International Journal of Clinical Medicine
Vol.3 No.2(2012), Article ID:17868,5 pages DOI:10.4236/ijcm.2012.32018
Undergraduate Pathology Education: Meeting the Challenge Ahead
![]()
1Department of Pathology, S. C. B. Medical College, Cuttack, India; 2Department of Obstetrics & Gynecology, S. C. B. Medical College, Cuttack, India; 3Department of Pathology, IMS & SUM Hospital, Siksha “O” Anusandhan University, Bhubaneswar, India; 4Department of Oncopathology, Acharya Harihar Regional Cancer Centre, Cuttack, India.
Email: *drpallavibhuyan@gmail.com
Received December 14th, 2011; revised January 26th, 2012; accepted February 8th, 2012
Keywords: Undergraduate Pathology Education; Problem Based Learning; Multidisciplinary Integrated Teaching
ABSTRACT
Background: In India, undergraduate medical education has remained more or less static and for last so many decades no effective development has been done. Therefore this study is done for restructuring it and to meet the challenges faced thereby. Material and Methods: Depending on the problems faced during undergraduate pathology teaching, questions were prepared and sent to pathology teachers of Odisha. In few aspects, suggestions were also asked for modification of the present system of medical curriculum including the problem of factual or information overload on students. Results: 18 questions were prepared and asked to 96 pathology teachers. The opinions mostly were to introduce small group teaching or problem based learning (PBL) and multidisciplinary integrated teaching. The opinion of students of 3rd and 4th MBBS were also taken into consideration for taking the decisions of modification. Conclusion: Efforts should be taken to bring the desired changes in undergraduate pathology education to produce need based human resources for health care in society.
1. Introduction
During last few minutes on earth, Dr. Virchow Robbins had told “Let me share a few thoughts about pathology education. All medical teaching is a humanitarian endeavour. Medical education does not exist to provide students with a way of making a living but to ensure the health of the community. Your job is to educate the other physicians so they may diagnose and treat disease. Learning treatment is easy. Understanding pathology is the hardest task of the young physicians.” It is the pathologists who must equip all other physicians to treat patients. Therefore teaching of pathology comes ahead of all other fraternities and its importance is unparalleled.
In most of the medical colleges, existing medical training provides a general education in a variety of subjects relevant to a doctor’s need and this broad base has made a significant contribution to the problem of information overload [1]. One must address the problem of factual or information overload in curriculum. There are attempts to delineate the core curriculum and options provide areas depending on individual needs and interests. Instead of the general burden,emphasis is being put on in depth work and high level or critical thinking. One must try education for capability by practical training and generic competencies. But the recent undergraduate curriculum fails to fulfil this expectation despite students’ extensive exposure to clinical teaching [1-4]. Taking into account of the existing system, their loopholes and inability to fulfil the demand of the society, this study is undertaken addressing the present methods keeping in view the changes in need in recent future. It has involved the faculty along with the students, their opinions, suggestions and the most relevant recommendations thought of thereby.
2. Materials and Methods
The pivot around which the medical education should be based is mostly the integrated medical learning. On one hand are the knowledge, interests, attitude and aspirations and on the other subject matters, teaching methods, teachers and departmental environments. And if one analyses and summarises these points, medical education system can be divided into 3 broad dimensions i.e. integrated medical curriculum or curriculum developement, faculty development and student assessment. Basing on these a questionnaire was prepared consisting of 18 questions for optimum development of each of these. They were again subdivided into small groups centered around a particular objective and at places suggestions were asked which can be incorporated into the study and some conclusive opinion can be formed.
This questionnaire format was sent to all pathology teachers (both working and retired) of the state of Odisha. Most of them are working in one of the 3 Government medical colleges or 3 private medical colleges. The answers and/or suggestions to the asked questions were compiled and a solution was formed depending on the majority for modification/restructuring of present undergraduate pathology education system.
3. Results
In the present study we sent the questionnaire to 96 pathology teachers which include 77 faculty and 19 retired teachers. State of Odisha has 3 government medical collages and 3 private medical colleges. Out of them, 27 are professors, 18 associate professors and 51 assistant professor (Table 1). A questionaire of few questions was also selected for the undergraduate medical students of 2nd and 3rd years (3rd - 5th Semestar) studying pathology. An assessment was made of their interest, approach and likely way of learning and the results were also incorporated into the study.
The questions subdivided into small groups of 4 - 5 numbers with answers:
1) Innovate and develop the medical curriculum or curriculum development:
Best utilization of 1 hour lecture can be done by:
(1) Macroscopic and/or microscopic preparations/illustrations about the conditions discussed in each class
A. Will be beneficial (88) B. Not up to mark (3) C. Difficult (5)
(2) Problem based learning/structured display
A. Should be employed (78) B. No (12) C. Not possible (6)
(3) MCQs for last 5 - 10 minutes following lecture to be answered by key pad by students
A. Necessary (40) B. Will not help (12) C. Infrastructure needed (44)
(4) MCQs after completion of each chapter (answered in paper)

Table 1. Pathology teachers of Odisha (n = 96).
A. Beneficial, should be classroom (74) B. Will not help (6) C. Beneficial, can be done in hostel (16)
Learning pathology from diverse format:
(1) What is more reproducible?
A. Class room teaching (35)
B. Small group teaching or PCCI (61)
(2) Small group students teaching with facilitator or PCCI:
A. Should be started (61) B. Not necessary (14) C. Is not possible (21)
(3) Combined teaching by faculty in pathology in clinical subjects
A. Should be conducted (62) B. Not of help (7) C. Cannot be conducted (27)
(4) CME in pathology should be conducted at an interval of
A. 6 months (43) B. 1 year (10) C. More frequently(36) D. Will not help (7)
(5)Integrated teaching programme to avoid unnecessary repetition
A. Teach once in any fraternity (8) B. Repetition is necessary (27)
C. Multidisciplinary integrative learning (61)
2) Building of an efficient intellectuals committed faculty or faculty development:
It is the foremost responsibility of the authority of any teaching institute. The questions were
(1) Change in selection method of teachers
A. Necessary (24) B. Not necessary (22)
C. Should be carriers, viva, group discussion among applicants (50)
(2) Reorientation training course for teachers for a period of
A. 3 month (52) B. 6 month (30) C. Not necessary(14)
(3) Evaluation of faculty should be done
A. At yearly interval (44) B. At 5 years interval(35) C. Not necessary (17)
(4) Assessment of teachers to be done by students
A. Yes (10) B. No (25) C. Yes but should be kept confidential (61)
(5) Awards should be given to faculty
A. National level (5) B. State level (11) C. Both (76) D. Nil (4)
3) Performance or assessment of Students:
(1) Strengthening academic performance of students by giving
A. Scholarship (39) B. Awards (47) C. Won’t be effective(10)
(2) Projects to be given for a short period from own medical colleges with rewards
A. Yes (65) B. No (13) C. Funds problem (18)
(3) Change in assessment through theory examination of students like MCQs and short questions and answers instead of long questions
A. Approve (78) B. Don’t approve (18)
(4) Change in practical assessment of students
A. Yes (20) B. No (24) C. Any suggestions (56)
Students’ perspective:
(1) Which method of teaching do you appreciate
A. Audiovisual (6%) B. Blackboard (36%) C. Both (58%)
(2) Attending clinic-pathological meetings
A. Yes (56%) B. Inconvenient (44%)
(3) Multidisciplinary teaching by both pathologists and clinicians
A. Yes (70%) B. No (08%) C. Can’t be done (22%)
(4) CME should be done
A. At 6 month interval (40%) B. More frequent (32%) C. Won’t help (28%)
(5) Home work on the taught chapter
A. Yes (48%) B. No (20%) C. Load will be more (32%)
4. Discussion
At the time of independence in 1947, India has just 20 medical colleges admitting about 3000 students. Sixty years later the number of colleges has reached 13 fold and the number of seats has reached to 30,000 [5]. Despite the numbers, quality still remains more or less static. Majority of colleges lack even the minimum infrastructure. This poor state of medical education prompted us to carry out this study, analyze the data and provide some concrete recommendations.
During the second year, students learn the basic principles of pathology and make clinical correlations in patient case studies to move forward in their medical career. Therefore it is the pathology faculty who must give first in depth exposure to human diseases to the students. Hence they should utilize the 1 hour lecture in the best possible way. The lecturers should plan their lecture in such a way that it could arouse interest and deeply motivate the students and should target student needs, attitudes, incentives, clear understandings. After analysis of the questions and answers, it was derived that one should break up the 1 hour into 45 minutes lecture and last 15 minutes for showing macroscopic/microscopic illustrations, ask MCQs or questions after each lecture/chapter or go for a problem based learning (Table 2).
Problem based learning or presenting students with problems to solve is a useful approach to pathology education. It is described as one of the most significant development in professional education, which was pioneered by the Mc Master Medical School in Canada in 1969 [6].
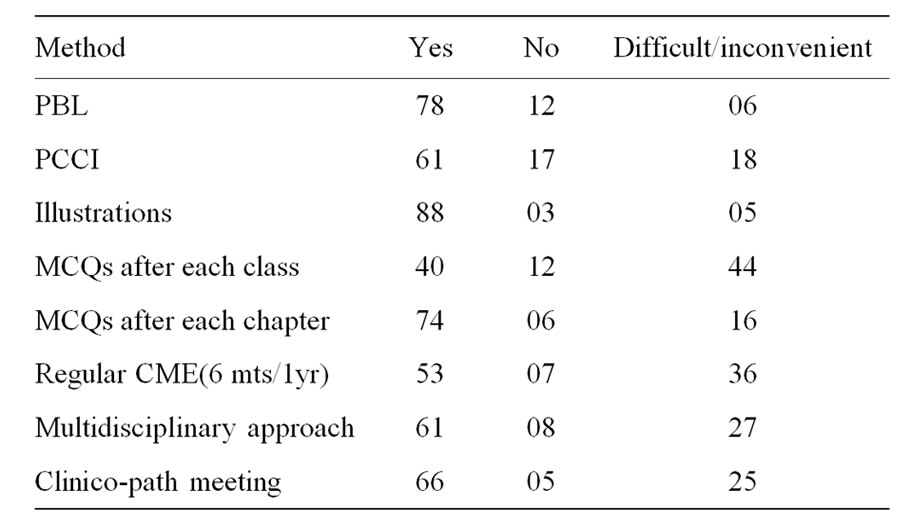
Table 2. Teaching methods.
PBL is a learner centered method where students learn by working on real life problems and teacher acts as a facilitator. It is more effective than learning based on established disciplines and can solve problems of traditional curriculum. It has been started in some centers of India, a welcome step. PCCI (Small group student teaching with facilitator) is another format of teaching in small groups of 8 - 10 students for around 12 weeks with a facilitator. The topics can be either student driven or determined by the specific teaching block.
It has been felt that in recent system exposing the students to a succession of subjects studied in different departments is not effective for producing competent physicians [1,7]. It is wasteful because of unnecessary repetition, disjoined and confusing (due to departmental differences of opinion). To solve this, in the early 1950s, the Cape Western Reserve University initiated an “Integrated teaching programme” [8]. Integrative learning in medical science is non-compartmentalised approach. Integrated curriculum alternates lectures on the same subject by different clinical and pathological faculty. This can be achieved if the course of study organises around organ systems. This is difficult to carry out but it can be highly beneficial for the students.
The total development of any teaching institute depends solely on performance of its students. And the major contribution to it comes from its dedicated faculty. The pathology faculty should be committed in making the undergraduate educational experience rewarding and successful. So for building a strong assured committed faculty five questions wear put and the opinions were derived.
Selection of medical teachers should be strict taking into account career, viva, presentation, personality and group discussion. Initiation of teachers training programs in some medical colleges have led to increased interest in teaching methods and research activities. The overall outcome is encouraging and an educational environment for change is beginning to emerge in medical education [9- 12]. Evaluation of teachers should be done at an interval of one (44/96) or five years (35/96) and the method can be by peer review of the lecture of teachers by an expert group or by subjecting the teachers to under graduate questions. And if they secure <50% for one year some miner constraints should be given and if it is repeated for three years major strictures should be taken. Evaluation or assessment of teachers should also be done by students but must be kept confidential. However, besides all the administrative regulations and strictures, the committed genius, research oriented and student loving teachers should be rewarded. It is a pleasure for all of us to know that in 2006, in 8th annual faculty excellence awards program, organized by school of medicine, Virginia, Commonwealth University, five pathology faculty members were rewarded. We congratulate those dedicated educators! This can also be done in India in State and National level.
Suggestions were also invited for better facilities necessary for the faculty. These include financial assistance for National conferences (once every year)/International conference (in every 7 years), CME, books, laptop and children education. Training in foreign universities, adequate infrastructure including hi-tech classrooms were some other suggestions.
The predictor of our efficacy and success are our students. But students differ in their approach to work, study habits and learning styles. It is important to have a deeper cognitive analysis than factual recall. Therefore we can apply different methods to assess their perception, increase their exposure and strengthening academic performances. Keeping this in mind, the questions on students perception and exposure were asked and the revealing facts are.
Today’s learning is motivated mainly by fear of failure and each dominated by note learning and regurgitation in examination and is followed by forgetting. It rather should be motivated by a desire and inquisition for knowledge and students should go for deep or strategic learning and we need a change in assessment of students both in theory/practical Students’ perception can be assessed by asking questions after finishing the lecture or by asking MCQs after each class or each chapter. Suggestions have come for changing the assessment of theory examinations (81.25%) by subjecting the students to short questions and answers or MCQs or clinically driven questions instead of long questions. 79% approved the change in practical examination system also by a continual assessment with frequent oral tests in small groups. Gross specimens should be demonstrated along with photomicrographs in each practical class. This also has been introduced in some centers.
“To study the phenomena of disease without books is to sail an uncharted sea, while to study books without patients is not to go to sea at all.” Therefore increasing exposure is important and as for the pathology teaching it can be done by attending clinic-pathological meetings,
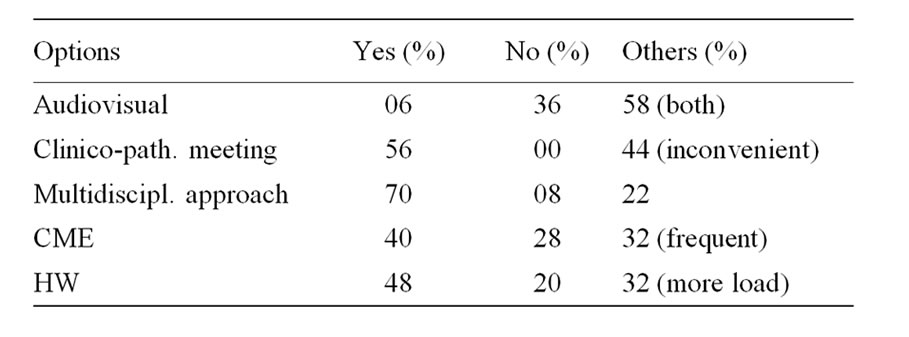
Table 3. Students’ perspective.
combined teaching, conducting CME, etc. The problem can be shortage of time, lack of interest, to plan out the programs. In addition to outside projects, new projects and rewards can encourage the students to initialize research orientation and drag towards a deeper understanding. Again here the problem can be dirth of funds and faculty which can be solved by sincere efforts of government.
The last set of questions were asked to students of 3rd - 5th MBBS which include 300 students in two batches (Table 3). Their answers were revealing and their interaction was an aide to the study. Surprisingly, they prefer black board teaching (36%) to the audio visual mode (6%) of teaching and majority (58%) opted for a combined mode of teaching. The reasons being fastness with power point method, loss of human to human contact (more of a computer to human contact) lack of a classroom atmosphere. So, we suggest to quit that and go for a combined powerpoint with blackboard teaching which can give definitely better results. They also have approved the multidisciplinary approach, regular CME and clinic-pathological meetings.
5. Conclusions
Change in medical education is currently a worldwide phenomenon. So, it is needed to prepare doctors to fulfill the expectations of society, to cope with growth of medical and scientific knowledge and to adjust medical education to changing conditions in the health care delivery system.
The health of people depends on freedom and on education. For this, pathology education holds the key.
REFERENCES
- GMC, “Tomorrow’s Doctors. Recommendations on Undergraduate Medical Curriculum,” General Medical Council, London, 1993.
- I. C. McManus, P. Richards and B. C. Winder, “Clinical Experience of UK Medical Students,” Lancet, Vol. 351, No. 9112, 1998, pp. 802-803. doi:10.1016/S0140-6736(05)78929-7
- S. Lowry, “What’s Wrong with Medical Education in Britain?” British Medical Journal, Vol. 305, No. 6864, 1992, pp. 1277-1280. doi:10.1136/bmj.305.6864.1277
- B. C. Jolly and M. M. MacDonald, “Education for Practice: The Role of Practical Experience in Undergraduate and General Clinical Training,” Medical Education, Vol. 23, No. 2, 1989, pp. 189-195. doi:10.1111/j.1365-2923.1989.tb00885.x
- Medical Colleges in India, 2008. http://www.mciindia.org/
- A. Majumder, U. D’Souza and S. Rahman, “Trends in Medical Education: Challenges and Directions for NeedBased Reforms of Medical Training in South-East Asia,” Indian Journal of Medical Sciences, Vol. 58, No. 9, 2004, pp. 369-380.
- Association of American Medical Colleges, “Physicians for the 21st Century: Report of the Project Panel on the General Professional Education of the Physician and College Preparation for Medicine,” Journal of Medical Education, Vol. 59, 1984, pp. 1-208.
- WHO, “Community-Based Education of Health Personnel: Report of a WHO Study Group,” World Health Organization, Geneva, 1987.
- P. Abeykoon and N. Mattock, “Medical Education in South-East Asia New Delhi: Regional Office for SouthEast Asia,” World Health Organisation, Geneva, 1996.
- S. S. Goudar and P F. Kotur, “Trends in Medical Education,” Indian Journal of Anaesthesia, Vol. 47, No. 1, 2003, pp. 25-29.
- H. E. Khoo, “Implementation of Problem-Based Learning in Asian Medical Schools and Students’ Perceptions of Their Experience,” Medical Education, Vol. 37, No. 5, 2003, pp. 401-409. doi:10.1046/j.1365-2923.2003.01489.x
- M. A. Majumdar, “A Review of the Undergraduate Medical Curriculum,” Bangladesh Medical Journal, Vol. 34, 2002, pp. 47-50.
NOTES
*Corresponding author.

