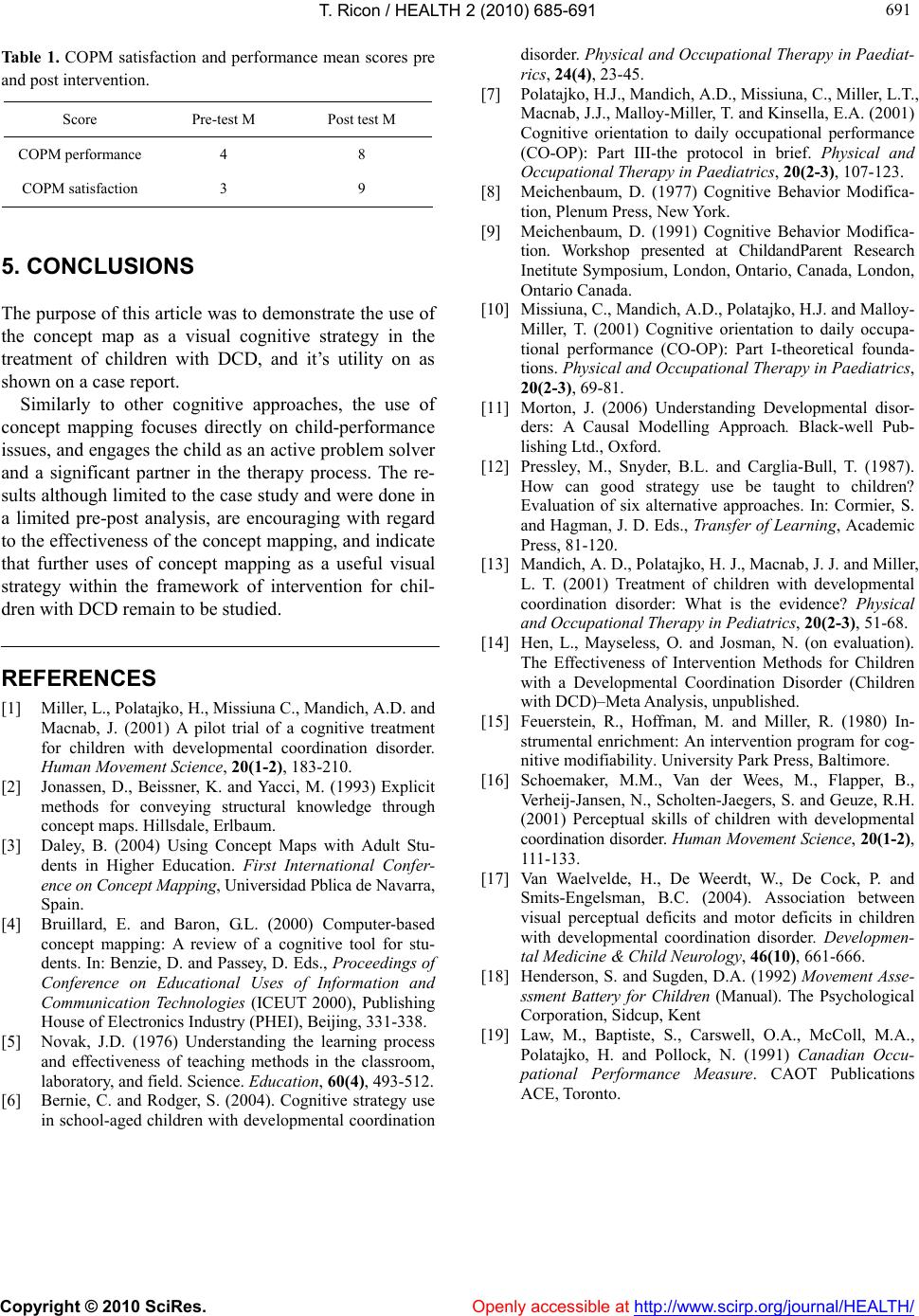
Ta ble 1 . COPM satisfaction and performance mean scores pre
and post intervention.
Score Pre-test M Post test M
COPM performance 4 8
COPM satisfaction 3 9
5. CONCLUSIONS
The purpose of this article was to demonstrate the use of
the concept map as a visual cognitive strategy in the
treatment of children with DCD, and it’s utility on as
shown on a case report.
Similarly to other cognitive approaches, the use of
concept mapping focuses directly on child-performance
issues, and engages the child as an active problem solver
and a significant partner in the therapy process. The re-
sults although limited to the case study and were done in
a limited pre-post analysis, are encouraging with regard
to the effectiveness of the concept mapping, and indicate
that further uses of concept mapping as a useful visual
strategy within the framework of intervention for chil-
dren with DCD remain to be studied.
REFERENCES
[1] Miller, L., Polatajko, H., Missiuna C., Mandich, A.D. and
Macnab, J. (2001) A pilot trial of a cognitive treatment
for children with developmental coordination disorder.
Human Movement Science, 20(1-2), 183-210.
[2] Jonassen, D., Beissner, K. and Yacci, M. (1993) Explicit
methods for conveying structural knowledge through
concept maps. Hillsdale, Erlbaum.
[3] Daley, B. (2004) Using Concept Maps with Adult Stu-
dents in Higher Education. First International Confer-
ence on Concept Mapping, Universidad Pblica de Navarra,
Spain.
[4] Bruillard, E. and Baron, G.L. (2000) Computer-based
concept mapping: A review of a cognitive tool for stu-
dents. In: Benzie, D. and Passey, D. Eds., Proceedings of
Conference on Educational Uses of Information and
Communication Technologies (ICEUT 2000), Publishing
House of Electronics Industry (PHEI), Beijing, 331-338.
[5] Novak, J.D. (1976) Understanding the learning process
and effectiveness of teaching methods in the classroom,
laboratory, and field. Science. Education, 60(4), 493-512.
[6] Bernie, C. and Rodger, S. (2004). Cognitive strategy use
in school-aged children with developmental coordination
disorder. Physical and Occupational Therapy in Paediat-
rics, 24(4), 23-45.
[7] Polatajko, H.J., Mandich, A.D., Missiuna, C., Miller, L.T.,
Macnab, J.J., Malloy-Miller, T. and Kinsella, E.A. (2001)
Cognitive orientation to daily occupational performance
(CO-OP): Part III-the protocol in brief. Physical and
Occupational Therapy in Paediatrics, 20(2-3), 107-123.
[8] Meichenbaum, D. (1977) Cognitive Behavior Modifica-
tion, Plenum Press, New York.
[9] Meichenbaum, D. (1991) Cognitive Behavior Modifica-
tion. Workshop presented at ChildandParent Research
Inetitute Symposium, London, Ontario, Canada, London,
Ontario Canada.
[10] Missiuna, C., Mandich, A.D., Polatajko, H.J. and Malloy-
Miller, T. (2001) Cognitive orientation to daily occupa-
tional performance (CO-OP): Part I-theoretical founda-
tions. Physical and Occupational Therapy in Paediatrics,
20(2-3), 69-81.
[11] Morton, J. (2006) Understanding Developmental disor-
ders: A Causal Modelling Approach. Black-well Pub-
lishing Ltd., Oxford.
[12] Pressley, M., Snyder, B.L. and Carglia-Bull, T. (1987).
How can good strategy use be taught to children?
Evaluation of six alternative approaches. In: Cormier, S.
and Hagman, J. D. Eds., Transfer of Learning, Academic
Press, 81-120.
[13] Mandich, A. D., Polatajko, H. J., Macnab, J. J. and Miller,
L. T. (2001) Treatment of children with developmental
coordination disorder: What is the evidence? Physical
and Occupational Therapy in Pediatrics, 20(2-3), 51-68.
[14] Hen, L., Mayseless, O. and Josman, N. (on evaluation).
The Effectiveness of Intervention Methods for Children
with a Developmental Coordination Disorder (Children
with DCD)–Meta Analysis, unpublished.
[15] Feuerstein, R., Hoffman, M. and Miller, R. (1980) In-
strumental enrichment: An intervention program for cog-
nitive modifiability. University Park Press, Baltimore.
[16] Schoemaker, M.M., Van der Wees, M., Flapper, B.,
Verheij-Jansen, N., Scholten-Jaegers, S. and Geuze, R.H.
(2001) Perceptual skills of children with developmental
coordination disorder. Human Movement Science, 20(1-2),
111-133.
[17] Van Waelvelde, H., De Weerdt, W., De Cock, P. and
Smits-Engelsman, B.C. (2004). Association between
visual perceptual deficits and motor deficits in children
with developmental coordination disorder. Developmen-
tal Medicine & Child Neurology, 46(10), 661-666.
[18] Henderson, S. and Sugden, D.A. (1992) Movement Asse-
ssment Battery for Children (Manual). The Psychological
Corporation, Sidcup, Kent
[19] Law, M., Baptiste, S., Carswell, O.A., McColl, M.A.,
Polatajko, H. and Pollock, N. (1991) Canadian Occu-
pational Performance Measure. CAOT Publications
ACE, Toronto.