Health
Vol.5 No.5(2013), Article ID:31970,15 pages DOI:10.4236/health.2013.55127
Iodine deficiency and women’s health: Colonialism’s malign effect on health in Oromia region, in Ethiopia
![]()
Toronto Public Health, Toronto, Canada; b.dugassa@utoronto.ca
Copyright © 2013 Begna Dugassa. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 25 August 2012; revised 6 October 2012; accepted 25 October 2012
Keywords: Iodine Deficiency Disorders; Women’s Reproductive Health; Capacity Building; Gender Equity; Health in Oromia; Ethiopia; Colonialism and Public Health
ABSTRACT
Objectives: Iodine is an essential nutrient needed for the synthesis of hormone thyroxin. Hormone thyroxin is involved in the metabolism of several nutrients, the regulation of enzymes and differentiation of cells, tissues and organs. Iodine deficiency (ID) impairs the development of the brain and nervous system. It affects cognitive capacity, educability, productivity and child mortality. ID hinders physical strength and causes reproductive failure. The objective of this paper is to explore if the health impacts of ID are more common and severe among women. Design: Using primary data (notes from a visit) and secondary data, this paper examines if the effects of ID are more common and severe among Oromo women in Ethiopia. Findings: The health impacts of ID are more common and severe among women. Conclusions: ID is an easily preventable nutritional problem. In Oromia, the persistence of ID is explained by the Ethiopian government’s colonial social policies. Preventing ID should be seen as part of the efforts we make to enhance capacity building, promote health, gender equity and social justice. Implications: Iodine deficiency has a wide range of biological, social, economic and cultural impacts. Preventing ID can be instrumental in bringing about gender equity and building the capacity of people.
1. INTRODUCTION
Iodine Deficiency (ID) is one of the longstanding and widespread public health problems in Oromia and surrounding regions [1-3] and elsewhere in the world. All European countries, with the exception of Iceland, have experienced ID and its health and socioeconomic effects to a greater or lesser degree [4]. ID is known as an easily preventable cause of mental retardation. Directly and indirectly, ID causes reproductive failure and affects educability and productivity. It affects the capacity of people, their human resources development (i.e. intellectual, social) as well as economic and cultural progress, which are essential for the development of public health.
In Oromia, Iodine Deficiency Disorder (IDDs) which refers to a wide spectrum of clinical, social, economic, cultural and intellectual declines is a major public health problem and it is one of obstacles to the socio-economic progress [1,2]. Severe ID during pregnancy can result in stillbirth, spontaneous abortion, congenital abnormalities including cretinism and an irreversible form of physical disability. In Ethiopia, the probability of children dying before they celebrate their fifth year birthday is 104 per one thousand live births. The maternal mortality rate is 470 per hundred thousand [5]. For the neighbouring, country of Kenya, where the salt is iodized, the under five-year child mortality rates are 84 per hundred thousand [6]. In 1995, all the salts sold in Kenya were iodized. At that time, less than 5 percent of the people in Ethiopia had access to iodized salt [2].
Iodine is one of the essential nutrients critically needed for the synthesis of thyroid hormone. The major physiological functions of iodine are linked to the synthesis of thyroid hormones. Thyroid hormone is involved in the regulation of various enzymes and metabolic processes of protein, carbohydrate, fat, minerals and vitamins. Thyroid hormone is involved in the differentiation of several organs, systems, tissues and cells [7]. Iodine is required for several essential physiological functions of all mammals [8]. If inadequate amounts of dietary iodine are ingested, several essential physiological functions are impaired. For example, the central nervous system (brain, and spinal cord) that governs the sensory and motor functions of the body and all the embryos of mammals rapidly grow these critical organs. ID affects the growth and development of the brain, spinal cord and nervous system of the fetus [9]. Dietary iodine is one of the nutrients that do not accumulate in body tissues. This necessitates a steady lifetime supply of iodine [10].
This paper has four major parts. The first part covers the introduction, background, research problem, objective of the study and theoretical framework. The second part covers data mining. Under this, the ways in which the Oromo people have conceptualised ID and the social conditions that contribute to the problem are examined. In the fourth part, the public health impacts of ID and the ways in which it affects women’s health are explored. The last part covers discussions and conclusions.
2. BACKGROUND
In research, introducing the context in which the study is conducted helps to clarify any ambiguity and serves to help the reader better comprehend the root causes of the problem. Providing background and context in which an event occurred, or is occurring, makes it easier to understand the conditions that have generated the question under investigation and hints at what we need to take into consideration. We can fully understand the public health conditions of a society if we comprehend the social setting in which the people live. Social settings are determined by political power and we cannot understand the former without understanding the latter.
The Oromo people have been under Ethiopian colonial rule for over a century [11-13]. The colonial agenda is driven both by the theory of racial superiority and economic interests. Colonialists impose the will of the colonizing people on the colonized and use the resources of the imposed people for the benefit of the imposer [14]; doing that limits the choice of the colonized people. Colonialism is a violation of the collective rights of people. Under Ethiopian colonial rule, the collective rights (i.e. social, economic, political, cultural and environmental) of the Oromo people have been violated. These violations have impaired the social, economic, political, cultural and environmental capacity of the Oromo people [15]. These social conditions have kept the Oromo people in poverty [16], illiteracy and conditioned them to famine [17,18], exposed them to HIV/AIDS infection [19] and several micro and macro nutrient deficiencies.
Iodine is a trace element that belongs to group seven elements of periodic table also known as the halogens family, which is a highly reactive non-metal. Iodine easily dissolves in water, evaporates in the sun, then condenses in the atmosphere and returns back to the earth in the form of rain and snow [20,21]. When the earth’s crust was formed, there was ample iodine. However, glaciations during the Ice Age exposed the deeper iodine-rich layers of the soil to rain, snow and wind. This has caused snow and rain to wash off most iodine from the surface soil and carry it to the sea by wind, rivers and floods. As a result, iodine is found in large amounts in the sea and lakes [20]. Soil in the coastal regions of the world is richer and the fruits and vegetables harvested from those areas contain more iodine. Iodine rich foods are fish, seaweed and kelp [21]. Moderate amounts of iodine are found in eggs, milk, and meat [22]. ID is more prevalent among populations who live in regions where the soil is eroded because of glaciation and further eroded by heavy snows, rainfalls and river flooding [23].
2.1. Research Problems
The most visible effect of ID is goiter, which represents the enlargement of the thyroid gland. Goiter is more prevalent among women than men. The size of the goiter increases as girls reach puberty and can continue to grow during the childbearing age. If a woman suffers from ID, the size of the thyroid gland enlarges during pregnancy and the menstrual cycle. However, for young men the severity of IDDs slows down as they reach puberty [1]. ID is one of the major causes of reproductive failure and mental retardation. Clinical research in ID sensitivity has made it clear that female fetuses are more sensitive than male ones [24-26].
The recommended dietary iodine allowance varies based on age, gender and physiological conditions. The daily recommended dietary iodine intake is high for pregnant women (220 µg/day) and breast-feeding mothers (290 µg/day); for other adults it is 150 µg/day. For growing children, it is 90 µg/day; for infants to six years and for school children, it is 120 µg/day [27]. The higher recommended iodine allowance level for pregnant and breast feeding mothers, suggests that women are at higher risk of ID. A person who lives to age 85, requires one teaspoon of iodine in his/her lifetime; this costs annually about three cents per person.
Twenty-five years after the author left his home village, he observed that ID became widespread public health problem. In this paper he asks, and try to answer the following questions: 1) what are the social conditions that aggravate ID? 2) if ID is more common and severe among women, if it damages brain and affects educability and the cognitive capacity of children, does this contribute to the differences in educational achievement of men and women? If the ID contributes to reproductive failure and physical impairment, has this contributed to lowering the social status of women? If the answers to these questions are yes, why has the Ethiopian government failed to iodize salt and continue to commit a public health malpractice?
2.2. Objective of the Study
Public health literature clearly suggests that unfair distribution of power is an obstacle to the improvement of public health conditions. Changing the distribution of power and creating social conditions where individuals and groups can represent themselves, identify their needs, fairly distribute the privileges and the risks of the society [28] are essential to promote health. Changes in power relations include freedom from colonial power relations, gender and class structural orders. Empowered people have a greater sense of control over their lives and can effectively build their capacity and prepare themselves to solve their current and future social and public health problems. The major objective of this paper is to examine if the health effects of ID are more common and severe among women.
In public health, the concept of capacity building focuses on understanding the obstacles that inhibit people from realizing their public health goals and enhancing the ability of people so they can achieve measurable and sustainable results [29]. The protein-energy malnutrition, micronutrient and trace elements nutritional deficiencies, premature death and reproductive failure as well as other public health problems in Oromia seem to result from a sequence of interlinked social and economic colonial policies of the Ethiopian government [18]. Those policies determine whether or not the Oromo people have food security and are entitled to fortify1 their foods and prevent nutritional deficiencies. The second objective is to take a close look at the social causes that have led to ID and its impacts.
2.3. Description of Study Setting
This research paper is about IDDs in the Oromia region in Ethiopia. Oromia is one of the nine ethno-national states in Ethiopia. As seen on the map below Figure 1, Ethiopia in general and Oromia in particular is a landlocked country. IDD literature suggests that as the distances from the sea increase, the concentration of iodine in the soil decreases [20]. Consistent with the literature in Oromia, IDDs are more common and severe in western Oromia than in the eastern and the southern parts of the country. IDD is more common in low-
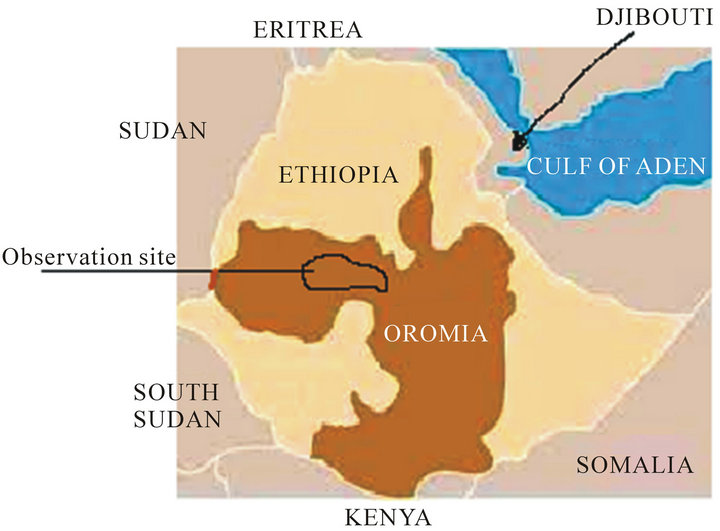
Figure 1. Oromia and surrounding regions.
land regions than in the highland regions [1]. The data collection was done in the highlands of Western Oromia (Eastern Wellega) and in Central Oromia (Western Shewa).
2.4. Theoretical Framework
The biomedical approach to health and diseases helped us to understand many public health problems and find workable solutions. However, it has serious limitations in helping us to understand the disease process and the social causes of the problem. Without understanding the social process of the problem and having proper social policies in place, simple biomedical discoveries cannot improve public health problems and sustain improvement. Social and political changes, fair disbursement of common privileges and burdens as well as the presence of enabling environments are necessary to improve public health conditions [30-32]. From the social theory of knowledge construction, it is clear that most research questions are framed from the perspective of researchers and social policies are designed in the interests of policy makers. This necessitates critically looking at the framework in which research questions are asked and the perspectives from which the policies are framed.
There is no single theory that is neutral and universally acceptable, and that can be used in analyzing all social issues [33]. It is for this reason that different theories are continuously constructed to explain, predict and analyze phenomena. The theoretical framework of research serves as a tool to ask specific questions, see issues with specific lenses, construct realities and envision solutions. Theoretical concepts provide the lenses through which we can see a symbolic representation of abstract ideas. Choosing the appropriate theoretical framework provides an analytical tool and helps us to emphasise certain issues.
The WHO defined health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [34] and I choose to frame this paper from the perspective of Oromo women, because they shoulder double burdens. Malnutrition affects women and children more severely and asking research questions and setting social policies from their perspective eases the suffering not only of women but of people as a whole. Oromo women are part of the larger Oromo society. When the Oromo people suffer, the health of Oromo women usually deteriorates. In asking questions and analysing data from the Oromo women’s perspective, I make use of the historical colonial practices as well as systemic discriminatory social policies and practices that Oromo people and Oromo women are subjected to.
Oromo women are shouldering double burdens [19]. On one hand, as part of the larger Oromo society, they are shouldering the burden of the colonial power relations. On the other hand, they experience male domination. In public health, it is well known that the presence of freedom helps life to flourish and determines whether or not a person or group will enjoy good health.
3. DATA MINING
It has been generally agreed that the social location of researchers influences the research questions they ask and the ways they collect data and interpret it [14,35]. The author was born and raised among the Oromo people. For over a decade, he did research on public health issues that are relevant to the Oromo people. He has contacts with family members and friends. As a public health nutrition practitioner and researcher, the author believes the biomedical model and “band-aid” solutions treat the symptom of the problems rather than the root causes. To shed light on the health effects of iodine deficiency, the author applied the “upstream” public health principle to capture data, analyse, correlate and then integrate it with secondary data.
First, among the Oromo people, ID has been known from time immemorial. The authors’ knowledge regarding ID is not only explicit knowledge that he acquired from Nutritional Sciences studies but also comes from the tacit knowledge that he acquired from lived realities. In 2010, the author visited his home village and the surrounding regions. At that time the author had just completed a project intended to establish the causes of ID in Oromia in general [1]. Until the author arrived in his home village, he assumed that the project was about those who live in lowland areas.
Observation is one of the ways of gathering data; it is done by watching events and social conditions in their natural setting. Observations can be overt or covert. The benefit of covert observation is that people are more likely to behave naturally if they do not know they are being observed [36]. The author of this paper knows the region very well and in his analyses of changes, he used his initial knowledge as the baseline. When the author arrived in his home village, he had no plan to conduct research. As Louis Pasteur said, “chance favours only the prepared mind”, when he noticed the signs of ID and ID causing conditions were widespread, the author opened his mind, eyes and ears to see and hear as well as observe. Following that he started to take notes. To clarify some of the issues, he engaged in indirect conversations with the elderly men and women whom he met on the street, restaurants and coffee shops. He went to market places to observe and identify any indicators of ID. On the street when he goes out for walk, he looked for any signs of ID among children and adults. Hence, the data collection was done by observation in an informal way.
When the author was young, he saw no single woman with goiter, visible at a distance, in his home village. He only saw it among those women in the lowland regions. However, 25 years later when the author returned back to his home village, he noticed several women with goiter. He noticed the widespread deforestation, soil erosion and signs of desertification [37]. Fertilizers and herbicides were widely used. Access to clean water was critically limited and many sources of spring water that traditionally provided drinking water were dried-up and now people depended on bigger rivers. The home where the author stayed in a town was not far away from a health clinic. Practically every day, he noticed a group of men caring pregnant mothers who were having complications in birthing bring to the clinic. To learn more about the magnitude of the problem, the author talked to local health professionals. He found out that the problem is a wide spread.
As part of data collection, instead of giving a small amount of money to street beggars, the author chose to take an elderly street-begging woman to a restaurant for a lunch and an elderly man to a coffee shop for snacks and talked to them. The woman revealed that she had raised five of her own children (three boys and two girls). One after the other, three of her sons was recruited into the government militia (1974-1991) and two of them died in the war front and one returned. Two of her daughters married and lived in a distance places. Few years after her son returned, he was charged with being a supporter of the Oromo Liberation Front (OLF) and imprisoned. While her son was still in prison, her husband died. This left her with no men to plough the land. Ethiopian government policy suggests that, if the farm lands are not properly used, it will be given to someone else. As a result, she lost her land.
The elderly cattle breeders complain that their cows are not producing enough milk, their growth is slowed, reproduction age is delayed, the gaps between gestation periods have increased and physically they have become unusually small and weak. The author observed that the poverty level was unusually high. Until recently in Oromo, begging was a taboo. However, things have been changed and many men, women and children have become street beggars. Another critical change noticed was since immemorial times, the authors’ home village was malaria free; now, it has turned into a malaria prone zone. When the author saw those realities and heard those stories and also personally observed them, several questions emerged in his mind. What are the social conditions that aggravated ID in Oromia? Understanding the relationships between ID, educability, productivity and reproductive failure, the other question that emerged in the mind of the author was what are the impacts of ID on women’s health and the poverty level? Do the Ethiopian government and international organizations understand that the prevention of ID is a critical step in promoting equity and building public health capacity?
Second, since 1992, the author is an active member of the Oromo Studies Association (OSA). Since 2000 he have been researching and writing on public health issues that are relevant to the Oromo people. At the OSA conferences, the author regularly presents papers and listens to the presentations of others. This has provided him a unique opportunity to better understand the social dynamics and public health problems in Oromia. Clearly, this helped the author to integrate and correlate public health problems in Oromia with the social conditions and political status of Oromo people.
Third, the author is knowledgeable that ID is an easily preventable public health problem. ID is the single largest cause of mental retardation such as cretinism and congenital abnormalities [28,38]. It also causes endemic goiter, hypothyroidism, a decreased fertility rate (miscarriages, stillbirths, preterm deliveries), and increased infant mortality [39,40]. The poverty level the author observed in his village and the stories he heard from farmers and health professionals clearly correlate with information in the literature.
Fourth, the author is influenced by newly emerging findings in iodine metabolism. Much of our present knowledge regarding ID is based on biomedical sciences and it lacks the social aspects such as gender, age, social status and political power relations. Now it is clear that ID is more common among people who live by subsistence farming. Several clinical studies also suggest that there are gender differences in iodine metabolism. The effects of ID are more severe in females [24-26,41]. The experimental studies conducted by Chan [24] and his colleagues clearly suggest that the female fetus is more sensitive in its cognitive development to maternal ID than is the male. In developing countries, iodine deficiency is seen as an obstacle to women’s achievement [42]. For the Oromo people, the major dietary iodine sources are meat, milk, and eggs. If they lose those sources and become conditioned to consume goiterogenic foods, they are at greater risk to suffer from ID [1]. If the experimental findings of Chan and others were true for humans then female fetuses are more sensitive, in their cognitive development, to ID. This might contribute to the differences in educational achievements between men and women. If dietary iodine is indeed a key to human cognitive capacity, it has major consequences to national and community development.
Fifth, iodine helps the body to detoxify and remove toxic chemicals such as mercury, fluorides, chlorides, and bromide compounds. Given that herbicide and fertilizers are widely used and the availability of clean water is very limited, most of the people are at risk of ingesting chemical toxins. In addition, in the Rift Valley region of Oromia, the fluoride level in soil and water is very high and it is one of the long-standing public problems [43,44]. If those who live where fluoride toxicity is endemic while others were ensured an adequate intake of iodine, it would have helped the latter to detoxify the fluoride and other toxic halides such as bromide and chlorinated compounds.
4. KNOWLEDGE CONSTRUCTION IN ID PREVENTION
The history of knowledge construction in ID and prevention practices offers an instructive example of transferring traditional practices to scientific discovery in public health. In China, for centuries seaweed has been used to prevent goiter. In an effort to understand the mechanism by which seaweed prevents ID, in the 1820s iodine was identified in seaweed [45,46]. Iodizing table salt, as a means of providing prophylaxis against IDDs, was first suggested in 1831. The first experiment in prophylaxis against IDDs was carried out in France. In this experiment, 100 mg of potassium iodide was given daily to humans. However, the experiment failed due to its toxic symptoms [47]. The concentration of iodine used was higher than the amount that humans can safely metabolize and the initial efforts failed. The first successful large-scale trial with iodine supplement was carried out in 1922 in Michigan, USA [23,48]. Two years later, for the first time iodized salt was used on large scale in goiter prevention efforts in Michigan and in Switzerland [23,46]. Following Michigan State and Switzerland, all US states and other countries iodized their table salt and were able to fully eliminate IDDs [48].
The evidence that supports the idea that ID causes endemic goiter, mental retardation, and reproductive failure is based on four separate research findings: 1) the correlation between a low iodine content in food and water and the appearance of IDDs in the population; 2) the sharp reduction in the incidence of IDDs when iodine is added to the diet; and 3) the experimental demonstration that the metabolism of iodine by patients with endemic goiter fits the pattern that would be expected from ID and is reversed by iodine repletion;4) lastly, ID causes major changes in the sizes and functions of thyroid glands of mammals that are similar to those seen in humans [49, 50]. Iodine is crucial in the differentiation of organs, tissues and cells, if an inadequate amount of iodine is consumed, several physiological functions can be impaired.
4.1. Pathological Social Conditions and IDDs in Oromia
If disease is an expression of individual life under unfavorable circumstances, then epidemics must be indicative of mass disturbances. Virchow cited in [51].
The above quote is from the works of Virchowthe father of social medicine. He made the statement after he had investigated the causes of typhus epidemics in Upper Silesia-whose inhabitants were predominately Polish but ruled by the Germans. From this study he concluded that all diseases are caused by the social conditions in which people live. Virchow’s work made it clear that epidemics are the biological markers of the social conditions in which people live and he established the relationships between colonialism and public health. Virchow`s and his work suggests the need to go beyond biochemical indicators of IDDs and investigate the pathological social conditions that contributed to it.
In agreement with Virchow, the WHO Commission on Social Determinants of Health [28] emphasized that social factors such as poverty, inadequate housing and lack of education were the real root instigators and the underlying proximal causes of morbidity and mortality in many countries. The commission’s report made it clear that the demand for social justice is not a luxury; it is about a choice between life and death. The commission highlighted the idea that the empowerment of women is critical in achieving fair distribution of health and preventing health disparities. Using the analogy of Virchow and WHO the nutritional status of the Oromo people has the potential to reveal the biological impacts of colonial power relations and discriminatory social practices of the Ethiopian government.
In Oromia, poverty, famine and protein-energy as well as several micronutrient deficiencies are not simply caused by simple natural calamities but caused by unjust political power relations [19]. Indeed, it is known that famine more often occurs in a dysfunctional society where there are unjust social relations [50]. According to Sen [52], political freedom is an essential condition to free people from hunger. Poverty and hunger are not different from torture [53] and the struggle of the Oromo people to self-determination is part of their struggle for food security and liberty [19]. Indeed, in Oromia the prevention of ID and protein-energy malnutrition requires multilateral actions and requires a considerable political power change.
Most Oromo people are farmers. A majority of them are settled in highland and semi-highland regions of the Horn of Africa and they had no, or limited, access to seafood. Oromo oral history suggests that in the past, salt was a highly valuable commodity. Currently 95 percent of the Oromo people have no access to iodized salt and more than 75 percent of them have no access to clean water [54]. In the Oromo language, goiter is known as Kulkuula Morma (bump of neck) or Quufa Morma (satiated neck). The Oromo people understood that drinking polluted water, poverty and eating corn cause goiter. The Oromo oral history suggests that the prevalence of goiter is higher among poor pregnant women and among those communities in lowland regions who are dependent on pond water where many carnivorous birds inhabit. The story suggests that the intestinal discharges and secretions of carnivorous birds leached to ponds and rivers cause goiter for consumers of the water [1].
Although there are no complete data, a few published documents suggest that the prevalence of goiter varies from one part of Oromia to another. In most cases, the distribution of IDDs in Oromia is similar to that of other countries in that the problem is more in inland areas than in coastal regions. As the distance from the sea or coastal region increases, the magnitude of the IDDs escalates. Cattle breeders are less affected by IDDs than are exclusive agriculturalists. Except for the region where the soil fluoride level is high, IDDs are rarely seen among nomadic people. However, consistent with the Oromo oral story, IDDs are more prevalent in lowland regions of Oromia than in the highland ones [1].
In Oromia, the prevalence of IDD is very high. The prevalence of IDD has been increasing since records have been kept. In 1986, 80% of salt was iodized [1,55]. However, from 1999 on, only 5 percent of the salts available in Ethiopia were iodized. As is demonstrated in Figure 2, in Oromia the prevalence of goiter is more common among women and young girls, than it is among men and young boys. As the boys’ ages increase, the IDD level slightly decreases; however, when it comes to the young girls as they get to puberty and motherhood, the prevalence of IDD increases.
The geographical proximity of Oromia in relation to the seacoast has contributed to iodine deficiency. The iodine content of soil changes as the distance from the sea increases [56]. For this reason in Western Oromia the prevalence of IDDs is higher than it is in the Eastern and Central regions. However, if the Oromo people were empowered, iodizing salt would have controlled this natural phenomenon. As presented in Figure 2, ID and
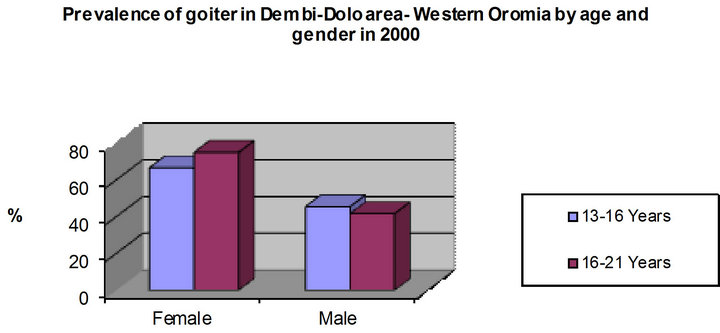
Figure 2. The prevalence of goiter in western oromia—by age and gender in 2000. The graph is based on data produced by the World Health Organization [57].
several easily preventable diseases are the manifestation of the violations of positive and negative freedoms. Violation of such rights is denying the people the opportunity to build their capacity, identify their needs and tackle their problems.
4.2. Human Rights as Social Medicine
The social determinants of health theory and practice opened up the possibility of identifying the social policies or conditions that impair or improve health. As Virchow’s work revealed, [51] if all public health problems are manifestations of the social conditions in which the people live, critical analyses of the social conditions in which the Oromo people live can reveal the root causes of their problems. Understanding the connections between the social conditions in which the Oromo people live and iodine deficiency can allow us to control or modify those conditions. This brings me to the next question. How does the presence or absence of liberty and freedom affect public health conditions in Oromia in general and ID in particular?
There are two theories that explain the concepts of liberty and freedom. Isaiah Berlin [58,59] made distinctions between “negative” and “positive” theories of freedom. The negative theories of freedom entail the freedom of individuals and groups from interference by the state or institutions. However, the positive theory of freedom sees freedom as not necessarily the presence or absence of interference, but rather the preparedness of the person and the group to live up to their potential. Both rights are essential for individuals and groups to be free from hunger and constantly improve their quality of life. Respect for the negative rights creates conditions for individuals and groups to be creative and critical thinkers and helps them achieve their desired goals. On the other hand, respect for positive rights protects citizens from internal vandalism and external forces. In addition, regard for positive rights obligates the state to create favourable conditions for society to grow and flourish. Furthermore, positive rights compel the state to provide educational opportunities and create safe and healthy social conditions. ID is a public health problem that has been known in Oromia for ages. Preventive measures for ID have been known since the 1920s; indeed, it is one of the most easily preventable nutritional problems. The presence of ID in the twenty-first century reveals the relationships between the Ethiopian government and the Oromo people.
Violations of or lack of attention to human rights, can have severe health outcomes (see Figure 3). For this reason, the WHO encourages all member states to integrate the principles of human rights in their social policy in general and public health policy in particular [60]. However, Ethiopian government policies are contrary to the advice of the WHO. In the Ethiopian case, leave alone setting healthy social policy, even foods that the international relief organizations donate are used as tools to incapacitate individuals and groups whom they see merely as opposition [61,62]. This means the causes of famines, protein-energy malnutrition and ID are not simply explained by natural calamities [16,27]. As it is illustrated in Figure 3, these ill health conditions are the manifestation of the violation of the collective rights of the Oromo people and the absence of healthy social policies needed to establish food security and iodize salts.
5. IODINE DEFICIENCY AND REPRODUCTIVE FAILURE IN FARM ANIMALS
Most of the Oromo people are cattle breeders. As is the case for humans, in farm animals severe ID causes a subnormal synthesis of thyroid hormone, which in turn causes reproductive failures such as a high incidence of miscarriage, stillbirths and weak calves [64], irregular heat cycling, low conception rates, retained placentas, decreased libido and semen quality in males [65]. In cattle, ID also causes a higher incidence of physically weak calves [66]. In sheep, it causes not only an increased incidence of miscarriages and stillbirths but also reduced fetus weight, and reduced wool growth, physical body deformations as well as weaker bone development [66]. It causes delayed puberty, poor conception rates, and prolonged gestation periods. ID is also associated with
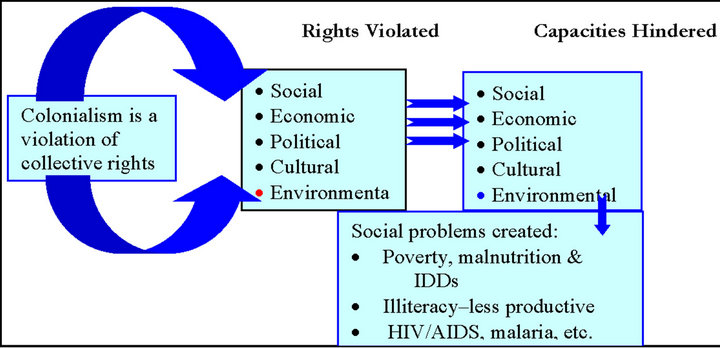
Figure 3. Violation of collective rights, impaired capacity and public health. The graphic is adopted from my work [63].
parturition and retention of placental membranes [64]. Furthermore, ID affects the survival rate of newborn calves. Even if the calves are born normal size, reduced hormone thyroxin levels affect their survival.
In endemic iodine deficient areas, the development of the fetus is not only delayed or arrested at some stage in gestation but also the survival of the newborn is significantly reduced. Their physical weaknesses limit their mobility and hinder them from competing for grazing. From the Oromo perspective, if farm animals are physically weak, this means they plow few plots of lands. The birth of hairless offspring means one of the mechanisms in which animals protect themselves from heat, cold and predators is not developed and this contributes to the early death of calves, lambs, baby goats and others. Indeed, ID is known as an agent that disrupts the normal development of an embryo or fetus. ID influences the growth rate, milk production and their physical strength [62,65]. What does this mean for the Oromo people in general and Oromo women in particular?
If ID causes reproductive failure and reduces the productivity of farm animals, would it affect the health of women? To answer this question, we need to understand the ways ID affects the health of farm animals and the degree to which the Oromo people are dependent on farm animals. Evidence shows that in several ways ID can increase poverty levels. This is clearer among cattle breeders. In its turn an increased poverty level has enormous implication for women’s health. First, in Oromia, meat and milk products are the only source of iodine intake. If ID affects farm animals, it further exacerbates the magnitude of the ID. Second, if ID causes reproductive failure and reduces the survival rates of newborns, it further increases the poverty level. For example, our Oromo farmers use oxen to plow their lands and horses, donkey, mules and camels as means of transportation. If ID affects the productivity and physical strength of farm animals it further exacerbates the food insecurity level. Third, Oromo women have full control of milk and milk products; if ID causes reproductive failure and reduces the productivity of animals, it takes away the material resources over which they have full control.
Fourth, if ID causes reproductive failure, poor conception rates, delays puberty, low productivity, and physical weakness as well as reduces the survival rate of farm animals, it will further increase the poverty level and escalate the burden of destitution among Oromo women. Sixth, Oromo women are expected to feed and care not only for children but also the young calves, lambs and others. If ID causes slow physical growth, weaker bone development and a reduced survival rate of farm animals, it will increase the burden on women of caring for the young animals.
5.1. Iodine Deficiency and Community Capacity Building
What are the relationships between ID and the capacity of people to understand their own problems and solve them? Would the prevention of ID contribute in building the capacity of Oromo women, in better understanding their own societal problems, and finding culturally acceptable and financially feasible solutions? For the Oromo people, mothers are the centres of the family and community; for this reason, asking questions from the perspective of Oromo women, and developing policies from their perspective, is essential in building the capacity of the whole society.
The idea of capacity building entails working on multiple levels, which includes individuals, groups, communities and organizations [29]. The concept of capacity building entails improving each of the individual entities that affect the others. By increasing the capacity of individuals we can strengthen the capacity of the community. In doing that society can progressively build a strong, integrated supportive system. Knowledgeable, capable individuals can build strong, capable organizations and communities. In its turn, strong organizations and communities supported with skilled leadership and resources can share their capacities in coalitions, partnerships and collaborative efforts with other organizations and bring about necessary changes. Clearly ID causes physical and mental retardation, severely affects educability, hinders participation and induces several social, economic and health problems [67]. It is through the power of the mind that human beings are capable of understanding and manipulating their social and natural environments and solving complex problems. If the mental capacities of all members of a society are well developed, they have the potential to be self-sufficient, prevent nutritional deficiencies and improve their quality of life. Hence, ID should be seen not only in terms of its acute effects on individuals and communities but also with regard to its long-term effects. The issue of ID should be seen as one of the lost opportunities in building the capacity of people.
Healthy and well-nourished children are more likely to be educable and productive. Hence, maternal health and raising healthy children is a prerequisite for community capacity building. ID impairs school performance even after the effects of other factors has been taken into account [66]. Through its effects on cognitive capacity and the educability of children, ID affects productivity and human capital development. Cognitive damage from ID slows economic growth and human capacity attainment. Elimination of ID increases human cognitive capacity, educability and productivity as well as reduces health costs [4] and improves community development. As has been shown in laboratory animals, if female fetuses are truly more sensitive in their cognitive development to ID than males, this might contribute to the differences in educational achievements between men and women.
Preventing ID has social, cultural, health and economic benefits. Studies from Germany, India, Latin America and the United States have shown the benefits of interventions to reduce ID [68]. The findings clearly show that by eliminating ID in previously iodine-deficient areas, an increase in cognitive development and economic gain are achieved. Similar economic gains can be achieved by preventing low birth weight children, reproductive failure and child mortality [69]. Another study, in Ecuador, found that people with moderate ID were paid less for agricultural work (Greene, 1977. cited in [70]. More recently, the WHO study groups looked at the cost-effectiveness and benefit-to-cost ratios of micronutrient interventions, nutrient fortification and salt iodization programs; both study groups established very high benefit-to-cost ratios [68,71]. Iodizing salt pays back nine times its cost [42]. Furthermore, given that the mortality risk associated with ID is high, the prevention of IDD offers up to an 8% benefit in child mortality reduction [72]. For the Oromo people who are predominantly cattle breeders, the economic benefit of preventing ID is even higher. In the next section I specifically look at the health effects of ID on women’s health.
5.2. Iodine Deficiency and Women’s Health
Iodine deficiency has long lasting effects on individuals and groups. Woman’s nutritional and health status before and during pregnancy directly contributes to a healthy pregnancy, child health and health in adulthood. A healthy pregnancy contributes to healthy childbirth and healthy birth outcomes. This means that optimizing the nutritional and health status of mothers contributes to the birth of healthy children, healthy families and communities. In Oromia, reproductive health is a crucial part of general public health. ID is one of the major contributing factors to reproductive failure. For example, Abuye and Berhane [73] found that in Ethiopia severe ID is associated with reproductive failure. In their study, they established that women with goiter and those who live in highly goiter endemic areas were more likely to experience reproductive failure, which includes miscarriages and stillbirths than those who live in less endemic regions.
The impacts of ID on reproductive health are immense. Reproductive ill-health accounts for 20% of the global burden for women and 14% for men [74,40]. Prevention of ID has a major role to play in reducing those burdens. A document produced by the Ethiopian Ministry of Health [75] shows that for every day of delay of iodizing salt, another 50,000 infants are born with reduced mental capacity and 50,000 prenatal deaths occur every year. Nevertheless, seven years after the report, 95% of the population still have no access to iodized salt.
According to the WHO standards, if the goiter rate is above 5% it constitutes a public health problem [76]. However, in Ethiopia the goiter rate is about 26% and in some areas the goiter rates reach between 50% and 95% [73]. Published scientific literature shows that in children who are born from mothers suffering from ID, 3% of them exhibit clear severe mental and physical damage, 10% of them show moderate mental retardation, and the others (87%) suffer from some form of mild intellectual disability [77]. In randomized and controlled studies, it has been established that infant survival rates improved in infants born to mothers whose ID is corrected to the recommended intake level before or during pregnancy. In one of such studies there was 72% decrease in the risk of infant death during the first two months of a follow-up [21,76,40].
Hormone thyroxin regulates several enzymes and involves in the metabolism of multiple nutrients and in the differentiation of several important cells, tissues, organs and systems. This means the disorders induced by ID are numerous [7]. The effects of maternal ID have implications for both the fetus and neonate. ID increases the neonatal and infant mortality and reduces overall child survival rates. It may cause birth defects in children or may halt pregnancy outright. ID causes infertility, and increases miscarriage [39]. It has well established that hypothyroidism causes anovulation, gestational hypertension, increased miscarriages, and stillbirths [39,40,77]. Miscarriages and stillbirths in turn cause several health complications for mothers. For example, miscarriages and stillbirths cause bleeding, which can lead to infection, anaemia, physical weakness and mental disturbance. Physical and mental stresses affect the productivity of women and further aggravate the poverty level.
Our health is dependent on our environment. For the fetus, their environment is their mother. The protein, energy and other nutrients required for fetal development are supplied entirely from the mother. This means that children born from malnourished mothers will grow up to be less healthy and productive. Iodine is an essential component of the hormones thyroxin and its inadequate supply diminishes the thyroxin level, the development of the brain of the fetus and causes physical impairment and brain damage [78,79]. Even mild ID can cause a significant loss of learning ability—about 13.5 intelligence quotient points. As a result, ID infringes the rights of children, hinders their productivity and slows the socio-economic progress of a society [2]. If children are born with mild and severe mental retardation or other physical disability, most likely it is the mothers who will have to provide lifetime care, diverting their time and scarce resources.
In addition, ID has cultural and socio-economic consequences for mothers. Given that the potential impact of ID hinders neuro-intellectual development, educability and productivity, it seems that it contributes to lower the social status of women in the community. For example, in Oromia differences in the ratio of boys to girls in primary and secondary educational achievement are well documented [80]. The report reveals that the boys are doing better than the girls. It is most likely that ID has a role in this.
Furthermore, infertility, increased miscarriages, stillbirths and infant mortality caused by ID compromise the status of women, their quality of life and their role in the family and community. Hence, for those who intend to bring equity and reduce health disparities, there is an urgent need to prevent ID.
6. DISCUSSIONS AND CONCLUSIONS
In Oromia, ID is explained not only in terms of the geographical proximity of the region from the coastal areas, but also by the level of soil erosion, poverty levels, denial of leadership and violation of the rights of Oromo people to determine their own affairs [1]. For example, in 2010, during my visit to my home village I observed many women with goiters. In the area there is clear deforestation and signs of desertification [37]. The region was well known for its zebu cattle, sheep, goats, horses, mules and donkeys. Cattle breeders complain about the reproductive failure of their cattle and of their being less productive. Although in Oromo culture it was taboo to beg and now it is becoming a way of life. I observed many elderly men, women and children who are street beggars.
Malnutrition and ID are caused at multi-sectarian levels and we can better understand the problem and address them if we clearly establish the root causes. Preventing nutritional deficiencies and improving public health conditions in Oromia requires assessing the situation, analysing the root causes and mobilizing human and material resources. If the right of people to decide on their affairs is compromised, it makes the assessment, analysing and mobilizing of human and material resources practically impossible. In the case of Oromo women who are experiencing multiple oppressions, the challenges of analysing the causative process, mobilization of human and material resources are formidable. According to WHO [74], there are three major essential conditions necessary to totally prevent ID and eliminate IDDs. These essential conditions include political support, administrative arrangements, and assessments as well as monitoring systems. Political support entails legally prohibiting non-iodized salt in the market. Administrative arrangements mean enforcing the law. Assessment and monitoring systems entail providing scientific data, which includes measuring progress to demonstrate whether or not adequate amounts of iodine are reaching the targeted population. Monitoring requires the selection of appropriate indicators of the salt iodization and packaging process, transportation, storage, usage and its impact. Indeed, progress towards the elimination of IDD or failure can only be established if it is measured. Establishing the law, insuring its implementation and monitoring necessarily involve the government. This makes the prevention of ID, creating reasonable public health conditions and being healthy as rights that individuals and groups need to claim rather than waiting for conditions to change with our prayers.
Much of our present knowledge about ID is framed around the biomedical model, which is more intended to provide a technical fix rather than identifying the social causes and addressing them. The biomedical model does not provide an understanding of the root causes and the social aspect of ID. From the theory of the social determinants of health, the vulnerability theory as well as from the history of public health, we know that under colonial rule public health conditions of the colonized people deteriorate over a period of time or show only a slow improvement. The ID problem in Oromia is a true example of a public health malpractice by a colonial state. Although ID is easily preventable, the Ethiopian government has allowed this public health problem to persist.
Apart from the geological proximity of Oromia from coastal areas, the causes of ID can be explained in five intertwined ways. First, violating the social rights of the Oromo people exposed them to ID. The Ethiopian government attacked the social fabric that maintained the social order, the social relations and social support of the Oromo people. Human beings are social beings, and they look after each other as families, friends and communities. Social support plays a pivotal role in community health [81]. The Oromo people are dependent on each other for their safety. Oromo social relationships ensured its members’ relatively equitable standards of living such as housing, food, water and clothing. Violating the social rights of Oromos has hindered their positive social relationships and the development of the longstanding principles of public good among the Oromo people. As the social values that promote caring and nurturing each other are hindered social conditions of the Oromo people are eroded.
Second, by violating political rights, the Ethiopian government has denied the Oromo people the right to develop their own leadership. The denial of leadership has hindered the Oromo people from identifying opportunities, risks and taking appropriate actions. If the Oromo people are empowered, they would develop a leadership that would be better able to identify what works for them and could have done everything possible to iodize their salts and allocate their human and material resources to address their needs. Despite increasing awareness that ID is widespread in Oromia and surrounding regions, and that the links between ID, child and maternal mortality as well as mental retardation are known, the Ethiopian government has been reluctant to take preventive measures and iodize salt as a prophylactic measure. From the perspective of the Oromo people, there are no any other projects that are more important than their children and maternal health. Denying the Oromo people the right to decide on their affairs and allowing easily preventable nutrition deficiencies to remain a widespread problem in Oromia truly reveals the Ethiopian government’s colonial policies.
Third is the violation of economic rights. For over a century the Ethiopian government’s economic policies have been designed to exploit the human and natural resources of Oromia. Such policies dispossessed the Oromo people of their land and this conditioned them to live in poverty. Increased poverty levels make iodine rich foods inaccessible for the poor. In many iodine deficient communities, impoverished people can’t afford to eat fish, meat and drink milk, which are rich in iodine and they become dependent on foods known to be goitrogenics2 and this further worsens the problem. Violation of economic rights has also conditioned the Oromo people to live in poverty. Poverty further aggravates ID levels.
Fourth is the violation of cultural rights. Culture constitutes the worldview of people and it is used to maintain peace, stability and maintain social order and defend the interests of the group. Like many other colonizers, racial and cultural superiority theories and economic interests drive Ethiopian colonial policies. The Ethiopian cultural superiority theory is ingrained in their social policies, which deliberately attacked the Oromo culture that promotes caring for the natural environment. Indeed, the Ethiopian elites have made greet efforts to dismantle the Oromo culture and worldview and several European empire builders provided them with human and material resources and political support. The Oromo culture and worldview that promote caring for the environmental world are seen as paganism by the Ethiopian government and European missionaries. The Ethiopians have convinced themselves that it is their moral duty to force and persuade the Oromo people to dismantle the natural world. This has contributed to the deforestation and erosion of Oromia. Violating the cultural rights of the Oromo people, through their formal and informal education, the Ethiopian government has made continuous efforts to convince the Oromo people that the colonial power relations that are responsible for their suffering are natural, inevitable and even desirable [81].
The violation of cultural rights and the imposition of the worldview of colonizers distort the reality of colonized peoples. Dominant groups very often mis-concepttualize and misunderstand the needs of the marginalized. This is usually done on purpose. For example, in the nineteenth century American medical doctors called, iron deficiency disease Cachexia Africana because the disease affected many African Americans who lived in slavery [82]. The sufferers of iron deficiency were known as dirt eaters. The white doctors understood the nutritional deficiency that affected black families to be a kind of mental inferiority rather than unjust social conditions that exposed those families to iron deficiency. In the same way, the Ethiopian government explains the protein-energy and several micronutrient deficiencies that many Oromos face as if these were natural tragedies rather than being the result of the social conditions that the colonial power relation has created.
Fifth is the violation of environmental rights. Population health is dependent on the physical environment and any damage to the environment has deleterious health effects. The concept of environmental rights entails the right to live in a healthy natural environment, with access to clean water, air and food. Violation of environmental rights allowed for the deforestation of Oromia, the pollution of rivers, lakes and made soil erosion a natural and acceptable phenomenon. In their turn, soil erosion, deforestation and pollution of rivers and lakes further aggravate the ID levels.
Conclusions
In this paper, I have made an effort to capture and analyse the complex causes of ID and the social and health problems that affect women. From this paper, the following conclusions can be made. First, iodine is a trace element that is needed for the production of thyroid hormone. Adequate intake of it allows cells, tissues and organs of the body to develop, differentiate and support life and to prevent many chronic and acute diseases and social problems. Our present knowledge clearly suggests that children born in iodine deficient areas are at risk of experiencing several neurological disorders, mental retardation cretinism, deaf-mutism, squinting and physical disabilities [83]. In addition, women who live in iodine deficient areas experience reproductive failure such as stillbirths and miscarriages.
Second, goiter is more common among young girls and women than young boys and men. In animal clinical studies, it has been shown that female fetuses are more sensitive in their cognitive development to ID. If this also true for human beings this might contribute to differences in educational achievements between men and women. For those who are intend to bring about improvement in women’s health, reduce health disparity and build their capacity, prevention of ID should play a central role. For those who wish to make practical efforts to promote gender equity and bring sustainable development, tackling the root causes of ID in Oromia and preventing IDDs should be part of the plan.
Third, if dietary iodine is indeed a key to human cognitive capacity, it has major consequences to community’s social, economic, political and cultural development. If ID causes social withdrawal, hinders participation of people leading to social isolation, prevention is critical in building the capacity of people. Providing food aid when famine occurs is like treating the symptoms of the illness rather than the disease it-self. It is worthwhile promoting the prevention of ID as a means of building the capacity of community.
Fourth, ID is an easily preventable public health problem and iodizing salt is a cost effective prophylactic measure. Building decent public health conditions goes beyond individuals’ efforts. In many parts of the world where people are under colonial rule, public health conditions deteriorate or show slow improvement. It has been clearly shown that to build the public good, the people need to be empowered, get organized and allocate their human and material resources as they please. It has been shown that food security can be established if the society has developed its social protections. Hence, in Oromia, the lack of iodized salt is a manifestation of the violation of collective rights (social, economic, cultural, political and environmental) of the Oromo people.
Fifth, the struggle for social justice, collective and individual rights should be seen as the struggle for quality of life. If the Oromo people were entitled to decide on their affairs they would have done everything possible to prevent ID and could have averted the social, cultural, economic and health problems that followed.
Sixth, despite our knowledge about the public health impact of ID, the Ethiopian government is reluctant to iodize salt. Human rights are indivisible, interdependent and interrelated. As Sen [52] clearly explained, freedom of one kind leads to the enjoyment of other freedoms; to put it another way, violations of one form of rights lead to the violation of the other forms. For example, violating economic rights led to violating social rights. Barring access to basic necessities in life, denies the Oromo people the right to participate in the decision-making process. ID should be seen as a part of a vicious cycle of cumulative violations of the collective rights of the Oromo people and preventing this public health problem should be seen as a means of building the capacity of people, improving their health and helping people to choose in life.
REFERENCES
- Dugassa, B. and Negassa, A. (2012) Understanding the ecology of iodine deficiency and its public health implications: The case of oromia region in Ethiopia. Journal of Community Nutrition & Health, 1, 4-17.
- UNICEF (2008) Sustainable elimination of iodine deficiency, progress since the 1990. World Summit for Children. http://www.childinfo.org/files/idd_sustainable_elimination.pdf
- Iodine Network (2012) Country profiles Ethiopia. http://iodinenetwork.net/countries/Ethiopia.htm#6
- WHO (2007) Iodine deficiency in Europe: A continuing public health problem. In: Anderson, M., De Benoist, B., Darnton-Hill, I. and Delange, F., Eds., France. http://whqlibdoc.who.int/publications/2007/9789241593960_eng.pdf
- WHO (2010) Ethiopia: Health profile. http://www.who.int/gho/countries/eth.pdf
- WHO (2010) Kenya: Health profile. http://www.who.int/gho/countries/ken.pdf
- Stewart, G., Carter, J., Parker, A. and Alloway, B. (2003) The illusion of environmental iodine deficiency. Environmental Geochemistry and Health, 25, 165-170. doi:10.1023/A:1021281822514
- Meletis, C. and Zabriskie, N. (2007) Iodine, a critically overlooked nutrient. Alternative & Complementary Therapies, 13, 132-136. doi:10.1089/act.2007.13309
- Hetzel, B. and Mano, A. (1989) A review of experimental studies of iodine deficiency during fetal development. Journal of Nutrition, 119, 145-151.
- Ingenbleek, Y. and Jung, L.B. (1999) A new iodized oil for eradicating endemic goiter. In: Abdulla, M., Bost, M., Gamon, S., Arnaud, P. and Chazot, G., Eds., New Aspects of Trace Element Research, Smith-Gordon, London.
- Holcomb, B. and Ibssa, S. (1990) The invention of Ethiopia. Red Sea Press, Trenton.
- Jalata, A. (2005) Oromia & Ethiopia: State formation and ethnonational conflict, 1868-2004. Lawrenceville, The Red Sea Press, Trenton.
- Bulcha, M. (2002) The making of the Oromo diaspora: A historical sociology of forced migration. Minneapolis, Kirk House Publishers, Minn.
- Dei, G. (2006) Anti-Colonialism and Education. The Politic of Resistance, Sense Publishers, Rotterdam.
- Dugassa, B. (2008) Colonial trauma, community resiliency and community health development: The case of the Oromo people in Ethiopia. Journal of Health & Development, 4, 43-61.
- Hameso, S. and Hassen, M. (2008) Arrested development in Ethiopia: Essays on underdevelopment, democracy and self-determination. The Red Sea Press, Trenton.
- Clay, J. and Holcomb, B. (1986) Politics and the Ethiopian famine, 1984-1985. Cultural Survival, Cambridge.
- Dugassa, B. (2004) Human rights violations and famine in Ethiopia. Journal of Oromo Studies, 11, 47-68.
- Dugassa, B. (2006) Ethiopian language policy and health promotion in Oromia. Journal of Sociology & Social Welfare, 33, 69-86.
- Dunn, J. Pretell, E., Daza, H.C. and Viteri, E.F. (1986) Towards the eradication of endemic goiter, cretinism, and iodine deficiency. Pan American Health Organization, Pan American Sanitary Bureau, Regional Office of the World Health Organization, Washington DC.
- Semba, R. and Francois, D. (2008) Nutrition and health in developing countries. 2nd Edition, Humana Press, Totowa.
- Encyclopedia of Public Health (2006) Lester, B. and Gale, C., Eds. http://www.enotes.com/public-health-encyclopedia/iodine
- Andersson, M., Takkouche, B., Egli, I. and De Benoist, B. (2003) The WHO global database on iodine deficiency disorders: The importance of monitoring iodine nutrition. Scandinavian Journal of Nutrition, 47, 162-166. doi:10.1080/11026480310022334
- Chan, S., Andrew, M., Lingas, R., McCabe, C., Franklyn, J., Kilby, M. and Matthews, S. (2005) Maternal nutrient deprivation induces sex-specific changes in thyroid hormone receptor and deiodinase expression in the fetal guinea pig brain. The Journal of Physiology, 566, 467- 480. doi:10.1113/jphysiol.2005.084673
- Field, E. and Robles, O. (2006) Iodine deficiency and schooling attainment in Tanzania. http://www.princeton.edu/rpds/seminars/pdfs/Field_IDD_Tanzania.pdf
- Friedhoff, A.J., Miller, J.C., Armour, M., Schweitzer, J.W. and Mohan, S. (2000) Role of maternal biochemistry in fetal brain development: effect of maternal thyroidectomy on behaviour and biogenic amine metabolism in rat progeny. The International Journal of Neuropsychopharmacology, 3, 89-97. doi:10.1017/S1461145700001863
- FAO (2011) Iodine. http://www.fao.org/DOCREP/004/Y2809E/y2809e0i.htm
- WHO (2008) Closing the gap in a generation: Health equity through action on the social determinants of health. http://whqlibdoc.who.int/publications/2008/9789241563703_eng.pdf
- Ontario, C.H. (2011) Community capacity building. http://www.ohcc-ccso.ca/en/community-capacity-building-0
- Gostin, L. and Powers, M. (2006) What does social justice require for the public’s health? Public health ethics and policy imperatives. Health Affairs, 25, 1053-1060. doi:10.1377/hlthaff.25.4.1053
- Kosny, A. (1999) The social determinants of health: Equity across the lifespan. Prepared for made to measure: Designing research, policy and action approaches to eliminate gender inequity. National Symposium, Halifax, 3-6 October.
- Kelly, M., Bonnefoy, J., Morgan, A., Butt, J. and Bergman, V. (2007) The social determinants of health: Developing an evidence base for political action, final report to World Health Organization Commission on the social determinants of health. Universdad del Desarrollo, Chille and National Institute for Health and Clinical Excellence, United Kingdom.
- Esterberg, K. (2002) Qualitative methods in social research. McGraw Hill, Boston.
- WHO (1948) Constitution of the World Health Organization. http://www.who.int/governance/eb/who_constitution_en.pdf
- Smith, L. (2002) Decolonizing methodologies. Research and Indegenous People, Zed Books, London.
- CDC (2008) Data collection methods for program evaluation: Observation. http://www.cdc.gov/healthyYouth/evaluation/pdf/brief16.pdf
- Dugassa, B. (2010) Research directions. The OSA Newsletter, 1, 6. http://www.oromostudies.org/OSA%20NEWSLETER%202010-1.pdf
- De Escobar, G., Obregon, M.J. and Del Rey, F.E. (2004) Role of thyroid hormone during early brain development. European Journal of Endocrinology, 151, U25-U37. doi:10.1530/eje.0.151U025
- Zimmermann, M. (2009) Iodine deficiency. Review, 30, 376-408.
- Semba, R.D., de Pee, S., Hess, S.Y., Sun, K., Sari, M. and Bloem, M.W. (2008) Child malnutrition and mortality among families not utilizing adequately iodized salt in Indonesia. The American Journal of Clinical Nutrition, 87, 438-444.
- Hegedus, L., Karstrup, S. and Rasmussen, N. (1986) Evidence of cyclic alterations of thyroid size during the menstrual cycle in healthy women. American Journal of Obstetrics & Gynecology, 155, 142-145.
- Kristof, N.D. and WuDunn, S. (2009) The women’s crusade. New York Times Magazine. http://www.nytimes.com/2009/08/23/magazine/23Women-t.html?pagewanted=all&_r=0
- Bjorvatn, K., Reimann, C., Ostvold, S.H., Tekle-Haimanot, R., Melaku, Z. and Siewers, U. (2003) High-fluoride drinking water. A health problem in the Ethiopian rift valley 1. Assessment of lateritic soils as defluoridating agents. Oral Health & Preventive Dentistry, 1, 141-148.
- Dugassa, F.B. (2009) Public health impacts of high fluoride in water and soil—The case of rift valley region of Oromia in Ethiopia. The 23rd Annual Conference of Oromo Studies Association, Atlanta, 1-2 August 2009.
- Marine, D. and Kimball, O.P. (1920) Prevention of simple goiter in man. Archives of Internal Medicine, 25, 661-672. doi:10.1001/archinte.1920.00090350088005
- Bürgi, H., Supersaxo, Z. and Selz, B. (1990) Iodine deficiency diseases in Switzerland one hundred years after Theodor Kocher’s survey: A historical review with some new goitre prevalence data. Acta Endocrinologica, 123, 577-590.
- Stanbury, J. and Hetzel, B. (1980) Endemic goiter and endemic cretinism. Iodine nutrition in health and disease. A Willey Medical Publication, New York.
- Maberly, G. (1994) Iodine deficiency disorders: Contemporary scientific issues. The Journal of Nutrition, 124, S1473-S1478.
- Hetzel, B.S. and Pandav, C.S. (1996). S.O.S. for a billion. The conquest of iodine deficiency disorders. 2nd Edition, Oxford University Press, Dehli.
- Delange, F. (2000) Iodine deficiency in the thyroid. In: Braverman, L.E. and Utiger, R.D., Eds., A Fundamental and Clinical Text, Lippincott Publishing, Philadelphia, 295-316.
- Taylor, R. and Rieger, A. (1985) Medicine as social science: Rudolf Virchow on the typhus epidemic in upper Silesia. International Journal of Health Services, 15, 547-559. doi:10.2190/XX9V-ACD4-KUXD-C0E5
- Sen, A. (1999) Development as freedom. Random House Digital, New York.
- Narayan, D., Patel, R., Schafft, K., Rademacher, A. and Koch-Schulte, S. (2000) Voice of the poor. Can anyone hear us? Oxford University Press for the World Bank, Oxford.
- UNICEF (2005) ETHIOPIA: Majority lack access to clean water-UNICEF. http://www.irinnews.org/report.aspx?reportid=53553
- Cherinet, A. and Kelbesa, U. (2000) Determinants of iodine deficiency in school children in different regions of Ethiopia. East African Medical Journal, 77, 133-137.
- Eduardo, J., Carlos, D.H. and Fernando, V.E. (1986) Towards the eradication of endemic goiter, cretinism, and iodine deficiency. Pan American, Health Organization, Pan American Sanitary, Bureau, Regional Office of the World Health Organization, Washington DC.
- WHO (2006) WHO global database on iodine deficiency. http://who.int/vmnis/iodine/data/database/countries/eth_idd.pdf
- Berlin, I.B. (1969) Four essays on liberty. Oxford University Press, London and New York.
- Levin, H.M., Pollitt, E., Galloway, R. and McGuire, J. (1993) Micronutrient deficiency disorders. In: Jamison, D.T., Mosley, W.H., Measham, A.R., Bobadilla, J.L., Eds., Disease Control Priorities in Developing Countries, World Bank, Washington DC.
- [61] WHO (2012) Health & human rights. http ://www.who.int/hhr/teamflyer_eng_rev.pdf
- [62] Human Rights Watch (2010) Development without freedom: How aid underwrites repression in Ethiopia, New York.
- [63] BBC (2011) Ethiopia “using aid as weapon of oppression”. http://news.bbc.co.uk/2/hi/programmes/newsnight/9556288.stm
- [64] Dugassa, B. (2012) Denial of leadership development and the underdevelopment of public health: The experience of the Oromo people in Ethiopia. Journal of Oromo Studies, 19, 139-174.
- [65] Hetzel, B.S. and Maberly, G.F. (1986) Iodine. Trace Elements in Human and Animal Nutrition, 5th Edition, Academic Press, New York, 139-208. doi:10.1016/B978-0-08-092469-4.50006-6
- [66] McDowell, L.R. (1992) Iodine. Minerals in Animal and Human Nutrition, Academic Press, New York, 224-245.
- [67] WHO (1996) Trace elements in human nutrition and health. Geneva. http://www.who.int/nutrition/publications/micronutrients/9241561734/en/index.html
- [68] Hunt, J.M. (2005) The potential impact of reducing global malnutrition on poverty reduction and economic development. Asia Pacific Journal of Clinical Nutrition, 14, S10-S38.
- [69] Hetzel, B.S., Delange, F., Dunn, J.T., Ling, J., Mannar, V. and Pandav, C. (2004) Towards the global elimination of brain damage due to iodine deficiency. Oxford University Press, Delhi.
- [70] Behrman, J.R. and Rozenweig, M.R. (2001) The returns to increasing body weight. PIER Working Paper, University of Pennsylvania, Philadelphia.
- [71] Darnton-Hill, I., Webb, P., Harvey, P., Hunt, J., Dalmiya, N., Chopra, M.M., Bloem, M. and De Benoist, B. (2005) Micronutrient deficiencies and gender: Social and economic costs. The American Journal of Clinical Nutrition, 81, S1198-S1205.
- [72] Allen, L., De Benoist, B., Dary, O. and Hurrell, R. (2004) Guidelines on food fortification with micronutrients for the control of micronutrient malnutrition. WHO, Geneva.
- [73] Mason, J.B., Musgrove, P. and Habicht, J.P. (2003) At least one-third of poor countries’ disease burden is due to malnutrition. DCPP Working Paper, Disease Control Priorities Project, Fogarty International Center, NIH, Bethesda, 1-19.
- [74] Abuye, C. and Berhane, Y. (2007) The goitre rate, its association with reproductive failure, and the knowledge of iodine deficiency disorders (IDD) among women in Ethiopia: Cross-section community based study. BMC Public Health, 7, 316. doi:10.1186/1471-2458-7-316
- [75] WHO (2011) Making pregnancy safer and reproductive health. http://www.searo.who.int/en/Section13/Section36/Section2439.htm
- [76] Ministry of Health, Family Health Department (2004) National guideline for control and prevention of micronutrient deficiencies Ethiopia. http://www.aedlinkagesethiopia.org/My_Homepage_Files/Download/Micronutrients%20guideline.pdf
- [77] WHO (2001) Assessment of iodine deficiency disorders and monitoring their elimination a guide for program managers.
- [78] Delange, F. (2011) Iodine deficiency as a cause of brain damage. Postgraduate Medical Journal, 77, 217-222.
- [79] Cobra, C.M., Rusmil, K., Rustama, D., Djatnika, S., Suwardi, S., Permaesih, D., Muherdiyantiningsih, M.S. and Semba, R. (1997) Infant survival is improved by oral Iodine supplementation. Journal of Nutrition, 127, 574-578.
- [80] Dunn, J. and Delange, F. (2001) Commentary: Damaged reproduction: The most important consequence of iodine deficiency. The Journal of Clinical Endocrinology & Metabolism, 86, 2360-2363. doi:10.1210/jc.86.6.2360
- [81] USAID (2006) Ethiopia pilot study of teacher professional development. Quality in education, teaching, and learning: Perceptions and practice, produced by American institutes for research under the EQUIP1 LWA. Academy for Educational Development, Institute of Educational Research Addis Ababa University. http://pdf.usaid.gov/pdf_docs/PNADH771.pdf
- [82] Dugassa, B. (2011) Colonialism of mind: The experience of Oromo people in Ethiopia. Journal of Sociology of Mind, 1, 55-64. doi:10.4236/sm.2011.12007
- [83] Byrd, M. and Clarton, L. (2000) An American health dilemma: A medical history of African Americans and the problem of race beginning to 1900. Routledge, New York.
- [84] Editorial (2001) Iodine deficiency as a cause of brain damage. Postgraduate Medical Journal, 77, 217-220. doi:10.1136/pmj.77.906.217
NOTES
1Fortification is the practice of deliberately increasing the content of essential micronutrients such as vitamins and minerals including trace elements in a food, so as to improve the nutritional quality of the food supply and provide a public health benefit with minimal risk to health.
2Goitrogenic foods are foods naturally containing substances that can interfere with the metabolism of iodine or functions of the thyroid gland. Foods known to be goitrogenic are cruciferous vegetables which includes: broccoli, brussel sprouts, cabbage, cauliflower, kale, kohlrabi, mustard, rutabaga, turnips, millet, peaches, peanuts, radishes, soybean and soy products, including tofu, spinach and strawberries.

