Journal of Cancer Therapy
Vol. 4 No. 1 (2013) , Article ID: 28165 , 9 pages DOI:10.4236/jct.2013.41037
Treatment Outcome of Pelvic Osteosarcoma a 20-Year Experience in a Single Institution*
![]()
Department of Orthopaedic Surgery, Koisn University Gospel Hospital, Busan, Korea.
Email: #shchung@kosin.ac.kr
Received October 16th, 2012; revised November 18th, 2012; accepted November 26th, 2012
Keywords: Osteosarcoma; Pelvis; Limb Salvage
ABSTRACT
Purpose: Osteosarcoma of limbs shows excellent therapeutic results due to development of diagnostic and treatment methods. However, osteosarcoma of pelvic bone is known to have lower incidence than those of limbs and poorer prognosis. This study is performed to research the diagnosis, treatment, treatment outcomes, and complications of osteosarcoma of pelvic bone and propose standards for adequate treatment. Objective and Method: 16 cases that were diagnosed as osteosarcoma of pelvic bone from January 1988 to October 2010 in Kosin University Gospel Hospital were analyzed. Follow-up periods were at least 2 months up to 60 months. There were 6 cases of male and 10 cases of female, and mean age was 44.3 (14 ~ 74) years old. 5 cases were accompanied by pulmonary metastasis at the time of the diagnosis. Surgical treatment including preoperative and postoperative chemotherapy was performed in 9 cases, and only chemotherapy and radiation were performed in 1 case. Among 9 cases having undergone surgical treatment, 3 cases were performed with biological reconstruction using autogenous bone graft and total hip replacement together, 1 case was performed with extracorporeal irradiated recycled autogenous bone graft, 1 case was performed with reconstruction using tumor prosthesis, and 4 cases were performed with wide excision. Retrospective review was done about diagnostic procedures, treatment methods and results, and complications. Results: Mean period from the onset of symptoms to the time of the diagnosis was 6.3 (3 ~ 12) months, and the symptoms were 7 cases of hip pain, each 3 cases of lumbar pain and radiating pain to lower limbs, pelvic mass, each 2 cases of inguinal pain, and each 1 case of thigh pain, Among the 9 cases performed with preoperative and postoperative chemotherapy and surgical treatment, there were 6 cases of T-10 protocol, 2 cases of T-20 protocol, and 1 case of IA (Intraarterial) Cis protocol. In the 1 case that haven’t undergone surgical treatment, T-10 protocol was performed. 13 of the 16 cases were expired, with the mean time of 15 (2 ~ 47 months) from the time of the diagnosis to death. Complications were 4 cases of surgical infection, and 1 case of peroneal nerve palsy. Conclusion: Osteosarcoma occurred in the pelvic bone may delay the start of the diagnosis and treatment, and prognosis is too bad. Early diagnosis is important, and this purpose, high-resolution and precise imaging tests performed with tumorrelated blood tests is necessary. In addition, preoperative systemic chemotherapy, rather than intra-aterial chemotherapy is recommended.
1. Introduction
Osteosarcoma is a malignant bone tumor which consists of variable connective tissues with broad spectrum of possibilities to malignancy. Known as approximately 20 percent of primary malignant bone tumor, the real incidence of osteosarcoma is thought to be more than that, which is one of the most common and important primary malignant tumor [1,2]. Conventional osteosarcoma is most common type of osteosarcoma. It is categorized into osteoblastic, chondroblastic, fibroblastic type according to dominant component of osteosarcoma. Osteoid and bone with mineral appears to sclerotic type; cartilage, spindle cell, histocyte, endothelial cell without minerals appears to osteolytic type; and both types could be observed. Whether which histological component is dominant, tumor osteoid or woven bone produced by malignant tumor cell are most important clue to diagnosis. For the past 30 years, the survival rate has been increased due to accurate diagnostic technique, various types of surgical methods and the development of effective anti-cancer chemotherapy regimens in the treatment of osteosarcoma of the extremities. Thus, it has ecently reached 60% - 70% [1-4]. But the osteosarcoma of the pelvic bone accounts for only 5% - 11% of total cases and its prevalence has been reported to be relatively lower. In addition, the timing of diagnosis is delayed because of various symptoms such as pelvic pain, lower back pain and radiating pain [5]. Because of a greater size of the tumor at the time of diagnosis and the complicated anatomical structures in the pelvic bone, there is a great difficulty of its surgical management. The survival rate in patients with osteosarcoma of the pelvic bone has been reported to be approximately 30% and this is markedly lower than that seen in cases of the extremities [1,2,3,6]. Because of a smaller sample size due to a lower prevalence and survival, only a small number of cases of the osteosarcoma of the extremities have been reported worldwide. But there are very reports about its treatment outcomes [7,8].
Given the above background, we examined the treatment outcomes in patients with osteosarcoma for whom a diagnosis was made at our medical institution.
2. Patients and Methods
Of 253 patients who were diagnosed with osteosarcoma at our medical institution during a period ranging from January of 1988 to October of 2010, 16 had a primary tumor in the pelvic bone. Our clinical series of patients were composed of six men and ten women, whose mean age was 44.3 years (range, 15 - 74 years). These patients had a mean follow-up period of 12.6 months (range, 2 - 60 months). At the time of diagnosis, all the patients underwent a plain radiography, a computed tomography (CT) of the affected sites, a chest CT, a magnetic resonance imaging (MRI) of the affected sites, a whole-body bone scan or PET-CT (positron emission tomography). In patients who had no obvious relationship between the nerve and the blood vessels in the pelvic cavity, an angiography was concomitantly performed. The location of the primary sites was determined based on the Musculoskeletal Tumor Society Classification, according to which there were four cases of P1, eight cases of P2 (Figures 1-3) and four cases of P3 [9]. At the time of diagnosis, there were five cases of pulmonary metastasis. Malignant tumors were classified under the Enneking system, according to which there were one case of Stage IA, three cases of Stage IB, seven cases of Stage IIB and five cases of Stage III. Of these, nine patients underwent a pelvectomy following a preoperative anti-cancer chemotherapy. Surgical approaches include an ilio-inguinal approach or a Kocher-Langenbeck one, which varied depending on the location of tumor and biopsy [8, 10]. The scope of resection was based on the classification systems of Enneking and Durham. As the methods of resection, there were one case of Type I, five cases of Types I+II, two cases of Types I + II + II and one case of Type III [1,3]. In regard to the evaluation of the margin of excision, a wide margin was evaluated in cases in

Figure 1. Plane Radiograph of Pelvis AP of a 15-year female with right hip pain (case No. 3) showed radiolucent bony lesion in right acetabulum and ilium.
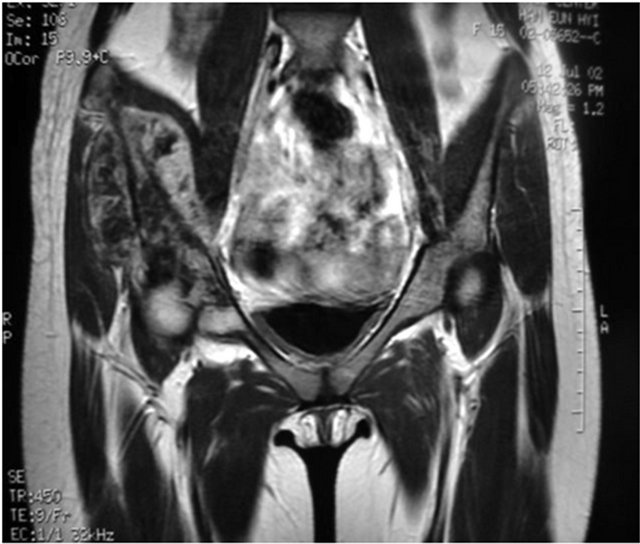
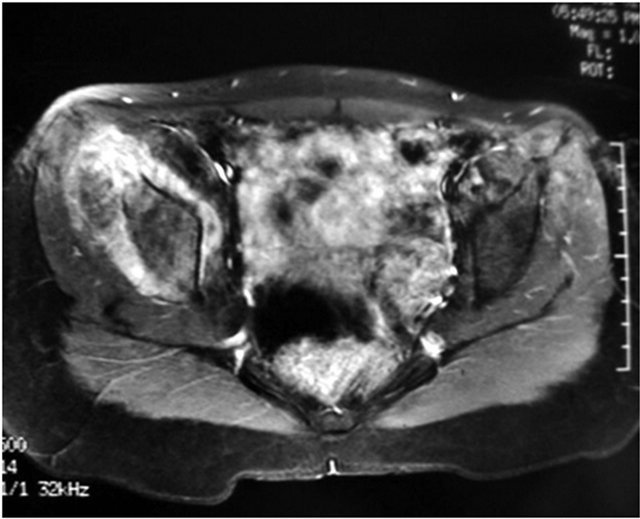
Figure 2. Axial and coronal image revealed bony lesion of extraosseous extension and inhomogeouns signal intensity of mass and surrounding muscle (case No. 3).

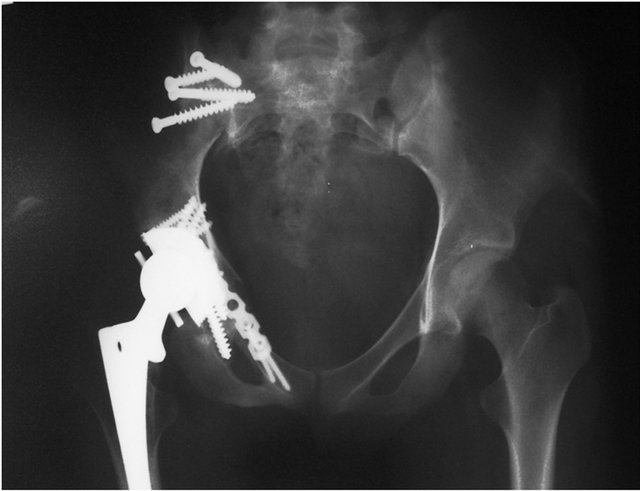
Figure 3. The result of incisional biopsy was grade 2 osteosarcoma. An Enneking Type I + II pelvic resection and reconstruction with pastueurized autobone and THRA was performed, 12 months follow up radiograph of pelvic AP, The functional score was 80% of normal limb.
which the tumor was excised including the adjacent normal muscles such as the iliacus muscle. In cases in which the dissection could be done although major nerves and vessels had a contact with the tumor, a marginal excision was evaluated. In cases in which the excision margin was positive on histopathology following the excision of tumor, an intralesional excision was evaluated. This showed that there were five cases of the extensive resection margin, three cases of the margin and one case of the intralesional margin. In the methods of the reconstruction following the resection, there was a variability depending on the location of primary lesions and the degree of defects formed following the resection. There were no reconstructions for both Type I and III excision. In the excision including the acetabulum, among a mobile arthroplasty, an arthrodesis and a pseudoarthroplasty, each one was selected depending on the location and size of the tumor and the degree of bone destruction. Of six cases for which a reconstruction was performed following the pelvectomy, there were five cases for which a recycling autograft was performed (three cases for which a pasteurization was performed and two cases for which an extracorporeal irradiation was performed) and one case for which a saddle prosthesis was used. In three cases, there were no reconstructions following the excision of tumor. In nine cases, the anti-cancer chemotherapy was performed both preoperatively and postoperatively. In six of these cases, according to the T-10 methods of Rosen et al., methotrexate (12 g/m2) was administered twice at a 1-week interval and this was followed by the administration of adraimycin (60 mg/m2) and cisplatin (100 g/m2) one week later, which was defined as one cycle of the treatment. Thus, a total of six cycles were performed. In two cases, the T20 method was performed with the addition of ifosamide (18 g/m2/8 days) to the T10 method. In one case, the surgical treatment was performed after an intraarterial chemotherapy with cisplatin (120 mg/m2) was performed twice after an interventional radiological angiography was preoperatively performed twice. In six patients, the chemotherapy was not completed due to an aggravation of the systemic status during a preoperative anti-cancer chemotherapy following a histopathologic diagnosis. All of these six patients died within six months. According to the histopathological classification, there were nine cases of a typical form of central osteosarcoma, five cases of osteogenic sarcoma, one case in which there was a concurrent presence of liposarcoma and one case of radiationinduced osteosarcoma. The follow-up period was defined as the length of time elapsed until the death occurred following a histopathologic diagnosis. In cases in which the final follow-up was unavailable or the death occurred within five years, however, the follow-up period was defined as the time elapsed until the corresponding events were noted. Thus, we examined oncologic outcomes (survival, recurrence and metastasis), initial symptoms, the length of time elapsed until a diagnosis was confirmed, complications and functional outcomes. In cases of survival, functional outcomes were evaluated using a questionnaire and a telephone interview which were both performed at a final outpatient visit by patients. In cases of death, functional outcomes were evaluated based on the clinical findings prior to the aggravation of systemic conditions and at a final outpatient visit. Functional outcomes were defined based on the Musculoskeletal Tumor Society functional classification scale which was established by the International Symposium on Limb Salvage (ISOLS) from 1993. This scale is composed of six items such as “Pain”, “Function”, “Emotional acceptance”, “Use of external acceptance”, “Walking ability” and “Gait”. Each item was scored with 0 to 5 points based on a questionnaire. Thus, the percentile value (%) to the normal functions was analyzed [8]. Statistical analysis was performed using SPSS 14.0, for which a Kruskal-Wallis test was used. A P-value of <0.05 was considered statistically significant.
3. Results
3.1. Oncologic Results
At a final follow-up in 16 patients with osteosarcoma of the pelvic bone, there were three patients (18.8%) with the continuous disease-free (CDF) survivals and 13 who died of diseases (DOD). The mean follow-up period was 12.6 months (range, 2 - 60 months). Until a diagnosis was made since the symptoms were first noted, a mean period of six months (range, 2 - 12 months) elapsed. In addition, there were seven cases of pain around the hip joint, three cases of low back pain accompanied by the radiating pain and two cases of inguinal pain. But there were only three cases in which the pelvic mass was palpated. In addition to five cases in which the pulmonary metastasis was detected at the time of diagnosis, there were two cases of pulmonary metastasis that occurred on postoperative months 4 and 10, respectively. Histopathologically, these cases had TNM stages of IIb and III, respectively. The corresponding patients underwent the anti-cancer chemotherapy following the excision of metastatic lesions, but died on postoperative months 9 and 18.
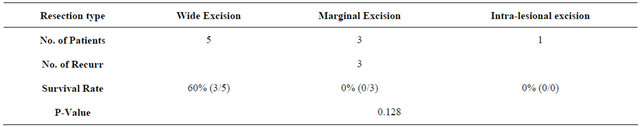
3.2. Local Recurrence
Three cases (30%) of local recurrence occurred on postoperative months 5, 8 and 11. By the methods of excision, there were two cases of Type I + II excision and one case of Type I + II + III excision. In one case of I + II excision, there was a concurrent presence of the pulmonary metastasis. In cases of local recurrence, the resection margin was found to be a marginal excision. In two cases, the anti-cancer chemotherapy was performed following the excision of metastatic lesions. In one case, the anti-cancer chemotherapy was performed concomitantly with the
Table 1. Patient, tumor and treatment factors, and survival of 16 patients with pelvic osteosarcoma.
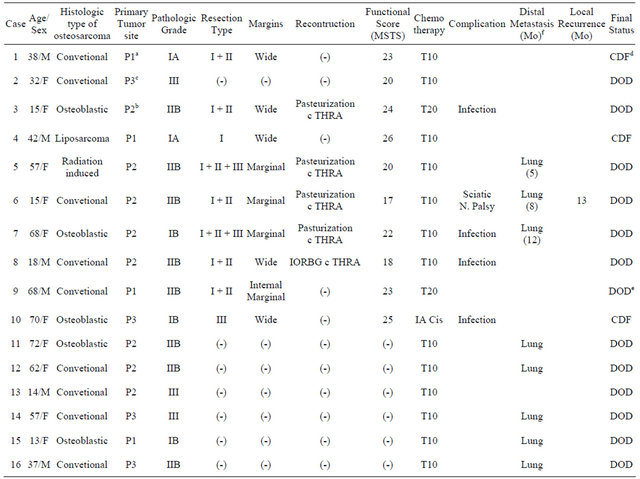
a: illium; b: periacetabular region; c: pubis and ischium; d: continously disease free; e: died of disease; f: measured from the time of diagnosis.
lumbar sympathetic ganglion block. All the three patients died on postoperative months 10, 14 and 20 (Table 1).
3.3. Complications
In five of a total of 16 patients, the postoperative complications occurred. In four patients, the infections occurred within a year postoperatively. Accordingly, these patients were treated with a debridement and an intravenous injection of antibiotics. The infections occurred in three (60%) of five patients who underwent a recycling autograft and one (33%) of three who underwent an extensive resection. Besides, there was one case of peroneal nerve palsy. Eight months postoperatively, our clinical series of patients received an advancement of the posterior tibial tendon. In two patients who underwent a pseudo-arthroplasty following the resection, there were no omplications that required a revision arthroplasty.
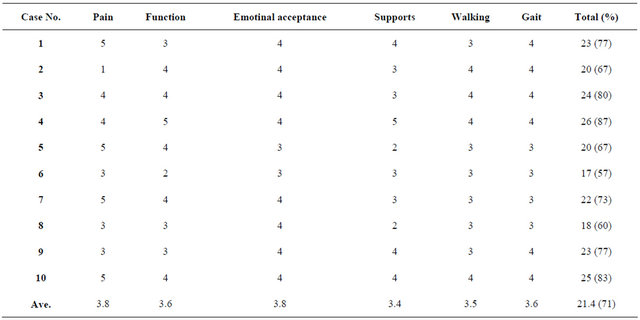
3.4. Functional Outcomes
At a final follow-up, the functional outcomes were evaluated in ten patients except for six who died during a preoperative chemotherapy. This showed a mean score of 21.4 points (71%). In two patients for whom the iliac wing and the pubic region were solely resected, the mean scores were 24 points (80%). A total of eight patients underwent a resection including the acetabulum. Of these, in three patients who underwent a low-temperaturetreated recycling autograft, the mean scores were 22 points (73%). Besides, the mean scores were 18 points (60%) in two patients who underwent an extracorporeally irradiated recycling autograft, 17 points (57%) in one who had a saddle-type prosthesis implanted and 24.5 points (82%) in two had no reconstruction procedures. These results indicate that the mean scores of the functional outcomes were relatively lower in patients who had a saddle-type prosthesis implanted. But this reached no statistical significance (p = 0.372) (Table 2).
4. Discussion
Osteosarcoma of the pelvic bone is such a very rare entity as to account for only 8% ~ 10% of total cases. Besides, its outcomes and prognosis are much poorer as compared with that of the extremities, which can be explained by several reasons [2,11]. Firstly, the pelvic bone has notable anatomical characteristics. The pelvic bone is characterized by the region with a smaller thickness, the iliac wing in particular, and a lack of the fascia or other anatomical structures that play a role in preventing the invasion to the intra-pelvic and extra-pelvic space like a barrier. This eventually leads to the spreading of osteosarcoma to the lumbosacral plexus outside of the pelvic cavity along the adjacent bony structures (sacrum and vertebral body), joints (sacro-iliac joint, symphysis pubica and hip joint), the gluteal muscle, the iliac artery, vein and lymphatic vessels through the adjacent body organs or retroperitoneal organs (urinary bladder, prostate gland and ureter in particular) via vertebral foramen. According to Spanier et al., a poor prognosis is expected in cases in which the osteosarcoma of extremities had a metastasis to more than two adjacent muscles, blood vessels and nerves from the bony sites [3,12]. In addition, Tayler et al. reported that a prognosis is poorer in cases
Table 2. Functional scores according to the revised ISOLS’s criteria.
in which the osteosarcoma of extremities invaded the adjacent soft tissue and blood vessels as compared with those in which the size of tumor was greater than 15 cm [3]. In the current study, based on the findings of imaging study which was performed at the time of diagnosis and surgical findings at an operation room, there was an invasion in the internal iliac artery in seven patients and in the sciatic nerve in two patients. In five of these nine cases, the death occurred within a mean period of 2.4 months (range, 2 - 5 months) without completing a preoperative chemotherapy following a histopathologic diagnosis. In three of patients whto underwent a chemotherapy and surgical treatment preoperatively or postoperatively, the recurrence or death occurred also had a past history of taking the treatment for the symptoms due to orthopedic or gynecologic diseases, which can commonly be encountered in a within a mean period of eight months (range, 5 - 11 months).
Secondly, a diagnosis is delayed in cases of osteosarcoma of the pelvic bone as compared with that of the extremities. In regard to the length of time elapsed until a diagnosis is made until the symptoms are noted, L.Daniel et al. reported that a mean period of ten months (range, one month-four years) elapsed [13] and Fahey et al. did that a mean period of six months (range, 1 - 15 months) elapsed [2]. Also in the current study, a mean period of six months (range, one month - two years) elapsed for a diagnosis to be established. This implies that a greater length of time elapsed as compared with 2.3 months, reported by Bielack et al., in making a diagnosis of osteosarcoma of the extremities [4] and 1.9 months, reported by Pollock et al., in making a diagnosis of tumors in infants and children [14]. In addition, a greater length of time also elapsed as compared with two months that we had experienced while making a diagnosis of osteosarcoma of the extremities at our medical institution. This is because the prevalence of osteosarcoma of the pelvic bone is approximately 4% - 10% of total cases and this corresponds to a very low value. Our results showed that 13 patients had a higher prevalence of the osteosarcoma of the pelvic bone, except for three who complained of the presence of a mass around the pelvis, as compared with that of the extremities. Besides, these patients the symptoms due to orthopedic or gynecologic diseases, which can commonly be encountered in a clinical setting, such as degenerative arthritis of the hip joint, spinal stenosis, the intervertebral disc herniation and pelvic inflammatory disease. Besides, there are no notable symptoms of the osteosarcoma of the pelvic bone. Most of the patients presented with non-specific symptoms. L. Daniel et al. reported that patients complain of pain around the hip joint, back pain, inguinal pain and radiating pain [13]. Also in the current study, there were seven cases of the pain of the hip joint, three cases of the lower back pain accompanied by the radiating pain and two cases of the inguinal pain. But there were only three patients (18%) who complained of a palpable mass in the pelvis. As described here, most cases of the osteosarcoma of the pelvic bone were misdiagnosed as other diseases. This led to a lack of the diagnosis and treatment at earlier occasions. Moreover, there were five cases (31%) in which there was a metastasis to other organs outside of the pelvic cavity at the time of diagnosis. Furthermore, there were six cases of the death occurring during a preoperative chemotherapy. In these cases, a diagnosis was made in such a condition that there were a metastasis to other organs and a notable tumor progression. Thirdly, there is a great difficulty in obtaining a sufficient degree of resection margin for the surgical removal of the osteosarcoma of the pelvic bone. In cases of osteosarcoma of the extremities, because there is a long bone shape [10, 15-18], it is possible to make a differentiation between the proximal and distal part in performing an extensive resection of the tumor. In cases of osteosarcoma of the pelvic bone, however, not only because the pelvic bone has an elliptical shape but also because it surrounded by such adjacent structures as the sacrum, lumbar spine, blood vessels, nerve and muscles in a 3-dimensional manner with no differentiation between the proximal and distal part of the pelvis, damages to the adjacent structures would therefore be unavoidable if a sufficient degree of the margin could be obtained [16,19]. This might also lead to the occurrence of various types of sequelae. Besides, there is also a possibility that the adjacent structures might be contaminated even during surgery because of a complicated anatomy of the pelvic cavity. In particular, in cases in which the osteosarcoma invaded the sacral cavity, vertebral canal and the iliac artery and vein, it would be impossible to perform an extensive resection. According to Rizzolli et al., a 7-year survival rate was 97% in cases of osteosarcoma in which a sufficient degree of resection margin was obtained. These authors also noted, however, that the survival rate was significantly reduced to 71% in otherwise cases [20]. Besides, according to B.G.I et al., the rate of local recurrence was 13% following an extensive excision, 38% following a debridement and 80% following an intralesional excision in cases of osteosarcoma of the pelvic bone [21]. In addition, according to Fahey M. et al., both a positive surgical margin (PSM) and a local recurrence were commonly found in the sacrum, lumbar spine, intrapelvic vessels, rectum and urinary bladder [2,11]. According to B.G.I. et al., a 1-year, 2-year, 5-year and 10-year survival rate were 68%, 51%, 41% and 35%, respectively, in cases of local recurrence. These authors also noted that the survival rate was further decreased in cases in which the local recurrence was concurrently found with the metastasis. That is, a 1- and 2-year survival rates were at most 30% and 14%, respectively [21]. In the current study, the survival rate was 50% (3/6) in patients who underwent an extensive resection. Besides, it was found to be 0% (0/4) in patients who underwent a debridement or an intralesional excision. Furthermore, local recurrence was noted in all the three patients who underwent a debridement, all of whom died within 18 months (Table 3). Fourthly, the infections were the complications that occurred the most frequently following surgery. According to B.G.I. et al., the infections occurred in 32% of patients who underwent surgery for the management of osteosarcoma of the pelvic bone. Mrake reported that the deep infections occurred in two of eight patients [21]. According to Abudu et al., the complications occurred in approximately 60% of patients who underwent the reconstruction surgery. According to these authors, 26% of the above patients presented with such complications as dislocation, arterial thrombosis and sciatic nerve palsy in a decreasing order [17]. According to Song et al., because there are many cases in which the adjacent muscles and soft tissues should be dissected to obtain a margin of the excision in the surgical excision of bone tumor as well as the atogenous bone graft, the recycled bony tissue simply plays a role like a foreign body that fills the empty space because of the soft tissue defects and the devascularization despite the anatomical reconstruction. This greatly raises risks of developing early-stage infections. These authors therefore noted that there is a higher degree of the risk of developing infections in cases in which the postoperative anti-cancer chemotherapy or a massive dissection of the soft tissue were mandatory [22,23], In our clinical series of patients, there were four cases of infections. All of these cases were completely treated with an intravenous injection of antibiotics and a debridement of the injection of antibiotics and a debridement of the infectious sites. Besides, there were no patients who had an internal fixator removed. In addition, the sural nerve was partially excised to obtain a sufficient degree of resection margin. This led to the occurrence of sural nerve palsy. Eight months postoperatively, this was followed by the advancement of posterior tibial tendon. In three patients who had no reconstruction procedures, however, there were no complications. Finally, in regard to the posterior functional outcomes, generally from a perspective of the sites of tumor and the scope of resection, there are no damages to the axis of weight bearing in patients who underwent a single resection of the iliac wing or the pubic region. Good functional outcomes could therefore be obtained despite a lack of the reconstruction. In patients for whom it would be unavoidable to resect the acetabulum, however, it is very difficult to replace the hip joint which is essential for weight bearing and functions from a long-term perspective [11,19,24].
It would be the most anatomical and physiologic method to perform a reconstruction using an autogenic composite graft or a recycling autologous graft. If the allogenic bone is used, however, there are following characteristics: [10] a difficulty in obtaining the appropriate donor bone, [7] a higher rate of infection and [8] a lack of the applicability of the surgical procedure to cases of severe bone destruction despite an anatomical consistency. Besides, there is a higher risk of developing earlystage infections and there is also a possibility that a loosening of the prosthesis or bone resorption might occur because the allogenic or heat-treated autologous bone are not viable tissue. In addition, if the allogenic or autogenous bone were used, it would be more difficult to achieve a rigid fixation as compared with the long bones of the extremities. Because the bone fusion cannot be well achieved accordingly, a loosening or a destruction of the internal fixator would also occur due to the resorption or non-fusion of autogenous bone. This might also be accompanied by the problems with a long-term durability [16,24,25]. In the current study, at a final follow-up, the mean scores were 23.6 points (78.6%) and this corresponded to the highest value in patients who underwent a pseudo-arthroplasty. In addition, these values were also found to be 21.2 points (70.6%) in patients who had a heat-treated autogenous bone implanted, 18.4 points (61.3%) in those who received an extracorporeal irradiation and 16.4 points (54.6%) in those who had a saddle prosthesis implanted (Table 3). A pseudo-arthroplasy without the reconstruction following the resection had the most excellent treatment outcomes, and it is one of the classical methods that have commonly been used to treat the infectious diseases in the hip joint. Because it is expected to cause a severe shortening of the lower ex
Table 3. Recurrence rate according to resection type.
tremities and a loss of the functions, there are some reports, that no reconstruction is attempted for these cases, only in a limited scope. Accordingly, there are advantages of a pseudo-arthroplasty that a sufficient degree of the margin of excision can be obtained, the operation time can be shortened, the amount of blood loss can be reduced, the risk of bleeding can be lowered, there is no external fixation following the surgery and patients can immediately perform a gait after the pain disappeared [19, 26-29]. Because of the compensation of the lumbar spine and the contralateral pelvic bone due to a loss of the adductor muscle of the hip joint and the shortening of lower extremities, however, there is also a possibility that lower back pain and physiologic scoliosis might occur. But there are advantages that no further surgical treatments are needed because of the mechanical defects unless there is a local recurrence. In our clinical series of patients, there were two who had a pseudo-arthrosis without the reconstruction procedures but presented with no complications. These patients could perform a gait from postoperative month 2 on. They had more excellent functional outcomes as compared with those who presented with the complications following the reconstruction procedures.
5. Conclusions
Osteosarcoma of the pelvic bone is a very rare disease entity, for which only an insufficient number of studies have been conducted up to present.
According to the current study, in cases of osteosarcoma of the pelvic bone, diagnosis was delayed because of its anatomical characteristics as compared with those of osteosarcoma of the extremities. The initiation of diagnosis and treatment was therefore delayed. In addition, both treatment outcomes and a prognosis were poorer in cases of osteosacoma of the pelvic bone. Particularly in cases of older age, an insufficient margin of the excision and an invasion to the adjacent blood vessels and nerve, functional outcomes were poorer. In patients who achieved a pseudo-arthrosis without the reconstruction procedures, as compared with patients who underwent a reconstruction following a resection of the tumor, the incidence of complications was lower and the degree of satisfaction with functional outcomes was higher.
In making a diagnosis of the osteosarcoma of the pelvic bone as the earliest as possible, it might be necessary to perform a blood test for such markers as alkaline phosphatase or lactate dehydrogenase as well as meticulous imaging studies (e.g., a computed tomography or a magnetic resonance imaging) under the suspicion of abnormalities in the pelvic cavity in patients who visited the outpatient clinic with chief complaints of the pain in the pelvis or hip joint or the lower back pain. In addition, it might be preferable to perform an intraarterial chemotherapy following a preoperative interventional radiographic angiography to a preoperative systemic chemotherapy following the diagnosis. This would be helpful in reducing the size of tumor with the direct action of anticancer drugs on the tumor, performing an extensive resection while preserving the adjacent muscle and soft tissue, minimizing the occurrence of postoperative complications and improving the functional outcomes. If severe defects are expected to occur following surgery, it might be recommended not to perform a reconstruction following the resection.
REFERENCES
- A. Kawai, A. G. Huvos, P. A. Meyers and J. H. Healey, “Osteosarcoma of the Pelvis: Oncologic Result of 40 Patients,” Clinical Orthopaedics, Vol. 348, 1998, pp. 196- 207.
- M. Fahey, S. S. Spnier and R. A. Vander Griend, “Osteosarcoma of the Pelvis. A Clinical and Histopathological Study of Twenty Five Patients,” The Journal of Bone & Joint Surgery, Vol. 74, No. 3, 1992, pp. 321-330,
- W. F. Taylor, J. C. lvins, D. C. Dahlin, et al., “Trends and Variability in Survival from Osteosarcoma,” Mayo Clinic Proceedings, Vol. 53, No. 11, 1978, pp. 695-700,
- S. S. Beilack, B. Kempf-Bielack, G. Delling, et al., “Prognostic Factors in High Grade Osteosarcoma of the Extremities or Trunk: An Anlaysis of 1702 Patients Treated Onneoadjuvant Cooperative Osteosarcoma Study Group Protocols,” Journal of Clinical Oncology, Vol. 20, No. 3, 2002, pp. 776-790. doi:10.1200/JCO.20.3.776
- L. D. Wurtz, T. D. Peabody and M. A. Simon, “Delay in the Diagnosis and Treatment of Primary Bone Sarcoma of the Pelvis,” The Journal of Bone & Joint Surgery, Vol. 81, No. 3, 1999, pp. 317-325.
- R. J. Grimmer, S. R. Carter, R. M. Tillman, et al., “Osteosarcoma of the Pelvis,” The Journal of Bone & Joint Surgery, Vol. 81, 1999, pp. 796-802. doi:10.1302/0301-620X.81B5.9241
- W. F. Enneking, W. Dunham, M. C. Gebhardt, M. Malawer and D. J. Pritchard, “A System for the Functional Evaluation of Recontructive Procedures after Surgical Treatment of Tumors of the Musculoskeletal System,” Clinical Orthopaedics and Related Research, Vol. 286, 1993, pp. 241-246.
- W. F. Enneking, S. S. Spanier and M. A. Goodman, “A System for the Surgical Staging of Musculoskeletal Sarcoma,” Clinical Orthopaedics and Related Research, Vol. 153, 1980, pp. 106-120.
- M. I. O’Connor and F. H. Sim, “Salvage of the Limb in the Treatment of Malignant Pelvic Tumors,” The Journal of Bone & Joint Surgery, Vol. 71, No. 4, 1989, pp. 481- 494.
- W. F. Enneking and W. K. Dunham, “Resection and Reconstruction for Primary Neoplasms Invovling the Innominate Bone,” The Journal of Bone & Joint Surgery, Vol. 60, No. 6, 1978, pp. 731-746
- J. P. Kouie, T. A. M’Bengue, J. Andoh, et al., “Pelvic Osteosarcoma: Problems in Management,” Medical and Pediatric Oncology, Vol. 22, No. 3, 1994, pp. 204-207. doi:10.1002/mpo.2950220310
- P. Bieling, N. Rehan, P. Winkler, et al., “Tumor Size and Prognosis in Aggressively Treated Osteosarcoma,” Journal of Clinical Oncology, Vol. 14, No. 3, 1996, pp. 848- 858.
- L. D. Wurtz, T. D. Peabody and M. A. Simon, “Delay in the Diagnosis and Treatment of Primary Bone Sarcoma of the Pelvis,” The Journal of Bone & Joint Surgery, Vol. 81, No. 3, 1999, pp. 317-325.
- B. H. Pollock, J. P. Krischer and T. J. Vietti, “Interval between Symptom Onset and Diagnosis of Pediatric Solid Tumor,” Journal of Pediatrics, Vol. 119, No. 5, 1991, pp. 725-732. doi:10.1016/S0022-3476(05)80287-2
- A. J. Abuolafia, R. Buch, J. Mathews, W. Li and M. M. Malawer, “Reconstruction Using the Saddle Prosthesis Following Excision of Primary and Metastatic Periacetabular Tumors,” Clinical Orthopaedics and Related Research, Vol. 314, 1995, pp. 203-213.
- R. S. Bell, A. M. Davis, J. S. Wunder, T. Buconjic, McGoveran and A. E. Gross, “Allograft Recontruction of the Acetabulum after Resection of Stage-IIB Sarcoma, Intermediate-Term Results,” The Journal of Bone & Joint Surgery, Vol. 79, No. 11, 1997, pp. 1663-1674.
- A. Abudu, R. J. Grimmer, S. R. Cannon, S. R. Carter and R. S. Sneath, “Reconstruction of the Hemipelvis after the Excision of Malignant Tumors. Complications and Fuctional Outcome of Prostheses,” The Journal of Bone & Joint Surgery. American Volume, Vol. 79, No. 11, 1997, pp. 773-779. doi:10.1302/0301-620X.79B5.6749
- R. Capanna, J. R. Van Horn and N. Guernelli, “Complications of Pelvic Resections,” Archives of Orthopaedic and Trauma Surgery, Vol. 106, No. 2, 1987, pp. 71-77. doi:10.1007/BF00435417
- R. B. Stephenson, H. Kaufer and F. M. Hankin, “Partail Pelvic Resection as an Alternative to Hindquarter Amputation for Skeletal Neoplasms,” Clinical Orthopaedics and Related Research, Vol. 242, 1989, pp. 201-211.
- M. Campanacci and R. Capanna, “Pelvic Rescetions: The Rizzoli Institute Experience,” Orthopedic Clinics of North America, Vol. 22, No. 1, 1991, pp. 65-86.
- B. G. I. Spiegelberg, K. Gokaraju, M. T. Parratt, A. M. Flanagan, S. R. Cannon and T. W. R. Griggs, “Late Recurrence of Pelvic Osteosarcoma: A Case Report and Review of the Literature,” Grand Rounds, Vol. 10, 2010, pp. 8-12.
- K. D. Harrington, “The Use of Hemipelvic Allografts for Reconstruction after Wide Resections of Malignent Tumors of the Pelvis,” The Journal of Bone & Joint Surgery. American Volume, Vol. 74, No. 3, 1992, pp. 331-341.
- C. F. Lord, M. C. Gebhart, W. W. Tomford and H. J. Mankin, “Infection in Bone Allografts. Incidence, Nature and Treatment,” The Journal of Bone & Joint Surgery Infection in Bone Allografts. Incidence, Nature and Treatment, Vol. 70, No. 3, 1998, pp. 369-376.
- A. Uchida, A. Myoul, N. Araki, H. Yoshikawa, T. Ueda and Y. Aoki, “Prosthetic Reconstruction for Periacetabular Malignant Tumors,” Clinical Orthopaedics and Related Research, Vol. 326, 1996, pp. 238-245. doi:10.1097/00003086-199605000-00029
- R. Windhager, J. Karner, H. P. Kutschera, P. Polterauer, M. Salzer-Kuntschik and R. Kotz, “Limb Salvage in Periacetabular Sarcoma: Review of 21 Consecutive Cases,” Clinical Orthopaedics and Related Research, Vol. 331, 1996, pp. 265-276. doi:10.1097/00003086-199610000-00038
- P. K. Jaiswal, W. J. S. Aston and R. J. Grimer, “PeriAcetabular Resection and Endoprosthetic Reconstruction for Tumorurs of Acetabulum,” The Journal of Bone & Joint Surgery, Vol. 90, No. 9, 2008, pp. 1222-1227. doi:10.1302/0301-620X.90B9.20758
- G. Bacci, S. Ferrari, A. Longhi, D. Mellano, S. Giacomini and C. Forni, “Delay in Diagnosis of High-Grade Osteosarcoma of the Extermity. Has It Any Effect on the Stage of Disease?” Tumor, Vol. 86, No. 3, 2000, pp. 235-237.
- A. J. Abouolafia and M. M. Malawer, “Surgical Management of Pelvic and Extremity of Osteosarcoma,” Cancer, Vol. 71, Suppl. 10, 1993, pp. 3358-3366. doi:10.1002/1097-0142(19930515)71:10+<3358::AID-CNCR2820711738>3.0.CO;2-O
- T. Ozaki, S. Flege and M. Kevric, “Osteosarcoma of the Pelvis: Experience of the Cooperative Osteosarcoma Study Group,” Journal of Clinical Oncology, Vol. 21, No. 2, 2003, pp. 334-341. doi:10.1200/JCO.2003.01.142
NOTES
*This study was supported by a grant from Kosin University College of Medicine (2011).
#Corresponding author.

