International Journal of Clinical Medicine
Vol.5 No.12(2014), Article
ID:47029,6
pages
DOI:10.4236/ijcm.2014.512088
Inguinal Hernia Repair with Local Anesthesia in the Outpatient—10 Year Experience
Flavio Antonio de Sá Ribeiro1,2*, Baltazar de Araujo Fernandes3, João Pedro de Araujo Simões Corrêa3
1Surgery of UNIFESO, Teresopolis, Brazil
2Hospital Federal de Bonsucesso, Rio de Janeiro, Brazil
3General Surgery Service, Hospital Geral de Bonsucesso, Rio de Janeiro, Brazil
Email: *flavioasribeiro@bol.com.br
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 1 April 2014; revised 29 April 2014; accepted 25 May 2014
ABSTRACT
Objective: To demonstrate the feasibility of inguinal hernia repair with local anesthesia in an outpatient regime, with safety, efficacy and short learning curve. Methods: We prospectively evaluated 1186 patients undergoing inguinal hernia repair under local anesthesia on an outpatient basis between November 2004 and March 2014. Of the total number of hernias surgically treated in this period, 755 were operated on the right, 394 on the left and 37 bilateral. We used clinical, surgical and psychosocial criteria for inclusion in the procedure. The parameters for exclusion were complex, irreducible or recurrent hernia, obesity (BMI greater than 30 kg/m2), patient’s refusal and psychiatric disorder. All patients underwent elective surgery and were analyzed regarding surgical outcome, complications and hospital stay. Results: All operations were completed successfully. In no case there was need to change the anesthetic method. Surgical time was similar to that conducted with other methods of anesthesia and there were no cases of adverse effects of local anesthetics. Intra-operative complications amounted to approximately 2.64%. There was no need for hospital admissions greater than 24 hours. Conclusion: The procedure is feasible and causes no perioperative significant pain, is safe, can be performed by residents under supervision, has satisfactory patient acceptance and complications similar to those observed in a conventional herniorrhaphy, allowing lower time and cost of hospitalization and faster access to treatment.
Keywords:Inguinal Hernia/Surgery, Local Anesthesia, Ambulatory Surgical Procedures

1. Introduction
Inguinal hernia is a prevalent health issue in both developing and 1st world countries, mostly among men, accounting for important costs to society, if considering days away from work and recurrent medical visits. When left untreated, hernia may lead to serious consequences such as high morbidity and even mortality that could have been avoided. Inguinal hernia repair with local anesthesia is widely used around the world [1] [2] . In Brazil, even with the encouragement of its use for more than two decades [3] , it is not yet widespread and accepted, despite the benefits observed by several centers of excellence worldwide [4] [5] . Local anesthesia plus sedation applied for this type of surgery is a method with less impact on the function of organs and systems, is safe, effective, easy to perform, with lower incidence of side effects, such as cardiovascular instability, nausea, vomiting or urinary retention, allowing rapid mobilization and resulting in a shorter hospital stay [2] -[6] , generally less than 24 hours. The aim of this study is to prove the feasibility of inguinal hernia repair under local anesthesia without admission to hospital, its safety, efficacy and the short learning curve for the novice general surgery resident.
2. Methods
We analyzed medical records of 1186 patients undergoing inguinal hernia repair with local anesthesia on an outpatient basis between November 2004 and March 2014, all operated by the technique of Lichtenstein [7] [8] associated with intravenous sedation in The First Surgical Clinic of Bonsucesso General Hospital, in Rio de Janeiro. We used a subjective, unidimensional, numerical, eleven-point scale, as proposed by Huskisson in 1974 [9] , to evaluate the perioperative pain (0—no pain, 10—unbearable pain). In the first postoperative outpatient appointment, each patient attributed a value that best represented the intensity of perceived pain during surgery.
The surgical team consisted of two residents (First and second years) in the surgical field, and the staff surgeon supervising the procedure. Another resident, usually of the second year, was responsible for monitoring the patient. The procedure always took place at the main operating room unit, with a standby anesthesiologist present, not necessarily in the operating room, to give support when needed. The activities conducted by residents are defined in the General Surgery Residency Program, approved by the National Committee of Medical Residency [10] . The criteria for inclusion in the procedure were clinical: lack of uncontrolled comorbidities—up to ASA II and age younger than 70 years; surgical: primary, reducible inguinal hernia and Body Mass Index BMI less than 30 kg/m2; and psychosocial: understanding of the procedure and emotional stability. The exclusion criteria were complex, irreducible or recurrent hernia, obesity (BMI greater than 30 kg/m2) and psychiatric disorder. During the procedures the patients were monitored with pulse oximetry, cardiac monitoring and noninvasive blood pressure and had a peripheral venous access and 3 l/min oxygen mask therapy. We used an intravenous bolus of one to ten mg of midazolam, 20 mg of tenoxicam, 20 to 100 mg of meperidine and 1 g of cefazolin. After reaching the desired depth of sedation, we performed the blocking technique of the operative field with an anesthetic solution consisting of 20 ml of 0.75% ropivacaine, 20 ml of 2% lidocaine and 0.4 ml of 0, 1% adrenaline dissolved in 30 ml of distilled water, amounting a 70 ml solution.
3. Blocking Technique
The anesthetic block of the operative field was carried out according to the following steps: marking points on local anesthetic injection (Figure 1) to start the procedure with local anesthetic injection, 10 ml at the anterior superior iliac spine (Figure 1), 5 ml of the anesthesic solution, aiming for the deep ring and for the superficial femoral nerve (Figure 1); 5 ml in the incision; 5 ml at the level of the pubis and in external oblique aponeurosis (Figure 2), 5 ml directly over the external oblique aponeurosis, aiming for the cord, 5 ml of the anesthesic solution in the pubis (Figure 2) after opening the external oblique aponeurosis (Figure 3). One must wait for the latency time of 20 minutes before starting the procedure. The Learning Curve is evaluated as the time necessary for the first year resident to perform the complete surgical procedure, with domain of the anatomy and technique used and the anesthetic blockade. During this period the Surgical Clinic staff evaluates the conduct of the resident, his/her knowledge and ability to perform the anesthetic blockade and to identify anatomical structures of the inguinal canal, as well as the ease in performing the standard Lichtenstein technique8 adopted by the Clinic.
4. Results
Of all patients operated, 4.8% were female and 95.2% male. We performed 755 hernioplasties on the right, 394
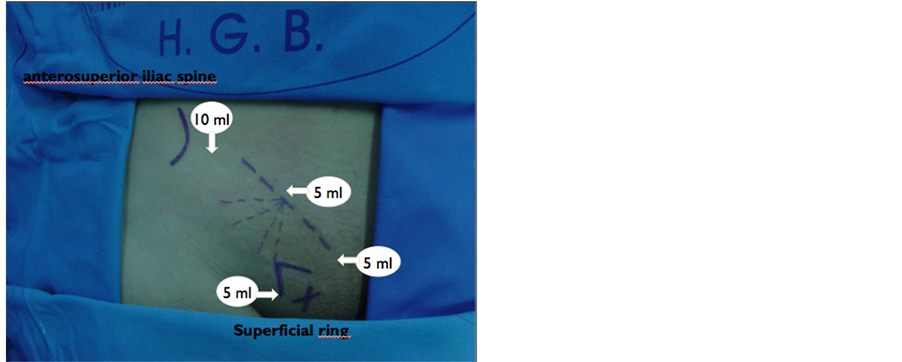
Figure 1. Initial injection, prior to skin incision, respecting palpable anatomic landmarks: anterosuperior iliac spine, incision site, superficial inguinal ring and pubis.

Figure 2. Injection of the external oblique aponeurosis before opening it.
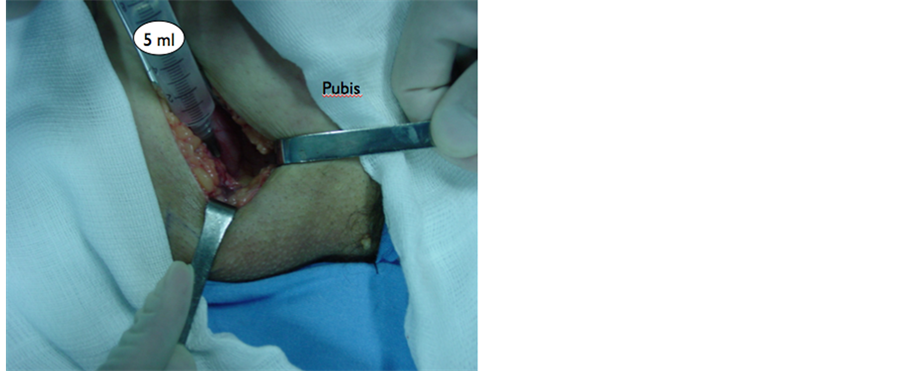
Figure 3. Pubis exposure and infiltration.
on the left and 37 bilateral. With respect to the Nyhus classification, 55% of cases were classified as type II, 24% type III-A, 14% type IIIB and 7% type I. All operations were successfully completed. In neither case a change in the anesthetic method was necessary. Operative time ranged between 40 and 90 minutes, with an average of 65, with no cases of local anesthetics adverse effects. There were seven cases needing assistance by the anesthesiologist, with rapid resolution of the problem (perioperative complications): five cases of sedative side effects (agitation), reversed with the use of specific antagonist; three cases of hypotension. There was no need for hospitalization longer than 24 hours. Regarding the perception of pain, 92% of patients denied feeling any pain, while 8% reported some soreness: grade I in six patients, grade II in three, grade III in one and grade IV in two. When asked about the surgical experience with local anesthesia, all the patients, even those included in the 8% who reported some soreness, said they were satisfied with the treatment received and, should they develop another medical condition that required surgery, they would agree to be submitted to it with use of local anesthesia. There were no deaths. Immediate postoperative complications, defined by presentation between the end of the surgery and hospital discharge were: a case of postural hypotension and another case of wound bleeding, handled with dressing change, without delay in hospital discharge.
Late postoperative complications, defined as being identified from the first postoperative consultation until the last meeting recorded during the study period, were: 1.5% recurrence, the earliest at 6 months and latest after 1 year of follow-up; 5% of chronic pain; 8.2% of wound infection (subcutaneous), without compromising the prosthesis, or surgical outcome (4.4%); one graft rejection; 12% seromas that did not evolve to wound infection; 6.4% complaints of paresthesia; 8% wound hematomas; 3% of swelling of the surgical scar, without the presence of seroma or infection; 0.47% of orchitis.
5. Discussion
The work of Lichtenstein [6] , developed in his clinic in California, shows 2000 patients operated on by his technique without hospitalization and with local anesthesia with absence of severe complications or deaths, and a recurrence rate below 1%. In Brazil, the work of Silva [11] held in Porto Alegre, comparing the conventional outpatient inguinal hernia repair without hospitalization, showed similar complication rates between procedures with and without hospitalization, with costs to the institution 20% lower. This same study noted the impact in significantly reducing the waiting list, similar to results found in this study. Confirming the impression about this aspect, we mention the work published by Neto [12] , which also consistently emphasizes the presented method. In a recent study conducted in our institution, and presented in Las Vegas Physical Medicine and Rehabilitation International Conference (August 19-23, 2014), Sá Ribeiro has compared the costs and time of hospital stay of our local anesthesia hernia program with the rest of Rio de Janeiro state public hospitals. The study compared data of 1042 patients submitted to the repair under local anesthesia in our hospital between 2004 and 2012 with 5451 patients submitted to elective inguinal hernia repair in the rest of Rio de Janeiro at the year of 2012. Our mean time of hospital stay was 6 hours, compared to 2.2 days of those interned at other units. Costs with the procedure were up to 75% lower in our institution.
There was also a lower incidence of side effects, such as cardiovascular instability, nausea, vomiting or urinary retention. The patient undergoing local anesthesia is rapidly mobilized after surgery, resulting in shorter hospital stay. In ten years of this program (2004-2014) there was no case of hospitalization about these patients who were submitted to this surgery. Surgical treatment of inguinal hernias is performed in outpatient clinics in about 70% of patients diagnosed with inguinal hernia in continents such as Europe and North America since the early eighties [1] [13] . In Brazil, even with the knowledge of this surgical technique and the incentive to use it for more than two decades, it is still little known and accepted, and presented in national publications with an air of novelty and not as a standard [2] [14] . Keyes published, in 2008 [15] , a review conducted by the American Association for Accreditation of Ambulatory Surgery Facilities on 1,141,418 surgical procedures performed in multiple ambulatory surgery centers, finding 23 deaths, 13 attributed to embolism by autopsy report; only one case was due to complications of the surgical procedure. The procedure most frequently associated with thromboembolic episodes is the abdominoplasty performed at a day-hospital regime. There are very few published reports of deaths resulting from ambulatory hernia operations [2] [16] . Recently Barros et al. [17] tried to highlight the reasons or situations where the need for admission (unscheduled) arises and reported the experience of their service in Portugal, with over 6000 cases of ambulatory surgeries, in an attempt to identify risk factors related to unscheduled hospitalization. Those that were statistically significant were: gynecologic procedures, nausea and vomiting, bleeding, severe pain, and duration of anesthesia over 120 minutes. In that work more than 30% of the procedures were laparoscopic and 40% were inguinal hernia repairs. The latter had, as an important factor, the occurrence of bleeding from the wound immediately after the procedure, approximately 0.2% of hernia ambulatory operations with local anesthesia. The need for an effective pathway for the treatment of less complex surgical disorders, of great socioeconomic impact, with the recognition of inguinal hernia as an important public health problem in Brazil, which keeps a very large number of individuals out of their work posts, and the concern about the need to ensure adequate training to our residents, made in 2004, the First Surgical Clinic of Bonsucesso General Hospital develop actions to ensure achievement of these procedures, without, however, compromising the need of beds for more severe patients. In this context, the “Program for surgery under local anesthesia without hospitalization” arose, in which was introduced the surgical treatment of inguinal hernias along with procedures such as: other abdominal hernias, anorectal surgery and surgical treatment of pilonidal cysts. This program was inspired and adapted to the reality of the institution from the successful experience of the outpatient Piquet Carneiro Polyclinic developed at the University of Rio de Janeiro (UERJ). The lack of resources, the hospital demand focused on high complexity, the care of oncology patients, besides the growing need for organ transplantation, mobilized almost all Bonsucesso General Hospital structure. Even worse, the lack of clear policies for primary care and strong hospital-centered health care “marketing” combine to virtually disable the care of patients with diseases that require a less complex surgery, but of great socioeconomic impact. The waiting list for surgical treatment of patients with inguinal hernia, which stretches for about five years, is observed in most public health units in Rio de Janeiro, compromising the social and financial spheres of the patients and their families and overwhelming the welfare system. Inguinal hernias affect a significant percentage of the active population in addition to compromising the quality of life of the population over 60 years old, constituting a major public health problem. These patients search various health care units in pursue of definitive treatment to allow their return to usual activities. In Bonsucesso General Hospital the most immediate result was the end of the waiting list for surgical treatment of inguinal hernia. The introduction of the project of surgical abdominal wall hernias with local anesthesia without hospitalization, initiated in 2004 by the First Surgical Clinic of the HGB, in accordance with initiative of the then director of the Hospital, Dr. Victor Grabois, who had created the institution’s Short Stay Unit, significantly decreased the waiting list, which was of about six years, a reality that still persists in most Brazilian public hospitals. The program led to a significant improvement in the surgical training of the resident’s body and of the HGB interns [2] , going from the 24 hernia operations in 2003 to 240 in 2009. Thus, the procedure “Inguinal Hernia Surgery with Local Anesthesia in Outpatient Regime” is feasible, without significant perioperative pain, is safely performed by residents under supervision, enabling a fast and secure learning curve, was well accepted by patients, with complications similar to those observed in a conventional herniorrhaphy, allowing a shorter hospital stay and consequently a lower cost and faster access to treatment, which is also easily replicated elsewhere with a good standby team and minimal resources. We sincerely hope that other Brazilian services can adopt this safe and more economical mode of treatment, like other countries have already done a few decades ago with widespread success. The World Health Organization [13] , the British [17] and Portuguese Health Services have recent publications [17] -[19] on their websites encouraging outpatient surgery, making suggestions and supplying algorithms and protocols to facilitate the growth and adoption of these procedures on an outpatient basis.
References
- Zavadinack Netto, M., Prado Filho, O.R., Bandeira, C.O.P., Sales, K.P.F. and Camiloti, T.A. (2000) Herniorrafia Inguinal: Anestesia Local ou Regional? Acta Scientiarum, 22, 621-623.
- Ribeiro, F.A.S. (2009) Cirurgia Ambulatorial. In: Saad Junior, R., Salles, R.O.R., Carvalho, W.R. and Maia, A.M., Eds., Tratado de Cirurgia do CBC, Atheneu, São Paulo, 1467-1481.
- Vater, J. and Gonçalves, M.C.V. (1987) Ampliação do binômio anestesia localpaciente externo: Enfoque especial para as hérnias inguinocrurais. Residência Médica (Rio de Janeiro), 15, 10, 13-14, 17-22.
- Abdu, R.A. (1983) Ambulatory Herniorrhaphy under Local Anesthesia in a Community Hospital. The American Journal of Surgery, 145, 353-356. http://dx.doi.org/10.1016/0002-9610(83)90199-X
- Amid, P.K., Shulman, A.G. and Lichtenstein, I.L. (1994) Local Anesthesia for Inguinal Hernia Repair Step-by-Step Procedure. Annals of Surgery, 220, 735-737. http://dx.doi.org/10.1097/00000658-199412000-00004
- Skinovsky, J., Sigwalt, M.F., Bertinato, L.P., Chibata, M., Moreira, L.M.S. and Granzotto, P.C.D. (2006) Herniorrafia Inguinal Com Anestesia Locorregional—(uso de ropivacaína). Revista do Colégio Brasileiro de Cirurgiões, 33, 224-227. http://dx.doi.org/10.1590/S0100-69912006000400006
- Lichtenstein, I.L. (1970) Hernia Repair without Disability. 1st Edition, Mosby, St. Louis.
- Sakorafas, G.H., Halikias, I., Nissotakis, C., Kotsifopoulos, N., Stavrou, A., Antonopoulos, C. and Kassaras, G. (2001) Open Tension Free Repair of Inguinal Hernias; the Lichtenstein Technique. BMC Surgery, 1, 3. http://dx.doi.org/10.1186/1471-2482-1-3
- Huskisson, E.C. (1974) Measurement of Pain. Lancet, 2, 1127-1131. http://dx.doi.org/10.1016/S0140-6736(74)90884-8
- MEC [Internet]. (2009) Brasília: Ministério da Educação. http://www.mec.gov.br
- Silva, D.N., Griebeler, M.L., Fernandes, S.F., Paixão, L.Q., Pitrez, F.A.B. (2004) Herniorrafia Ambulatorial Comparada a Convencional. Revista do Colégio Brasileiro de Cirurgiões, 31, 287-90. http://dx.doi.org/10.1590/S0100-69912004000500004
- Laurino Neto, R.M., Buchmann, A.A.C.M. and Messias, L.R.R. (2004) Tratamento cirúrgico das hérnias inguinais sob anestesia local em ambulatório. Revista do Colégio Brasileiro de Cirurgiões, 31, 102-106.http://dx.doi.org/10.1590/S0100-69912004000200006
- Castoro, C., Bertinato, L., Baccaglini, U., Drace, C.A. and McKee, M. with the Collaboration of IAAS Executive Committee Members (2007) Day Surgery: Making It Happen. World Health Organization, on Behalf of the European Observatory on Health Systems and Policies.
- Executive Committee of International Association for Ambulatory Surgery (2003) Ambulatory (Day) Surgery—Suggested International Terminology and Definitions. Paris.http://www.iaas-med.com/joomla/index.php
- Keyes, G.R., Singer, R., Iverson, R.E., McGuire, M., Yates, J., Gold, A., Reed, L., Pollack, H. and Thompson, D. (2008) Mortality in Outpatient Surgery. Plastic and Reconstructive Surgery, 122, 245-250.http://dx.doi.org/10.1097/PRS.0b013e31817747fd
- Bay-Nielsen, M and Kehlet, H. (2008) Anaesthesia and Post-Operative Morbidity after Elective Groin Hernia Repair: A Nation-Wide Study. Acta Anaesthesiologica Scandinavica, 52, 169-174. http://dx.doi.org/10.1111/j.1399-6576.2007.01514.x
- Barros, F., et al. (2008) Can We Find Predictive Factors for Unplanned Overnight Admission. Ambulatory Surgery Journal, 14.
- Department of Health (2002) Day Surgery: Operational Guide. Department of Health Publications, London. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4005487
- Lemos, P., Regalado, A., Soares, J. and Alves, E. (2006) A evolução recente da cirurgia ambulatória em Portugal. Resultados do IV Inquérito Nacional. Revista Portuguesa de Cirurgia Ambulatória, 7, 5-15.
NOTES

*Corresponding author.

