Open Journal of Medical Psychology
Vol.2 No.1(2013), Article ID:27232,5 pages DOI:10.4236/ojmp.2013.21002
Personality Characteristics among Patients Waiting for Liver or Kidney Transplants*
1Université Paris Descartes, Sorbonne Paris Cité, IUPDP, Paris, France
2Hôpital Bicêtre, Département de Psychiatrie, INSERM, Université Paris XI, Le Kremlin Bicêtre, France
Email: isabelle.varescon@parisdescartes.fr
Received October 14, 2012; revised November 17, 2012; accepted November 30, 2012
Keywords: Personality Disorder; Transplantation; Kidney; Liver
ABSTRACT
Introduction: Personality characteristics are believed to predict post-transplant adherence and outcome. However, data concerning the prevalence and type of personality disorders (PDs) among transplant populations are sparse. Objectives: To evaluate the prevalence and types of PDs among patients waiting for liver or kidney transplants, to compare the results obtained between the two groups and to identify predictors of the prevalence of PDs. Method: In a prospective cohort study, 629 patients waiting for liver (n = 196) or kidney (n = 433) transplants were assessed by the Personality Diagnostic Questionnaire, fourth edition (PDQ-4+). Results: The 629 pre-transplant patients were 46.1 years old on average (SD: 11.5). The PDQ total score was 25.5 (SD: 13.7). 36.5% had a total score equal to or greater than 30. Paranoid (42.1%), avoidant (31.1%) and obsessive-compulsive (29.8%) were the most common possible PDs identified. Patients waiting for a kidney transplant had a higher total score than those waiting for a liver transplant (p < 0.001) and they also had significantly more paranoid (p = 0.001), obsessive-compulsive (p = 0.002) and avoidant (p = 0.001) PDs. Comment: In case of possible PDs, an assessment of other clinical variables for helping patients is needed so that a specific treatment could be offered to patients at the time of their inclusion on the waiting list, during the waiting period and after the organ transplant.
1. Introduction
The psychiatric assessment of patients waiting for an organ transplant is common and should have several objectives: diagnosis and treatment of current psychiatric disorders, assessment of psychological context and the search for predictive factors of poor compliance [1-3]. The presence of personality disorders (PDs) has been shown to affect adherence among psychiatric and general medical patients [4]. For this reason, some PDs have sometimes been considered as a contraindication for a transplant in the majority of transplantation programs [5]. Clinically, personality characteristics are also believed to predict post-transplant adherence and outcome. However, data concerning the prevalence and type of PDs among transplant populations are sparse [4]. The growing population of patients who need liver or kidney transplantation has intensified the need to identify PDs for less favorable adjustment to the pre-transplantation evaluation process and long term outcome [3]. However, to our knowledge, no studies have specifically examined PDs in a large sample of patients waiting for a liver or kidney transplant.
The objectives of the present study were thus: 1) to evaluate the prevalence and types of PDs among a sample of such patients; 2) to compare the prevalence and types of PDs among patients waiting for liver or kidney transplants; 3) to identify predictors of the prevalence of PDs.
2. Method
2.1. Population and Procedure
PSYGREF is a prospective cohort of adult patients assessed while waiting for kidney and liver transplantation in three centers in the southern area of Paris. The cohort has been described elsewhere [2,3,6]. The patients were recruited between September 2002 and June 2008. Eligible participants were at least 18-year old and had sufficient proficiency in French to complete the assessments. Participation was proposed to 704 patients meeting these criteria and 629 of them agreed to take part in this study. 196 patients were waiting for a liver transplant and 433 patients were waiting for a kidney transplant.
Each patient provided their written informed consent. Those unable to communicate or complete questionnaires or who were referred for an emergency transplantation were excluded. PSYGREF baseline assessments were conducted at each transplantation center by a trained clinical psychologist, blind to medical data. On account of ethical considerations and in order to avoid bias arising from additional visits, assessments were carried out when patients had an appointment at the transplantation center for their usual medical visits. The PSYGREF procedures were approved by the ethics committee of the University Hospital of Bicêtre and the institutional review board of the Clinical Research Department of Paris. Data were used according to the standard regulations of the French Network for Transplantation and for the preservation of patient anonymity and privacy Measures.
The Personality Diagnostic Questionnaire, fourth edition (PDQ-4+) is a 99-item, true/false self-report questionnaire designed to assess the ten PDs of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders. True is always the pathological response. The PDQ-4+ includes the additional diagnoses of passive-aggressive personality disorder and depressive personality disorder which are included in the appendix of DSM-IV [7]. Each PD criterion is assessed by 1 item. Exceptions are borderline PD, for which 2 or more examples must be given to reach the threshold for the impulsivity criterion, and antisocial PD, where 3 items are required for the conduct disorder in the childhood criterion. Also included are six items composing two validity scales: a “Too Good” scale consisting of four items may indicate underreporting of pathology and a “Suspect Questionnaire” consisting of two items designed to identify lying, responding randomly or not taking the questionnaire seriously.
The total PDQ-4+ score is determined by summing all the pathological responses. A total score of 30 or more indicates a substantial likelihood that the patient has a significant personality disturbance [8,9].
Several international studies have been conducted with the PDQ-4+ in clinical and non-clinical samples for assessing probable PDs. An examination of the screening properties of the PDQ-4+ showed that the questionnaire generated many false-positive diagnoses but few falsenegative ones [10], thus it appears to be suitable for use as a screening tool. The French version of the PDQ-4+, which has been employed in several published works [10,11], was used for the present study [12,13].
2.2. Statistical Analyses
Analyses were conducted using the software SPSS™ (V17, IBM). First, the distribution and frequencies of sociodemographic data among patients waiting for kidney or liver transplants were examined. T-tests and Chi² were used to evaluate differences between the two groups in terms of sociodemographic data and PDQ-4+ scores. Finally, to investigate to what degree sociodemographics predict PDs, a regression analysis was carried out.
3. Results
3.1. Sociodemographic Characteristics
The 629 patients were 46.1 years old on average (SD: 11.5, range 19 to 78). 68.8% were waiting for a kidney transplant and 31.2% for a liver transplant. No differences were found in the sociodemographic data between the kidney transplantation sample and the liver transplantation sample except for age (p = 0.0012) and sex (p = 0.006) (Table 1).
3.2. Results Obtained from PDQ-4+
Cronbach’s α varied from 42 to 64. Five of the 12 scales had a reliability coefficient greater than 0.60: avoidant (0.67), dependent (0.64), schizotypal (0.63), narcissistic (0.62), depressive (0.61). The other personality disorders were ranged as follows: borderline (0.58), paranoid (0.57), histrionic (0.54), obsessive-compulsive (0.54), negativism (0.54), antisocial (0.46) and schizoid (0.42). Results associated with these last scales must be interpreted with precaution due to the potential impact of measurement errors which are substantial here.
The total score was 25.5 (SD: 13.7, range 0 - 74). 36.5% had a PDQ total score equal to or greater than 30. Paranoid (42.1%), avoidant (31.1%) and obsessivecompulsive (29.8%) were the most common PDs identified. Patients waiting for a kidney transplant had a higher total score (mean = 27) than those waiting for a liver transplant (mean = 22.1, t(627) = 4.2, p < 0.001). Patients waiting for a kidney transplant also had a higher number of possible PDs (mean = 2.64) than those waiting for a liver transplant (mean = 1.9, t(627) = 3.6, p < 0.001). The significant differences for patients waiting for a kidney transplant were found for paranoid (p = 0.001), obsessive-compulsive (p = 0.002) and avoidant (p = 0.001) PDs (Table 2). After controlling the interactions between gender and type of transplant for each personality disoder, general regression model analyses indicated that these results do not depend on gender prevalence.
Regression analyses were also conducted with the total PD scores as dependent variables: (1) the sociodemographic data (age, sex, marital status, parental status, occupational status, educational level); (2) the type of transplantation as independent variables. The whole model explained 9% of the PDs (F(8.617) = 7.6, p < 0.0001). When the sociodemographic variables were controlled, the type of organ transplant still had an effect
Table 1. Sociodemographic characteristics.
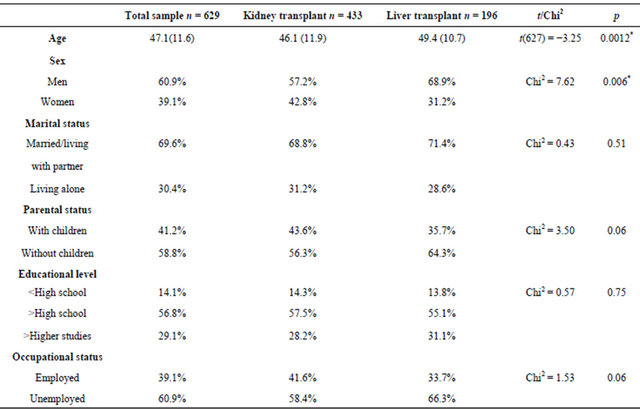
*Significant p.
Table 2. Prevalence of PDs according to PDQ-4+.

*Significant p.
on the presence of personality disorders (β = 0.19, F(1.617) = 19.2, p < 0.001). The results also indicated that the lower the level of education (β = −0.15, F(1.617 = 13.7, p < 0.001) the higher the presence of a PD.
4. Discussion
The prevalence of PDs in community populations has been reported as 10% to 13.5% in previous published studies [14-16]. In our study, 36.5% had a PDQ total score equal to or greater than 30. Paranoid, avoidant and obsessive-compulsive were the most common possible PDs identified. Paranoid PD is characterized by a pervasive long-standing suspiciousness and generalized mistrust of others. Avoidant PD is characterized by a pervasive pattern of social inhibition, feelings of inadequacy, extreme sensitivity to negative evaluation and avoidance of social interaction. Obsessive-compulsive PD is characterized by a pervasive pattern of preoccupation with orderliness, control and perfectionism.
Concerning the literature about organ transplant patients in particular, Yates, LaBrecque & Pfab [5] found that 27% of 73 subjects with an alcoholic-related liver disease met the criteria for PDs (PDQ-R), especially antisocial PD. Among 73 adult cardiothoracic transplant recipients, Stilley, Dew, Pilkonis et al. [4] assessed PDs. The results showed that 33% met the diagnostic criteria of PDs with obsessive-compulsive being the most prevalent. Our result is consistent with previous research which has shown that the traits of an obsessive-compulsive personality, such as rigidity, inflexibility and perfectionism, are associated with an increased risk of developing chronic disease [4]. Indeed, the patients included in our study all suffered from chronic liver or kidney disease requiring organ transplantation.
In the same cluster (cluster C), we found a significant level of possible avoidant PD where anxiety and inhibition predominate. Concerning the high levels of possible paranoid PD, it is possible that a medical population responds to questions about mistrust in a certain way because of their experiences as patients.
PDs as a possible contraindication to transplant patients have been discussed in previous studies. In 1999, Weitzner, Lehninger, Sillivan & Fields [17] reported the case of a borderline patient and discussed the ethical issues involved in the evaluation of borderline patients and the determination of their appropriateness for a transplant. Akaho, Sasaki, Uoshino, Hagiya et al. [18] reported cases of bone marrow transplant patients who had been suffering from mental disorders. The transplantation was achieved in all the subjects with the exception of one with a borderline personality disorder. For liver transplantation, Yates, LaBrecque & Pfab [5] did not support the exclusion of subjects based solely on the diagnosis of a personality disorder because the latter is correlated with a variety of clinical variables which influence the process of transplantation.
Even though the results of our study should be interpreted with caution, due to the properties of the questionnaire, they show that more than a third of patients present possible PDs according to the PDQ-4+. The question of an assessment of possible PDs should be systematic when patients are added to the waiting list for an organ transplant. The PDQ-4+ could thus be used as a screening tool. In order to avoid false-positive diagnoses, as mentioned in the Method section above, a clinical assessment by a psychiatrist or a psychologist could prove useful. In case of possible PDs, an assessment of other clinical variables for helping patients is needed so that a specific treatment could be offered to patients at the time of their inclusion on the waiting list and during the period before the organ transplant. Clearly, patients with PDs require more time and attention from the medicalpsycho-social team to help them adjust to the pretransplantation evaluation process, to facilitate relationships between them and the staff and afterwards to cope with the graft. A multidisciplinary team is highly beneficial because patients with PDs need more innovative interventions to promote adherence and maximize outcomes [4].
The present study has some potential limitations; PD was defined according to a limited interview and selfreport data with subscales including some limits in term of internal reliabilities. A complete interview with another scale was not carried out because of time constraints and sometimes the high level of medical illness in the study sample. The results obtained for pretransplant patients do not reveal the impact of these results on post-transplantation morbidity, mortality or adherence. Nevertheless, these findings obtained in a larger sample do contribute to a better understanding of the possible PDs in adult patients assessed while waiting for kidney and liver transplantation in three centers. Few studies of PD assessment have been published for patients waiting for organ transplants. Among these data, most are related to a small number of people in a single center. To our knowledge, this research is the first to assess PDs among a large sample of patients waiting for liver or kidney transplants in three organ transplant centers.
REFERENCES
- E. Corruble, “L’Evaluation Psychiatrique du Futur Greffé: Psychiatric Assessment of Patients Waiting for a Transplantation,” Annales Médico-Psychologiques, Vol. 168, No. 3, 2010, pp. 216-219. doi:10.1016/j.amp.2010.01.001
- E. Corruble, C. Barry, I. Varescon, A. Durbach, D. Samuel, P. Lang, D. Castaing, B. Charpentier and B. Falissard, “Report of Depressive Symptoms on Waiting List and Mortality after Liver and Kidney Transplantation: A Prospective Cohort Study,” BMC Psychiatry, Vol. 11, No. 182, 2011, pp. 182-192. doi:10.1186/1471-244X-11-182
- E. Corruble, C. Barry, I. Varescon, B. Falissard, D. Castaing and D. Samuel, “Depressive Symptoms Predict LongTerm Mortality after Liver Transplantation,” Psychosomatic Research, Vol. 71, No. 1, 2011, pp. 32-37. doi:10.1016/j.jpsychores.2010.12.008
- C. S. Stilley, M. A. Dew, P. Pilkonis, A. Bender, M. McNulty, A. Christensen, K. R. McCurry and R. L. Kormos, “Personality Characteristics among Cardiothoracic Transplant Recipients,” General Hospital Psychiatry, Vol. 27, No. 2, 2002, pp. 113-118. doi:10.1016/j.genhosppsych.2004.11.005
- W. R. Yates, D. R. LaBrecque and D. Pfab, “Personality Disorder as a Contraindication for Liver Transplantation in Alcoholic Cirrhosis,” Psychosomatics, Vol. 39, No. 6, 1998, pp. 501-511. doi:10.1016/S0033-3182(98)71282-4
- E. Corruble, C. Barry, I. Varescon, B. Falissard, D. Castaing and D. Samuel, “The Transplanted Organ Questionnaire: A Validation Study,” Journal of Psychosomatic Research, Vol. 73, No. 4, 2012, pp. 319-324. doi:10.1016/j.jpsychores.2012.07.012
- American Psychiatric Association, “Diagnostic and Statistical Manual of Mental Disorders,” American Psychiatric Association, Washington DC, 1994.
- S. E. Hyler, A. E. Skodol, J. M. Oldham, H. D. Kelleman and N. Doudge, “Validity of the Personality Diagnostic Questionnaire-Revised: A Replication in an Outpatient Sample,” Comprehensive Psychiatry, Vol. 33, No. 4, 1992, pp.73-77. doi:10.1016/0010-440X(92)90001-7
- S. E. Hyler, “Personality Diagnostic Questionnaire (PDQ- 4+),” State Psychiatric Institute, New York, 1994.
- M. Bouvard, M. Vuachet and C. Marchand, “Examination of the Screening Properties of the Personality Questionnaire-4+(PDQ-4+) in a Non-Clinical Sample,” Clinical Neuropsychiatry, Vol. 8, No. 2, 2011, pp. 151-158.
- H. Chabrol, S. Callahan and S. E. Hyler, “Frequency and Structure of DSM-IV Personality Disorder Traits in College Students,” Personality and Individual Differences, Vol. 43, No. 7, 2007, pp. 1767-1776. doi:10.1016/j.paid.2007.05.015
- M. Bouvard and P. Cosma, “Étude Exploratoire d’un Questionnaire sur les Troubles de la Personnalité,” L’Encé- phale, Vol. 34, No. 5, 2007, pp. 517-525. doi:10.1016/j.encep.2007.08.006
- M. Bouvard, “Questionnaires et Echelles d’ Evaluation de la PersonnalitE: Personality Scales and Questionnaires,” Masson, Paris, 2002.
- J. Reich, W. Yates and M. Nduaguba, “Prevalence of DSM-III Personality Disorders in the Community,” Social Psychiatry and Psychiatric Epidemiology, Vol. 24, No. 1, 1989, pp. 12-16. doi:10.1007/BF01788194
- M. F. Lenzenweger, A. W. Loranger, L. Korfine and C. Neff, “Detecting Personality Disorders in a Non-Clinical Population,” Archives of General Psychiatry, Vol. 54, No. 4, 1997, pp. 345-351. doi:10.1001/archpsyc.1997.01830160073010
- S. Torgersen, E. Kringlen and V. Cramer, “The Prevalence of Personality Disorders in a Community Sample,” Archives of General Psychiatry, Vol. 58, No. 6, 2001, pp. 590-596. doi:10.1001/archpsyc.58.6.590
- M. A. Weitzner, F. Lehninger, D. Sullivan and K. K. Fields, “Borderline Personality Disorder and Bone Marrow Transplantation: Ethical Considerations and Review,” Psycho-Oncology, Vol. 8, No.1, 1999, pp. 46-54. doi:10.1002/(SICI)1099-1611(199901/02)8:1<46::AID-PON332>3.0.CO;2-1
- R. Akaho, T. Sasaki, M. Yoshino, K. Hagiya, H. Akiyama and H. Sakamaki, “Bone Marrow Transplantation in Subjects with Mental Disorders,” Psychiatry and Clinical Neuroscience, Vol. 57, No. 3, 2003, pp. 311-315. doi:10.1046/j.1440-1819.2003.01122.x
NOTES
*Funding/Support: This work was supported by grants from the Na- tional Hospital Clinical Research Program of the French Ministry of Health (PHRC AOM 01004) and the Clinical Research Department of the Paris Public Hospital System (FAP06011).

