Post-Varicella Disciform Keratitis: Case Report
84
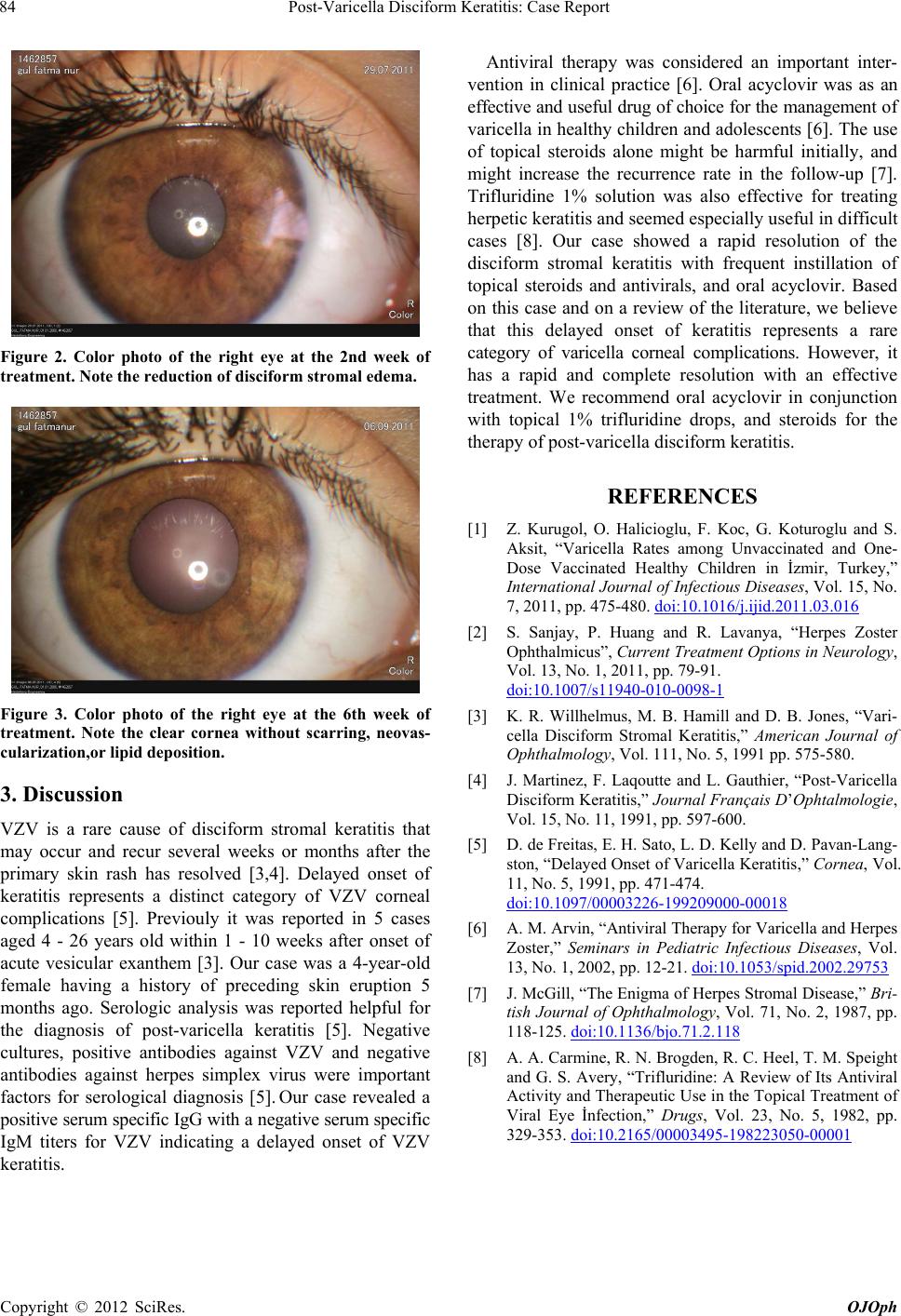
Figure 2. Color photo of the right eye at the 2nd week of
treatment. Note the reduction of disciform stromal edema.
Figure 3. Color photo of the right eye at the 6th week of
treatment. Note the clear cornea without scarring, neovas-
cularization,or lipid deposition.
3. Discussion
VZV is a rare cause of disciform stromal keratitis that
may occur and recur several weeks or months after the
primary skin rash has resolved [3,4]. Delayed onset of
keratitis represents a distinct category of VZV corneal
complications [5]. Previouly it was reported in 5 cases
aged 4 - 26 years old within 1 - 10 weeks after onset of
acute vesicular exanthem [3]. Our case was a 4-year-old
female having a history of preceding skin eruption 5
months ago. Serologic analysis was reported helpful for
the diagnosis of post-varicella keratitis [5]. Negative
cultures, positive antibodies against VZV and negative
antibodies against herpes simplex virus were important
factors for serological diagnosis [5]. Our case revealed a
positive serum specific IgG with a negative serum specific
IgM titers for VZV indicating a delayed onset of VZV
keratitis.
Antiviral therapy was considered an important inter-
vention in clinical practice [6]. Oral acyclovir was as an
effective and useful drug of choice for the management of
varicella in healthy children and adolescents [6]. The use
of topical steroids alone might be harmful initially, and
might increase the recurrence rate in the follow-up [7].
Trifluridine 1% solution was also effective for treating
herpetic keratitis and seemed especially useful in difficult
cases [8]. Our case showed a rapid resolution of the
disciform stromal keratitis with frequent instillation of
topical steroids and antivirals, and oral acyclovir. Based
on this case and on a review of the literature, we believe
that this delayed onset of keratitis represents a rare
category of varicella corneal complications. However, it
has a rapid and complete resolution with an effective
treatment. We recommend oral acyclovir in conjunction
with topical 1% trifluridine drops, and steroids for the
therapy of post-varicella disciform keratitis.
REFERENCES
[1] Z. Kurugol, O. Halicioglu, F. Koc, G. Koturoglu and S.
Aksit, “Varicella Rates among Unvaccinated and One-
Dose Vaccinated Healthy Children in İzmir, Turkey,”
International Journal of Infectious Diseases, Vol. 15, No.
7, 2011, pp. 475-480. doi:10.1016/j.ijid.2011.03.016
[2] S. Sanjay, P. Huang and R. Lavanya, “Herpes Zoster
Ophthalmicus”, Current Treatment Options in Neurology,
Vol. 13, No. 1, 2011, pp. 79-91.
doi:10.1007/s11940-010-0098-1
[3] K. R. Willhelmus, M. B. Hamill and D. B. Jones, “Vari-
cella Disciform Stromal Keratitis,” American Journal of
Ophthalmology, Vol. 111, No. 5, 1991 pp. 575-580.
[4] J. Martinez, F. Laqoutte and L. Gauthier, “Post-Varicella
Disciform Keratitis,” Journal Français D’Ophtalmologie,
Vol. 15, No. 11, 1991, pp. 597-600.
[5] D. de Freitas, E. H. Sato, L. D. Kelly and D. Pavan-Lang-
ston, “Delayed Onset of Varicella Keratitis,” Cornea, Vol.
11, No. 5, 1991, pp. 471-474.
doi:10.1097/00003226-199209000-00018
[6] A. M. Arvin, “Antiviral Therapy for Varicella and Herpes
Zoster,” Seminars in Pediatric Infectious Diseases, Vol.
13, No. 1, 2002, pp. 12-21. doi:10.1053/spid.2002.29753
[7] J. McGill, “The Enigma of Herpes Stromal Disease,” Bri-
tish Journal of Ophthalmology, Vol. 71, No. 2, 1987, pp.
118-125. doi:10.1136/bjo.71.2.118
[8] A. A. Carmine, R. N. Brogden, R. C. Heel, T. M. Speight
and G. S. Avery, “Trifluridine: A Review of Its Antiviral
Activity and Therapeutic Use in the Topical Treatment of
Viral Eye İnfection,” Drugs, Vol. 23, No. 5, 1982, pp.
329-353. doi:10.2165/00003495-198223050-00001
Copyright © 2012 SciRes. OJOph