International Journal of Clinical Medicine
Vol.3 No.4(2012), Article ID:20869,3 pages DOI:10.4236/ijcm.2012.34050
Relationship between Cognition and Activities of Daily Living in Elderly Women with Mild Cognitive Impairment in Japan
![]()
1Department of Nursing, Kyoto Koka Women’s University, Kyoto, Japan; 2College of Health and Human Science, Osaka Prefecture University, Osaka, Japan; 3Division of Health Sciences, Graduate School of Medicine, Osaka University, Osaka, Japan.
Email: m-yamamoto@mail.koka.ac.jp
Received March 7th, 2012; revised April 12th, 2012; accepted May 27th, 2012
Keywords: Woman’s Elderly; Cognitive Function; ADL; Community
ABSTRACT
Purpose: This study aims to examine the relationship between cognition and ADL in elderly women with MIC. Methods: Cognitive function was assessed using a 4-item instrument screening for dementia. Each item was scaled from 1 to 4. The Katz Index was used to Participants (N = 680) were asked to return the completed questionnaire in the sealed envelope provided. The study received approval from the human subject’s ethics committee at Osaka University. Results and Conclusion: Participants’ mean age was 78.2 ± 6.5 years old. The age range of participants was 65 to 97 years old. Associations were not statistically significant between cognitive function and family structure. However, associations were significant for ADL items involving excretory failure (OR = 3.5, p = 0.000 in 2004, OR = 2.9, p = 0.000 in 2005; P < 0.05) using a logistic regression analysis adjusted for age. Therefore, we recommend that nurses work to educate the public about treatment-adjusted dementia in the community, teaching family members or caretakers to observe the ADL of the elderly, being watchful for unusual excretory habits, extra clothes, or the smell of elderly persons’ dirty clothing.
1. Introduction
Mild cognitive impairment (MCI) is a relatively recent term used to describe people who have some memory problems, but do not actually have dementia. In recent years, some drug treatments that can improve the symptoms of Alzheimer’s disease (AD) have become available [1,2]. Other treatments that may slow down the progression of AD in the brain are also being developed. It is important that people with AD be identified as early as possible, so that they can benefit from these treatments in the future. Identifying people with MCI is one way to try to achieve this. Moreover, Basic activities of daily living (ADL) are self-maintenance abilities such as dressing or bathing [1]. ADL questionnaires play an important role in assessing the functional abilities of older adults and evaluating the impact of cognitive impairment on routine activities [3]. However, it is difficult to assess activities of daily living (ADL) impairment among elderly women with mild cognitive impairment (MCI) using existing scales [4,5]. Moreover, these scales do not allow for detailed assessment of ADL.
2. Purpose
This study aims to examine the relationship between cognition and ADL in elderly women with MIC.
3. Methods
Six hundred and eighty-two elderly women were enrolled in a longitudinal study from cities and towns surrounding Osaka. All participants had not received treatment for any diseases and had reported having not fallen in the previous year. All participants were also receiving at-home care. Questionnaires were mailed to participants in 2004 and again in 2005. Cognitive function was assessed using a 4-item instrument screening for dementia. Each item was scaled from 1 to 4. The Katz Index was used to measure ADL, which contained a 6-item instrument scaled from 1 to 6 points [6]. The questionnaire also asked about sexuality, age, family structure, experiences while receiving treatment and episodes of falling within a year. A logistic regression analysis was conducted to examine the association of cognitive function as a dichotomous variable with various characteristics of ADL. The association between cognitive function and
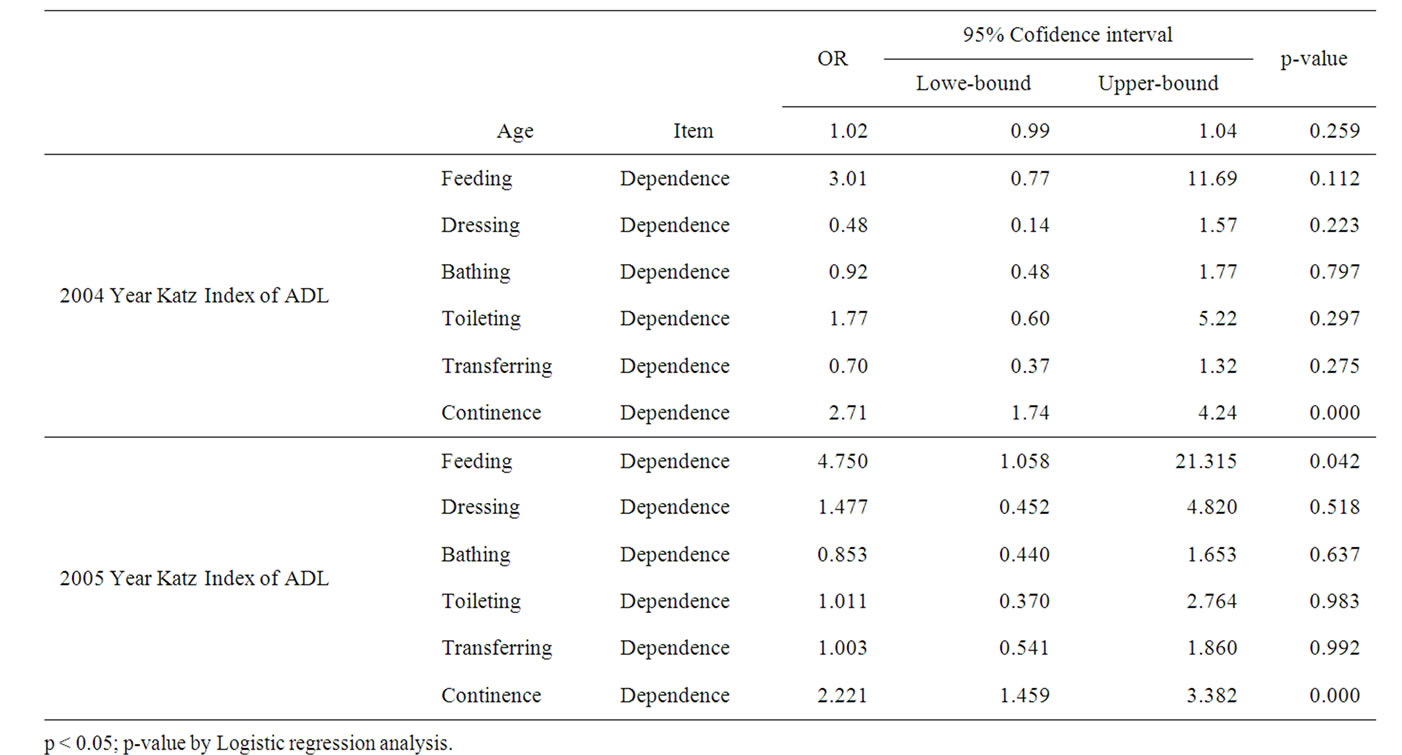
Table 1. Logistic-regression analysis result that MIC of a dependent variable in 2004-2005.
ADL was adjusted for age in the analysis. Finally, it was Ethics Approval of this study, because the questionnaire was self-administered, participant’s privacy was ensured and others were not aware of their responses. Responses remained anonymous to study investigators through the use of unique identifiers for each questionnaire. Participants were asked to return the completed questionnaire in the sealed envelope provided. The study received approval from the human subject’s ethics committee at Osaka University.
4. Results
Participants’ mean age was 78.2 ± 6.5 years old. The age range of participants was 65 to 97 years old. Associations were not statistically significant between cognitive function and family structure. However, associations were significant for ADL items involving excretory failure (OR = 3.5, p = 0.000 in 2004, OR = 2.9, p = 0.000 in 2005; p < 0.05) using a logistic regression analysis adjusted for age (Table 1).
5. Conclusion
These results suggest that ADL involving excretory failure are associated with elderly women with MCI living in the community. This results similar to articles in Japan [7]. This type of problem may be difficult for others to recognize. Women has feel shame when seeking assistance regarding excretory problems [8]. Furthermore, elderly women also may feel shame when seeking assistance regarding excretory problems [9,10]. Therefore, we recommend that nurses work to educate the public about treatment-adjusted dementia in the community, teaching family members or caretakers to observe the ADL of the elderly, being watchful for unusual excretory habits, extra clothes, or the smell of elderly persons’ dirty clothing.
6. Acknowledgements
The authors are very grateful to all the respondents from the participants.
REFERENCES
- B. P. Leifer, “Alzheimer’s Disease: Seeing the Signs Early,” Journal of the American Academy of Nurse Practitioners, Vol. 21, No. 11, 2009, pp. 588-595. doi:10.1111/j.1745-7599.2009.00436.x
- J. Corey-Bloom and D. Galasko, “Adjunctive Therapy in Patients with Alzheimer’s Disease. A Practical Approach,” Drugs Aging, Vol. 7, No. 2, 1995, pp. 79-87. doi:10.2165/00002512-199507020-00002
- G. Sanchez-Benavides, et al., “Spanish Version of the Bayer Activities of Daily Living Scale in Mild Cognitive Impairment and Mild Alzheimer Disease: Discriminant and Concurrent Validity,” Dementia and Geriatric Cognitive Disorders, Vol. 27, No. 6, 2009, pp. 572-578. doi:10.1159/000228259
- E. Mariani, R. Monastero and P. Mecocci, “Mild Cognitive Impairment: A Systematic Review,” Journal of Alzheimer’s Disease, Vol. 12, No. 1, 2007, pp. 23-35.
- S. Alladi, et al., “Mild Cognitive Impairment: Applicability of Research Criteria in a Memory Clinic and Characterization of Cognitive Profile,” Psychological Medicine, Vol. 36, No. 4, 2006, pp. 507-515. doi:10.1017/S0033291705006744
- M. P. Lawton and E. M. Brody, “Assessment of Older People: Self-Maintaining and Instrumental Activities of Daily Living,” Gerontologist, Vol. 9, No. 3, 1969, pp. 179-186. doi:10.1093/geront/9.3_Part_1.179
- N. Nakanishi, et al., “Urinary and Fecal Incontinence in a Community-Residing Elderly Population: Prevalence, Correlates and Prognosis,” Nihon Koshu Eisei Zasshi, Vol. 44, No. 3, 1997, pp. 192-200.
- L. Semere and N. M. Nour, “Obstetric Fistula: Living with Incontinence and Shame,” Reviews in Obstetrics and Gynecology, Vol. 1, No. 4, 2008, pp. 193-197.
- R. N. Butler, et al., “Urinary Incontinence: Keys to Diagnosis of the Older Woman,” Geriatrics, Vol. 54, No. 10, 1999, pp. 22-26, 29-30.
- O. Contreras, “Stress Urinary Incontinence in the Gynecological Practice,” International Journal of Gynecology & Obstetrics, Vol. 86, Suppl. 1, 2004, pp. S6-S16. doi:10.1016/j.ijgo.2004.05.004

