International Journal of Clinical Medicine
Vol.4 No.6A(2013), Article ID:33165,6 pages DOI:10.4236/ijcm.2013.46A002
Does Computer Navigation Improve the Results of MIS Technique in Total Knee Arthroplasty?
![]()
1Department of Orthopaedic Surgery, Hospital St. Agustin, Aviles, Spain; 2Department of Orthopaedic Surgery, School of Medicine, University of Oviedo, Oviedo, Spain.
Email: *dhernandezv@meditex.es
Copyright © 2013 Alfonso Fernandez-Noriega et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received March 18th, 2013; revised May 2nd, 2013; accepted May 19th, 2013
Keywords: Knee; Total Knee Arthroplasty; Minimal Invasive Surgery; Computer-Assisted Surgery
ABSTRACT
The Minimal Invasive Surgery (MIS) technique used for knee arthroplasty implantation implies a less aggressive surgery and reduces the aesthetic impact. Its most notable disadvantage is the poor visualization of bone structures, which may lead to alterations in the correct placement of the prosthetic components. Navigation-assisted surgery may help avoid such mistakes, and thus navigation coupled with the MIS technique may be an alternative for the future. This is a prospective randomized study of 50 patients who received a total knee arthroplasty. In 25 cases the MIS technique was used, whereas in the other 25 navigation was also employed. Mean age of the patients was 71.63 years, and the mean body mass index was 31.19. Results were assessed based on the definitive radiographic position of the femoral, tibial, and limb axis prosthetic components, as well as according to the Visual Analogue Scale (VAS), the Knee Society Score (KSS), Western Ontario and McMaster Universities Arthritis Index (WOMAC), Short Form version 12 (SF-12) questionnaires, and the “up-and-go” test. Differences were found between both groups for duration of the procedure (p = 0.0005). No differences were found in the need for analgesics, amount of drained blood, or mean stay time. There were differences regarding the best radiographic position of the tibial component in the navigation group, but not in the final mechanical axis of the limb, even though out-of-range cases were more abundant in the standard-MIS group. At one year after surgery, clinical, functional and quality of life outcomes were similar in both groups. The combined use of surgical navigation and the MIS technique does not yield advantages in terms of limb alignment nor clinical results at one year after surgery.
1. Introduction
Total knee arthroplasty (TKA) is a procedure which normally leads to a reduction of pain, an increase in functioning, and an improved quality of life. Nevertheless, the percentage of patients who state their expectations prior to surgery have not been met is still considerable. In order to lessen surgical aggression and aesthetic impact, the use of Minimal Invasive Surgery (MIS) technique has been recommended in recent years.
Implanting a TKA with a MIS technique aims to perform the intervention by means of a smaller incision and less bloody gestures, and thus a faster recovery and the use of less health resources is to be expected. MIS is defined as a type of surgery which requires a cutaneous incision of less than 10 centimeters, does not damage the quadriceps, does not avert the extensor apparatus, features no femorotibial luxation, and allows for the implantation of a standard arthroplasty [1,2]. The goal is to reduce blood loss, cause a smaller cutaneous scar and less aggression to soft tissue, reduce postoperative pain and thus shorten hospital stay [3-5] while at the same time favoring a greater and faster recovery of mobility.
There are still unanswered questions regarding the outcomes of the TKA-MIS technique, most notably whether it is a reproducible and cost-effective technique. Potential complications have been pointed out, such as a greater risk of malalignment, difficulties to properly see the bone structures and the extraction of dried out bonecutaneous issues such as wound edge necrosis or soft tissue entrapment [6]. Furthermore, disadvantages like the unavoidable and steep learning curve and the longer surgery time are attributed to this technique.
In recent years, computer-assisted surgery (CAS) has been introduced as a supporting technique for TKA placement, allowing the correct mechanical alignment and a good ligamentous balance. There is enough literature on the subject that backs the better alignment of TKA by using CAS, but experience with the MIS-CAS approach is still insufficient. If the usefulness of such combination could be demonstrated, it may be considered as a future reliable alternative.
The aims of our study were:
1) To confirm whether CAS support in TKA implantation using a MIS technique results in a greater accuracy of implant placement than that achieved with the conventional MIS technique.
2) To assess whether the clinical and functional evolution of TKAs implanted with MIS-CAS differ from those of TKAs implanted with the conventional MIS technique.
2. Materials and Methods
This is a prospective randomized study. The series is made up of 50 patients picked from the surgery waiting list. Mean age of the series was 71.63 years (SD = 6.68), and 80% of patients were women. Mean body mass index (BMI) for the series was 31.19 (SD = 4.68). All patients were asked to sign an informed consent form specifically designed for this study, which was approved by the regional Ethics Committee.
The study comprised patients with knee joint degenerative disease (Ahlbäck grade III or IV) with no joint deformities greater than 10˚, and who had received medical or physical treatment for at least 6 months without showing any improvement.
Patients were randomly assigned to one of two groups. The surgeon did not know beforehand which group had been assigned to each patient until the moment of the intervention. The first group (group A) included 25 patients who underwent TKA surgery with MIS technique, whereas the second group (group B) comprised 25 patients who received a TKA placement by means of the MIS-CAS technique.
The preoperative radiographic protocol included conventional antero-posterior, lateral, and axial projections of the patella and CT with “surview” technique, including the hip and ankle joints. In all cases, a single preoperative dose of a first-generation cephalosphorin antibiotic prophylaxis was administered. Low molecularweight subcutaneous heparins were administered as antithrombotic treatment for six weeks starting in the preoperative period. The TriathlonTM (Stryker Orthopaedics, Mahwah, NJ, USA) model was used in all patients; all the components were cemented, and the posterior crucip ate ligament was preserved. In addition, all patients received a prosthetic patella.
The MIS approach used was the “mid-vastus” (Figure 1). Specific instrumentation for MIS technique was employed. In the cases were navigation was required, the wireless Stryker Navigation System (Stryker-Leibinger, Freiburg, Alemania) was utilized. This system comprises a workstation featuring an opto-electronic camera which locates light-emitting sources, or diodes with an error margin of 1 mm (equivalent to a 1˚ orientation error), 2 infrared light-emitting diodes (LED) mounted on screws to be introduced percutaneously in the diaphysis of the femur and the tibia equipped with a lithium battery which does not require any wired connection (Figure 2). Through the emitters, the system collects information about the preoperative status of the limb. During the surgical procedure this helps with the accuracy and direction of the bone cuts, the size of the implant, and the ligamentous status. Finally, it also provides feedback about the final position of the arthroplasty with respect to the limb axis as well as mobility and the definitive ligamentous status in the form of a summary report. All patients followed the same postoperative protocol, resting in bed with compressive bandage and performing isometric

Figure 1. TKA implanted with MIS technique (cutaneous incision of 9 centimeters).

Figure 2. Wireless navigation system in TKA.
quadriceps exercises during the first 48 hours. Afterwards, a guided physiotherapy program was started. Ambulation was authorized on the third day, with the help of two walking sticks. During the first 48 hours, an intravenous perfusion of 300 mg of tramadol every 24 hours was administered, plus 1 g of paracetamol intravenous rescue doses every 8 hours if the patient experienced pain.
Discharge criteria were the lack of need of major analgesics, ambulatory capability with walking stick, no temperature above 37.5˚C, no wound secretion, no hematoma, and a minimum knee flexo-extension mobility of 90˚.
Patients were examined at 12 months after surgery. The assessment comprised knee radiographies in two projections, CT of the lower limb including hip, knee, and ankle, and filling out the visual analog scale (VAS) for pain and satisfaction (with scores from 1 to 10), the KSS, WOMAC, and SF-12 questionnaires, and the “upand-go” test.
For the statistical analyses, the EPI 6 statistical package was used. A descriptive analysis of the data was performed at baseline using frequency distribution for the qualitative/quantitative variables categorized. For the description of the quantitative variables, the mean has been taken as measurement of the central trend, and the standard deviation as dispersion measurement. The statistical analysis was carried out with Student’s t-test. Quantitative variable normality was checked both graphically and with the Kolmogorov-Smirnov test. Hypothesis contrasts for qualitative variables were performed with Chi-square test or Fisher’s exact text when the required conditions for the former were not met.
3. Results
No patient was lost to follow-up. Both groups were homogeneous in terms of epidemiological features, clinical status before intervention, and alignment of the femorotibial axis.
3.1. Intraoperative Variables
Mean length of the incision was 10.92 cm (SD = 0.86) in group A and 11.32 cm (SD = 0.92) in group B, with no statistically significant differences (p = 0.12). Group B required more surgery time, with a mean of 128.8 minutes (SD = 26.78) as opposed to 104.4 minutes (SD = 19.11) for group A (p = 0.0005).
3.2. Immediate Postoperative Variables
Results of hemoglobin decrease measured in g/dl during the immediate postoperative period did not yield any significant differences between both groups. The mean loss for group A was 1.72 g/dl (SD = 0.81) and 1.68 (SD = 0.74) for group B (p = 0.85). No significant differences were found either in the volume collected by the drainages: mean 615.6 cc (SD = 419.73) for group A and a mean of 686.8 cc (SD = 365.25) for group B (p = 0.52).
The analysis of the results showed there were no significant differences when comparing the mean dose of rescue analgesics administered to each group during the first 48 hours (group A = 1.04, SD = 1.24; group B = 1.32; SD = 1.31). No differences were present for the length of hospital stay in days (group A = 6.96; SD = 1.48; group B = 7.12; SD = 1.26) either.
At discharge, no objectively significant differences were observed between both groups regarding mobility, neither in extension, flexion nor total range of mobility.
3.3. Component Alignment
A postoperative CT was performed in all patients (Figure 3) in order to assess the sagittal mechanical alignment. Results show that there exists a significant difference between both groups when it comes to the alignment of the tibial component (TA) (p = 0.008). No differences were present in the alignment of the femoral component (FA) (p = 0.58) nor in the alignment of the femorotibial axis (FTA) (p = 0.13) (Table 1).
Group A exhibited a higher number of cases beyond alignment limits, which were set at ±3˚ (8 cases for FA, 6 for TA, and 11 for FTA). In group B, only 2 cases were found for FA, 3 for TA, and 5 for FTA. The percentage of outlier cases in each group for FA, TA, and FTA is shown in Table 2. Significant differences were only present between groups in the alignment of the femoral component (p = 0.033).
3.4. Status of Patients at One Year after Surgery
No significant differences were found in the mobility of the operated knee, VAS, the “up-and-go” test, the KSS
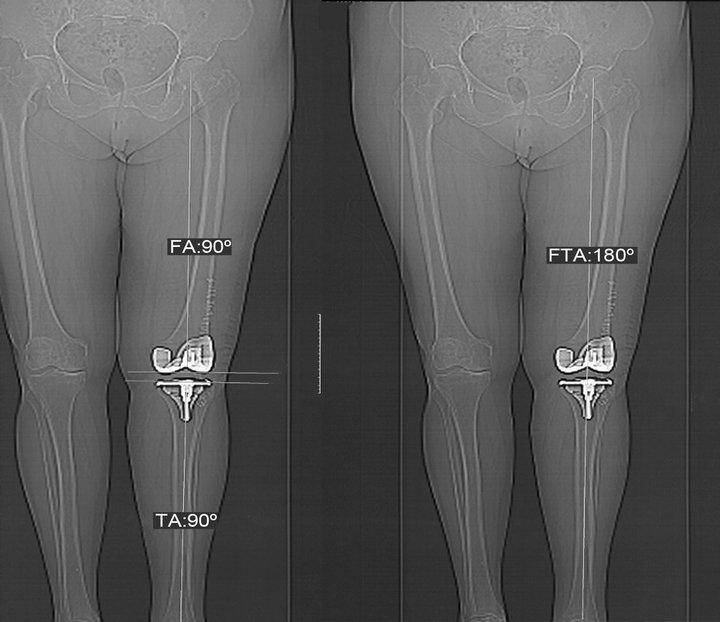
Figure 3. Measurement of femoral angle (FA), tibial angle (TA) and femorotibial angle (FTA) in the postoperative.
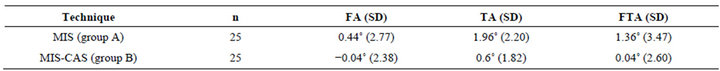
Table 1. Results of alignment after implantation of the arthroplasty in the operated knee for the study groups. Positive values express varus deformity, whereas negative values express valgus deformity. FA: femoral angle, TA: tibial angle, FTA: femorotibial angle.

Table 2. Outliers percentage in FA, TA, and FTA.
questionnaire and its sub-scales, the WOMAC questionnaire and its sub-scales, or the SF-12 (Table 3).
No major complications happened in any of the groups. The rate of minor complications was 12% for the MIS group and 8% in the MIS-CAS group. None of these complications required additional surgery time nor produced delays in hospital stay time.
4. Discussion
When following the standard technique for TKA implantation, the equipment used aims to place the implants following the mechanical axis of the limb. These systems are based on standardized geometrical measurements or subjective impressions, lacking any individualization when it comes to anatomical peculiarities. Usually, this procedure is performed through an internal anterior parapatellar incision of about 15 cm. The MIS technique for TKA was introduced in clinical practice in order to reduce the aesthetical impact while aiming to reduce soft tissue aggression and also allow for a faster recovery. There are no contraindications for performing this technique, although the literature does mention some factors which may complicate this type of surgery, such as overweight, muscular hypertrophy, previous surgery, or low patella position [7].
CAS adds safety to bone cuts, customizes the technique and the final angulation, allows reproducing the procedure while avoiding subjective impressions, and ensures the proper final results in terms of alignment and ligamentous status.
By combining both techniques, MIS and CAS, we aimed to introduce a quality control for patients operated with MIS. CAS avoids errors derived from a defective visualization of structures, a complication present when using MIS.
We did not find differences between the length of the incision irrespectively of whether CAS was used or not. Blood loss was similar in both groups. The values show that MIS techniques provoke less bleeding than the standard technique, as described in the literature [8,9]. The
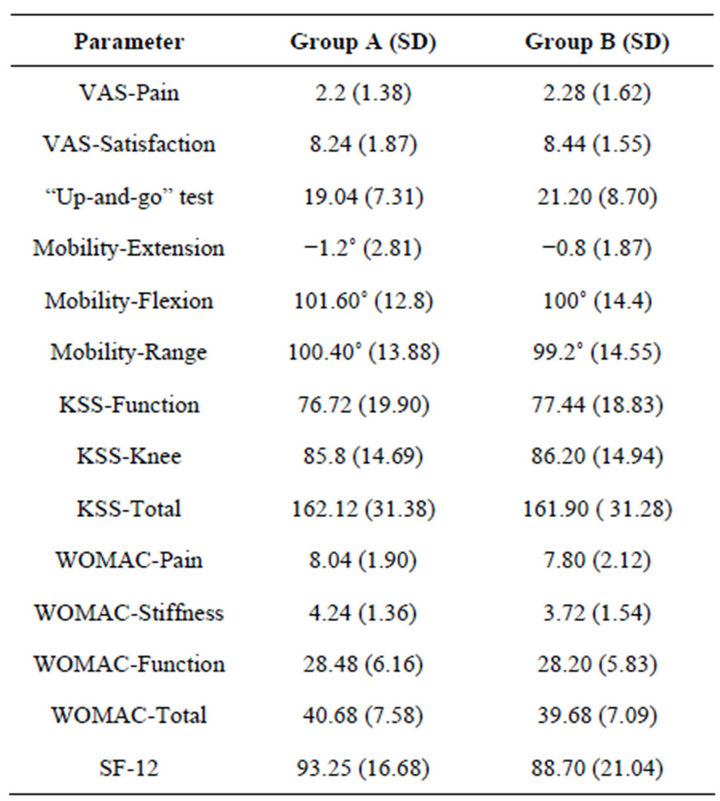
Table 3. Clinical, functional, and quality of life outcomes at one year after surgery.
increase of surgery time (by 18%) in the MIS-CAS group did not cause a higher complications rate in our study.
In order to assess pain during the immediate postoperative period, we analyzed the amount of rescue doses of analgesics required by the patients. Differences were not statistically significant between groups. Measuring pain is a complex issue, since it is a subjective perception, and thus difficult to grade. In other similar studies, the analgesia used was measured according to its morphine equivalent [9], total amounts of analgesics [10], visual pain scales or other grading scales. Nevertheless, the results found in these other studies always point to less pain or at least less use of analgesics in patients operated with MIS techniques as opposed to the conventional technique [8].
No statistically significant differences were found in length of hospital stay between both groups. Measurements of knee mobility at the time of hospital discharge showed no differences either. Previous studies support the supposition that the MIS technique favors a faster rehabilitation and a quicker return to normal life, although we do not have comparative studies between MIS and MIS-CAS at our disposal.
As for radiographic alignment, we discovered that even though the results in the MIS-CAS group were more accurate, the excellent accuracy rates achieved in the arthroplasties performed in the MIS group made any differences only noticeable in partial measurements, but not in the final axis of the limb. Previous publications find higher placement accuracy in the femoral [11-13] and tibial [12-14] components, together with an improved alignment of the femorotibial mechanical axis [13] when CAS is used. In our study, however, we only found significant differences in the placement of the tibial component. No differences were found for the position of neither the femoral component or the mechanical axis of the limb. Nevertheless, in the case of patients with outof-range axis angulations ±3˚ (outliers), we did find notably statistically significant decreases in the MIS-CAS group. Outlier measurement is the main reference some meta-analyses employ [15-17] to confirm the higher accuracy in prosthetic component alignment when CAS is used. It seems there is a consensus that the main advantage of navigation is a decrease of cases of alignment outside the optimal range [18].
Among the limitations of our work, the small number of patients assessed, the short follow-up period, and the absence of cases featuring intraor extra-articulatory deformities must be taken into account. At one year after implantation, the clinical and functional outcomes of both techniques were the same, making it impossible to state which one is better. Neither range of mobility, functional and pain scales, nor quality of life differ at that moment, a fact that puts into question the indication of CAS for the support of the MIS technique. CAS features a proven utility in major extraor intra-articulatory deformities [19] or with hardware material after osteosynthesis. In knees featuring light deformities, surgical navigation with or without MIS is questioned, and further, longer term studies are needed to demonstrate its use and recommend its implementation in routine clinical practice.
5. Conclusion
When the MIS technique is used for TKA, CAS support does not improve the final limb axis. There are no significant differences in the results when comparing the outcomes of MIS vs. MIS-CAS techniques neither in the immediate postoperative period nor in the clinical, functional, and quality of life parameters at one year after surgery.
REFERENCES
- R. S. Laskin, B. Beksac, A. Phongjunakorn, K. Pittors, J. Davis, J. C. Shim, H. Pavlov and M. Petersen, “Minimally Invasive Total Knee Replacement through a Mini-Midvastus Incision: An Outcome Study,” Clinical Orthopaedics and Related Research, Vol. 428, 2004, pp. 74-81. doi:10.1097/01.blo.0000148582.86102.47
- S. B. Haas, S. Cook and B. Beksac, “Minimally Invasive Total Knee Replacement through a Mini Midvastus Approach: A Comparative Study,” Clinical Orthopaedics and Related Research, Vol. 428, No. 11, 2004, pp. 68-73. doi:10.1097/01.blo.0000147649.82883.ca
- J. B. Reid 3rd, D. Guttmann, M. Ayala and J. H. Lubowitz, “Minimally Invasive Surgery-Total Knee Arthroplasty,” Arthroscopy, Vol. 20, No. 8, 2004, pp. 884-889. doi:10.1016/j.arthro.2004.07.021
- E. M. Goble and D. F. Justin, “Minimally Invasive Total Knee Replacement: Principles and Technique,” Orthopaedics Clinical North American, Vol. 35, No. 2, 2004, pp. 235-245. doi:10.1016/S0030-5898(03)00113-5
- A. J. Tria, “Minimally Invasive Total Knee Arthroplasty: The Importance of Instrumentation,” Orthopaedics Clinical North American, Vol. 35, No. 2, 2004, pp. 227-234. doi:10.1016/S0030-5898(03)00118-4
- P. M. Bonutti, M. G. Zywiel, S. D. Ulrich, M. S. McGrath and M. A. Mont, “Minimally Invasive Total Knee Arthroplasty: Pitfalls and Complications,” American Journal of Orthopaedics, Vol. 39, No. 10, 2010, pp. 480-484.
- R. S. Laskin, “Minimally Invasive Total Knee Replacement Using a Mini-Mid Vastus Incision Technique and Results,” Surgical Technologie Internationale, No. 13, 2004, pp. 231-238.
- D. Hernández-Vaquero, A. Noriega-Fernández and A. Suárez-Vázquez, “Total Knee Arthroplasties Performed with a Mini-Incision or a Standard Incisión. Similar Results at Six Months Follow up,” BMC Musculoskeletal Disorders, Vol. 11, 2010, p. 27. doi:10.1186/1471-2474-11-27
- A. Tanavalee, S. Thiengwittayaporn and P. Itiravivong, “Results of the 136 Consecutive Minimally Invasive Total Knee Arthroplasties,” Journal Medical Association Thai, 2005, Vol. 88, Suppl. 4, pp. S74-S78.
- Y. Hoo Kim, K. S. Sohn and J. D. Kim, “Short-Term Results of Primary Total Knee Arthroplasties Performed with a Mini-Incision or a Standard Incision,” Journal of Arthroplasty, Vol. 21, No. 5, 2006, pp. 712-718. doi:10.1016/j.arth.2005.09.001
- A. Ensini, F. Catani, A. Leardini, M. Romagnoli and S. Gianinni, “Alignments and Clinical Results in Conventional and Navigated Total Knee Arthroplasty,” Clinical Orthopaedics and Related Research, Vol. 457, No. 4, 2007, pp. 156-162.
- G. Matziolis, D. Krocker, U. Weiss, S. Tohzt and C. Perka, “A Prospective, Randomized Study of Computer Assisted and Conventional Total Knee Arthroplasty. ThreeDimensional Evaluation of Implant Alignment and Rotation,” Journal of Bone and Joint Surgery, Vol. 89, No. 2, 2007, pp. 236-243. doi:10.2106/JBJS.F.00386
- D. Zorman, P. Etuin, H. Jennart, D. Scipioni and S. Devos, “Computer Assisted Total Knee Arthroplasty: Comparative Results in a Preliminary Series of 72 Cases,” Acta Orthopaedica Belgica, Vol. 71, No. 6, 2005, pp. 696-702.
- S. K. Chauhan, R. G. Scott, W. Breidahl and R. J. Beaver, “Computer Assisted Knee Arthroplasty versus a Conventional Jig-Based Technique. A Randomized Prospective Trial,” Journal of Bone and Joint Surgery, Vol. 86, No. 3, 2004, pp. 372-377. doi:10.1302/0301-620X.86B3.14643
- M. Sparmann, B. Wolke, H. Czupalla, D. Banzer and A. Zink, “Positioning of Total Knee Arthroplasty with and without Navigation Support. A Prospective, Randomized Study,” Journal of Bone and Joint Surgery, Vol. 85, No. 6, 2003, pp. 830-835.
- J. B. Mason, T. K. Fehring and R. Estok, D. Banel and K. Fahrbach, “Meta-Analysis of Alignment Outcomes in Computer-Assisted Total Knee Arthroplasty Surgery,” Journal of Arthroplasty, Vol. 22, No. 8, 2007, pp. 1097- 1106. doi:10.1016/j.arth.2007.08.001
- Y. S. Brin, V. S. Nikolaou, L. Joseph, D. J. Zukor and J. Antoniou, “Imageless Computer Assisted versus Conventional total Knee Replacement. A Bayesian Meta-Analysis of 23 Comparative Studies,” International Orthopaedics, Vol. 14, No. 3, 2010, pp. 31-39.
- P. M. Bonutti, D. A. Dethmers, M. S. McGrath, S. D. Ulrich and M. A. Mont, “Navigation Did Not Improve the Precisión of Minimally Invasive Knee Arthroplasty,” Clinical Orthopaedics Related Research, Vol. 466, No. 11, 2008, pp. 2730-2735. doi:10.1007/s11999-008-0359-4
- D. Hernandez-Vaquero, A. Suarez Vazquez, M. A. Sandoval-Garcia and A. Noriega-Fernandez, “Computer Assistance Increases Precision of Component Placement in total Knee Arthroplasty with Articular Deformity,” Clinical Orthopaedic Related Research, Vol. 468, No. 5, 2010, pp. 1237-1241. doi:10.1007/s11999-009-1175-1
NOTES
*Corresponding author.

