Open Journal of Anesthesiology
Vol.3 No.3(2013), Article ID:31091,7 pages DOI:10.4236/ojanes.2013.33030
Neural Modulation of Hemiparetic Shoulder Pain by Repetitive Ultrasound-Guided Suprascapularis Nerve Block
![]()
1Rehabilitation Unit, Neuroscience Department Rummo Hospital DEA II Livello, Benevento, Italy; 2Anaesthesiology & IC Unit, Piedimonte Matese Hospital, Piedimonte Matese, Italy.
Email: luigidilorenzo2005@libero.it
Copyright © 2013 Luigi Di Lorenzo, Santopadre Domenico. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received January 24th, 2013; revised March 29th, 2013; accepted April 15th, 2013
Keywords: Shoulder Pain; Nerve Block; Pre Emptive Analgesia; Neurological Rehabilitation; Stroke
ABSTRACT
Background: Neural blockade is widely used in clinical practice to alleviate acute or chronic pain, including pain during rehabilitation. To date there is little controlled evidence to confirm the efficacy of nerve blocks in hemiparetic shoulder pain after stroke. Design: This study is a prospective, open label, cohort trial reporting result from a cohort of stroke patients affected by shoulder pain. Aim: As a cohort study report, in which it is often firstly reported the possibility of an association between an observed effect and a specific environmental based on detailed clinical evaluations and histories, we aim to firstly provide clues in identifying Suprascapularis Nerve blockade as further valuable approach for shoulder pain after stroke. Population: We studied a cohort of patients affected by hemiparetic shoulder pain after Stroke. Methods: Our protocol foresees nerve blocks to be performed each 3 out of 4 days (treatment lasting 30 days) in conjunction with a rehabilitation program with the first aim to provide the window of opportunity to proceed with effective rehabilitation. 47 potential study subjects fulfilled the study criteria and were enrolled. Twenty-four subjects were randomised to the study Group to receive SSNB for the pain of their hemiparetic shoulder while 23 subjects randomized to the control Group whose member did not receive SSNB. They received serial blocks each 3 out of 4 days during rehabilitation. Results: Both treatment reported a reduction in the intensity of their shoulder pain, according to data collected from day 1 through day 42 (6 weeks). Study Group patients, receiving SSNBs, reported significant improvement from entry through the whole follow-up period. The efficiency data were higher for SSNB Group after 2 weeks and again for SSNb group at the end of treatment. Conclusion: Excellent pain relief was achieved in SSNB without clinically relevant complications, these patients having a better improvement on pain during rehabilitation, than the control subjects. Great efficacy has been achieved by combining a nerve block and rehabilitation. About Clinical Rehabilitation Impact, we believe that Suprascapularis nerve blocks can help the stroke survivors maintain an ambulatory or outpatient treatment status, maintain participation in a physical therapy or rehabilitation program, decrease the need for analgesics and in some cases lead to a complete pain relief.
1. Introduction
Hemiplegic shoulder pain is defined as pain perceived in the shoulder and arm after stroke, with a source that does not lie always in the shoulder muscles or joint. Shoulder pain hinders rehabilitation, it is an important contributor to length of hospital stays, and has been associated with depression and decreased quality of life [1]. Several factors have been related to shoulder pain after stroke such as paralysis, restricted range of motion in the shoulderspasticity, right hemispheric cerebrovascular lesion and left hemiplegia, sensory abnormalities, diabetes mellitus and inappropriate handling of the patient [1]. Recovery from shoulder pain may occur in up to 80% [1].
Several approaches for the treatment of hemiparetic shoulder pain have been attempted, but they have had no definitive effects on relieving symptoms. Patients are typically treated with psychotropic drugs, such as amitriptyline, or nonsteroidal anti-inflammatory drugs (NSAIDs) in an attempt to relieve the pain and possibly to improve their mood, sleep and collaboration during physiotherapy [1,2]. A number of studies have suggested that the ideal management of the syndrome be mainly based upon prevention [3-5]. For prophylaxis to be effective it must begin immediately after a stroke and, during early physiotherapy, the multidisciplinary team, patients, and caregivers should be instructed to avoid injuries to the affected limb. Stroke survivors usually suffer for nociceptive hemiparetic shoulder pain: when the central pain is excluded, the pain is assumed to be coming from the joint, with the whole soft tissues stretched from the weight of the parethic arm. The C-fiber mediated effect perceived as pain represents the nociceptive pain most often affecting the shoulder and is reported to be in a significant number of stroke survivors [3-5]. It is often related to change dynamics due to paresis or weakness on the affected side [3]. Early severe pain treatment is advocated, because the earlier is pain treatment, the better is the pain outcome [6]. Neural blockades including suprascapularis nerve blocks, widely used in clinical practice to alleviate acute or chronic pain during rehabilitation programs, may provide temporary relief of pain that is not usually sustained [7]. Neural blockade comprises a diverse group of procedures that are often used to treat pain in clinical practice. In general, these have been advocated to alleviate acute pain or an exacerbation of chronic pain, and to provide direct and localized therapeutic action, especially in patients in whom pain is accompanied by swelling and inflammation [7]. Therapeutic nerve blocks can help the patient maintain an ambulatory or outpatient treatment status, maintain participation in a physical therapy or rehabilitation program, decrease the need for analgesics and, in some cases, avoid or delay surgical intervention [7]. Sensory blocks can also be used to “reset” the pain generators, especially in cases of sympathetic mediated pain disorders with serial injections [8,9]. Once a response to painful stimuli is attenuated, the patients can participate in a therapy program that emphasizes functional tasks, joint range of motion, stretching, and skin desensitization. In order to ensure a persistent pain relief, more accurate localizations of the specific nerves to block should be guaranteed. At our institutions, nerve stimulator-guided blocks have facilitated successful blocks for anaesthetic and analgesic purposes but sometimes, during rehabilitation, we use to perform blocks with ultrasound guidance only In a previous experience we saw as suprascapular nerve blocks had successfully facilitate rehabilitation programs [10]. However, despite widespread use of suprascapularis nerve block in clinical practice, to date there is no controlled evidence to confirm the efficacy of this nerve block for shoulder pain after Stroke. Given this recent evidence supporting a strong-weak opioid combination, a prospective open-label study was initiated with the aim of evaluating the possible advantages due to effects of the nerve block from pain relief due to analgesic medication and/or therapeutic exercises. After a first uncontrolled and unpublished prospective case-series study anedoctally confirming us the suitability, in day-to-day clinical practice, of repetitive nerve ultrasound-guided suprascapular nerve blocks for hemiparetic shoulder pain after stroke, we decide to perform this trial.
2. Method
Setting and study design. The settings of the study were the rehabilitation unit and Day Hospital providing rehabilitation services for inpatients and outpatients. The study was a prospective, open label, cohort trial. The goal was to recruit at least about 80 subjects so that there would be about 40 subjects in each treatment group. Random allocation sequences were not previously planned, but a simple dichotomisation was obtained during follow-up. Namely, we choose to treat with or without nerve blocks according physician feelings about several variables: patients willing, compliance with pharmacotherapy, ongoing physical therapy (e.g. Laser Therapy, Electric Nerve Stimulation, etc.), number of drugs needed, side effects already claimed, comorbidity (e.g. mild renal failure) and acceptance of nerve blocks. We so obtained two groups of patients treated with rehabilitation and pain killers (BDZ, triciclics, coadiuvant analgesics, opioids, etc.) or rehabilitation plus nerve blocks. The only common limitation was to avoid chronic use of NAIDSs except for acute pain due to a clear biomechanical breakthrough pain (e.g. patients needing to walk for a long while being aware that this could cause worse pain for that while). Patients were excluded from the study if they had received regular treatment with a strong opioid, recent long lasting NAISD therapy or had already received ipsilateral shoulder surgery during last weeks before the study. Screened patients satisfying the selection criteria each gave written informed consent before inclusion in this open prospective trial. Our institutional review board approved the study protocol and all patients provided written informed consent before enrolment. Moreover, this prospective study was carried out in accordance with the latest revision of the Declaration of Helsinki and Good Clinical Practice. Assessment included the biomedical and functional implication of each symptom. A carefully planned history taking and a clinical examination were performed by physicians knowledgeable in neurology, rehabilitation medicine and treatment of musculoskeletal pain in order to avoid delaying the diagnosis. Patient histories are usually critical in the differentiation between traumatic muscular lesions and tears, cervical neuropathic pain or secondary conditions after stroke (i.e. spasticity, discomfort, etc.). As these conditions are associated with similar clinical findings, including pain and weakness with attempted sitting position or walking, radiological imaging were obtained and were carefully scrutinised to determine if there is an underlying pathological process. A full work-up, including a carefully shoulder X-ray and an ultrasound study of rotator cuff muscle and shoulder girdle were necessary to differentiate the nature of the pain in all cases. To complete the assessment, the emotional state of the patient and an understanding of the effect of the disabilities in the context of the patient’s normal environment are needed. For this purpose, in our clinical practise we routinely administer anxiety and depression scale and a neuropsicological assessment after stroke. The result in this study was used to exclude the positive subjects from the eligible ones.
Subjects. For these study we accepted patients having a diagnosis of Stroke but no other neuropathies (e.g. G. Barrè) causing profound physical impairment. They are all patients admitted at our hospitals and diagnosed with Hemiparetic Shoulder Pain (HSP) based on all of the following inclusion criteria: 1) diagnosis of stroke, based on clinical examination and a computerised tomography (CT scan) within the first week after onset of symptoms. Patients’ selection was based on I.C.D.-10 classification [infarct cerebri (433) and NOT hemorragia cerebri (431); 2) nociceptive pain at hemiparetic shoulder defined as pain on moving (or try to move) the arm and/or pain at rest and 3) refractory hemiparetic shoulder pain syndrome treated with pain killers and physiotherapy only. Patients were not considered if they had history of adhesive capsulitis (limited or painful passive mobility of the shoulder), biceps tendonitis, previous rotator cuff tears or surgery, allergy or intolerance of any of the drugs used in the study, or if they were receiving long lasting steroids treatment. Patients received Suprascapular Nerve Blocks injecting 10 ml of bupivacaine delivered with a 21 G, length 40 mm, intramuscular needle, under ultrasound guidance. Our protocol foresees nerve blocks to be performed each 3 out of 4 days (treatment lasting 30 days) in conjunction with a rehabilitation program with the first aim to provide the window of opportunity to proceed with effective rehabilitation. Main outcome measure was always shoulder pain measured according a Visual Analogic Scale (V.A.S.) based on subjective pain answers with a score range of 0 - 10. Patients were asked to record the pain scores, eventual analgesics needed per day during rehabilitation and they were usually revaluated daily. A self-made questionnaire assessing the patient’s satisfaction about quality of sleep was given the last day of treatment. Nerve block’s were performed only on the base of clinical evaluations, beyond this study’ necessities. Patients being assisted for completely loosed autonomy in ADL (Activities of Daily Living) were not accepted, though patients with using of canes or devises were. No limit was placed on the time since starting of pain, though in our anectodal experience early onset with diagnosis of sub-acute pain does not discourage nerve blocks use as first line approach. Different outcomes, occurrence rate of side effects and different painkillers required to achieve a good pain relief were reported. Inconsistent responses were defined as full pain relief after few days or effectiveness pain relief of less then 10%; acceple outcomes were defined as pain relief effectiveness of more than 50% within at least 2 - 3 weeks.
3. Pain Assessment and Analysis
Pain was assessed using a 10 cm V.A.S. with the left end marked “0” and “No Pain” and the right end as “10” and “Severe Pain”. As suggested elsewhere [11], the parameter treatment effectiveness was used as a measure of residual disability. Effectiveness at discharge reflects the proportion of potential improvement achieved during hospitalisation. The proportion was calculated according to the following formula: (discharge scale score-initial Scale score)/(maximum scale score-initial Scale score) × 100. According to the formula, the effectiveness was 100% when a patient achieved the maximum scale score [11]. We also calculated the rate of pain improvement per days (average daily improvement in duration of rehabilitation treatment: efficiency, which was calculated as follows: efficiency = (discharge score-initial score)/(days of treatment) of V.A.S. score [11].
4. Analgesic Consumption
Albeit this study was not designed to differentiate effects of the nerve block from pain relief due to analgesic medication, patients were asked to record the quantity of analgesics needed per day during the study period and try to avoid rescue doses. During rehabilitation patients with a VAS < 4 were allowed paracetamol 500 mg with a maximum of 6 lets per 24 hours. Patients with a VAS > 4 were allowed either paracetamol or tramadol 100/200 mg once day let. After the first block, all drugs were suspended apart from one paracetamol 1000 mg let that was the unique daily rescuedose.
5. Suprascapularis Nerve Block
5.1. Anatomy
Arm blocks require meticulous technique and can be challenging to those unfamiliar with the regional anatomy. The suprascapular Nerve originates from the superior trunk of the brachial plexus and contains fibers from the fifth and sixth cervical roots. It enters the supraspionus fossa below the transverse scapular ligament after passing obliquely deep to the trapezius and omohyoid muscles (Figure 1). The nerve innervates the supraspinatus muscle and gives branches to the glenohumeral and acromioclavicular joints as well as the conoid, trapezoid,
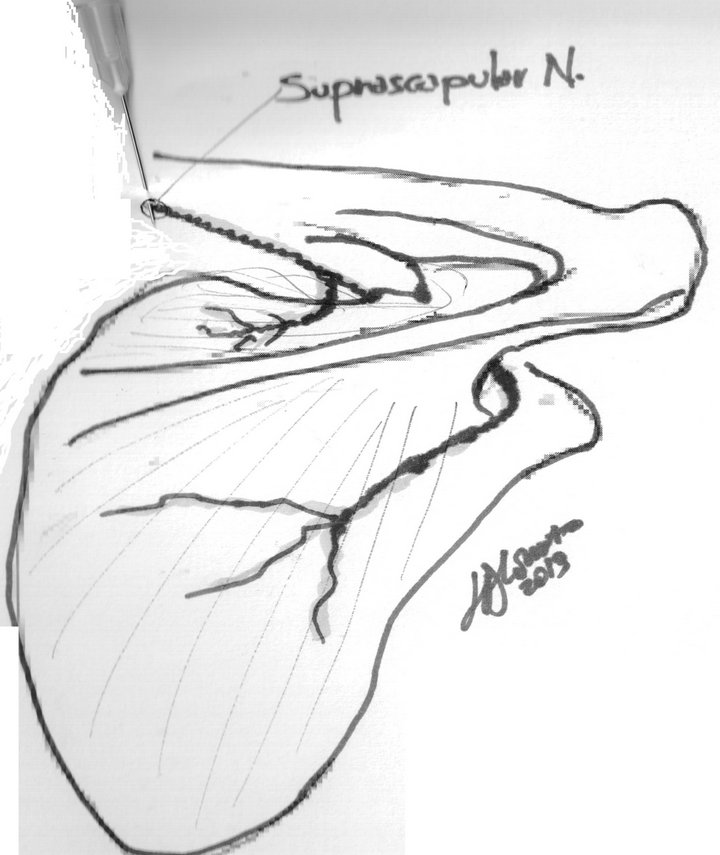
Figure 1. The suprascapular nerve arises from the upper trunk (formed by the union of the fifth and sixth cervical nerves). It innervates the supraspinatus and infraspinatus muscle. It runs lateral beneath the trapezius and the omohioideus and enters the supraspinatous fossa through the suprascapular notch, below the superior transverse scapular ligament; it then passes beneath the supraspinatus and curves around the lateral border of the spine of the infrasinatous fossa. In the supraspinatous fossa it gives off two branches to the Supraspinatus muscle, and an articular filament to the shoulder joint; and in the infraspinatous fossa it gives off two branches to the infraspinatous muscle, besides some filaments to the shoulder joint and scapula.
and coracoacromial ligaments. The nerve passes around the spinoglenoid notch to terminate in the infraspinatus muscle. It also carries sympathetic innervation to the joint capsule.
5.2. Ultrasound Anatomy
Supraspinous notches is usually studied by means ofoblique coronal images obtained medial to the acromion revealing the supraspinous notch as a shallow groove located in the cranial aspect of the scapula just medial to the bony glenoid. The suprascapular nerve is appreciated in the supraspinous notch, deep to the supraspinatus muscle, as tiny hypoechoic dots beside the suprascapular artery.
6. Block Technique
The nerve is the pathway of somatic pain from the shoulder and acromioclavicular joints and structures surrounding them. The block does not result in any skin analgesiabut when successful, relieves pain in the shoulder joint. The S.S. nerve block had been well described since several decades [12] and Granirer firstly described a posterior approach [13,14]. Our procedures are usually performed under ultrasound guidance but to refine our technique and reduce the risk of pneumothorax we followed the indirect S.S.N.B. method described by Dahan et al. [14].
The patient should be sitting with arms to the sides and head and shoulders slightly flexed. With a skin pencil the spine of the scapula is lined in: the inferior scapular angle is located and bisected by a line which crosses the first line. A weal is raised one finger-breadth from the crossing, in the upper outer angle, and a needle inserted downwards and medially to make contact with the bone of the supraspinatus fossa, just lateral to the notch. Needle is then withdrawn and reintroduced more medially until its point lies in the notch. Paraesthesia, if provoked, takes the form of pain at the tip of the shoulder and after aspiration 10 ml of analgesic solution can be injected. The block must be at the Suprascapular notch as there the nerve is accessible to a needle and no afferent branches leave it before it passes through the notch. The ultrasound guided injection of 10 cc of local anaesthetic into the supraspinous fossa results in completely filling the supraspinous muscle fossa, which then contains the anaesthetic within its fascia [15]. The suprascapular nerve then gets bathed in local anaesthetic as it enters the fossa resulting in an effective nerve block [12,14].
7. Results
After a couple of monitored physiotherapy weeks, 47 potential study subjects fulfilled the study criteria and were enrolled. They all continued the indicated rehabilitation therapy which included ongoing shoulder training. All the patients were taking daily medication at the beginning of the study and continued that therapy with no change in dosages for its duration. At the time of enrolment, the study participants were randomised in two comparison groups: twenty-four subjects randomised to study Group to receive S.S.N.B. for the pain of their hemiparetic shoulder while 23 subjects randomized to the control Group whose member did not received S.S.N.B. As shown in Table 1, the two randomization groups were statistically comparable with regard to demographic variables and pain scores post-CVA. Pain from the shoulder and its surrounding tendons was often felt anterolaterally and at the insertion of deltoid and rotator cuff muscle: sometimes it radiated down the arm on the triceps muscle and less frequently down the other shoulder muscle. The rotator cuff is a sheet of conjoint tendons closely applied over the shoulder capsule and inserting into greater tuberosity of the humerus. It is composed of subscapularis in front, supraspinatus above and infraspi-
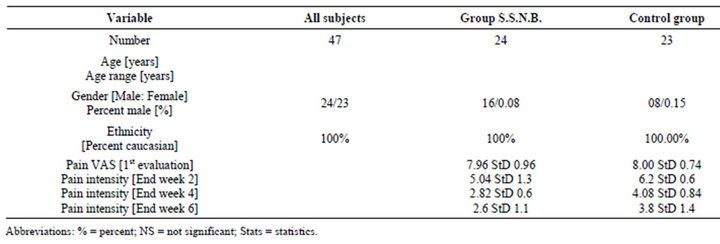
Table 1. Demographics of study subjects.
natus and teres minor behind: the “rotator muscle” which has an important function in silizing the head of the humerus by pulling it firmly into glenoid when the deltoid lifts the arm forwards or sideways. In our subjects, pain on the top of the shoulder suggested a sort of gravitational dysfunction. The entire haemiparetic shoulder was stretched down by its own weight and the top muscles frequently become site of referred pain and trigger points. Both treatments reported a reduction in the intensity of their shoulder pain, according to data collected from day 1 through day 42 (6 weeks) (Tables 1 and 2). Study Group patients, receiving S.S.N.B.s, reported significant improvement from entry through the whole follow-up period. The efficiency data were higher for S.S.N.B. Group after 2 weeks (S.S.N.B. Group = 0.21 for 14 days; Control Group = 0.12 for 14 days) and again for S.S.N.B. group at the end of treatment (S.S.N.B. Group = 0.13 for 42 days; Control Group = 0.9 for 42 days, Table 2). Good pain relief was achieved in S.S.N.B. without clinically relevant complications (PainVas effectiveness = 67.5 StS13.4, Table 2), these patients having a better improvement on pain during rehabilitation, than the control subjects (PainVas effectiveness = 51.29 percent, Table 2). Analysis of the variance (ANOVA) of PainVas effectiveness, PainVas end of Treatment and Questionnaire data was made between the two groups, where S.S.N.B. Group also reported having less severe pain during sleep and during physiotherapy associated with a more restful sleep than the control subjects (Table 3). Adverse effects from the S.S.N.B. procedure were infrequent and generally benign. During the injection phase in sitting position, some patients experienced soreness and in a few cases we also observed local or regional cutaneous vasodilatation, piloerection and sweating consistent with strong regional sympathetic responses to the soft tissue needling.
8. Discussion
Anaesthetic blocks provide temporary relief of pain that are not usually sustained during time. When we perform
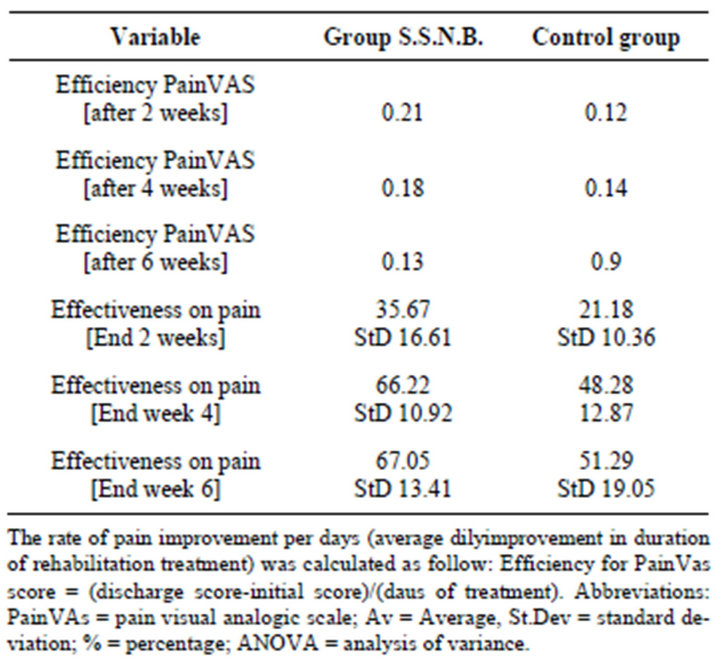
Table 2. Reducion in pain severità with treatments as evidenced by efficiency and effectiveness for the variable PainVas.
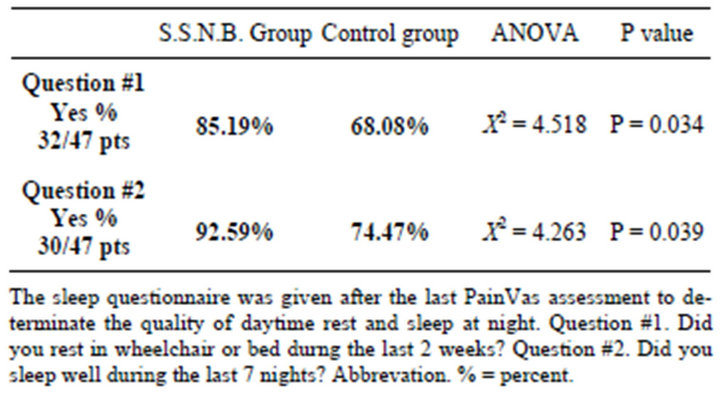
Table 3. Results from the sleep questionnaire.
a blockade Local Anaesthetics (LA) produce an impulse conduction block that is painless and completely reversible, the nerve block dissipates spontaneously with time, as the drug is released from its bond with the sodium channel receptors. The transitory neural quiescence provided by local anaesthetic block, repeated at intervals, is often sufficient to gradually wind down the activity of spontaneously discharging hyperactive neurons, thereby relieving pain effectively beyond the few hours’ duration of the drugs’ blocking action [7]. The Suprascapularis nerve supplies the supraspinatus muscle and provides articular branches to the glenohumeral and acromioclavicular joints but it also supplies sensory and sympathetic fibres to two-thirds of the shoulder capsule. Nerve blockade can therefore reduce an eventual “crosstalk” eventually occurring between descending involved sympathetic nerves and ascending sensory nerves. This because we know that increases in sympathetic nervous system activity result in an increase in pain, known as sympathetically mediated pain [7]. Reducing the sympathetic nerve activity in the painful shoulder by blocking nerve with a series of local nerve blocks can break the cycle of sympathetically mediated pain and provide relief. More prolonged neural blockade could also be performed using continuous perineural infusion of LA. This study does not aim to differentiate effects of the nerve block from pain relief due to analgesic medication and/or therapeutic exercises but reports the suiility of such blocks in day to day clinical practice. After several numerous blocks performed in conjunction with a rehabilitation program for various shoulder pains, anecdotal experiences suggests us that nerve blocks can provide pain relief beyond the period of local anaesthesia. Unfortunately original published accounts of the incidence, duration, and degree of prolonged pain relief are scarce. Further study was deemed necessary to evaluate the duration and mechanism of action of nerve blocks. A comparative controlled study of the analgesic values of nerve blocks was carried out by our Unit [10] for shoulder pain after rotator cuff tendonitis and it was observed that nerve blocks were effective since the first days of rehabilitation and lasting for a sufficient period. It was concluded that the blocks provides more effective and longer lasting pain relief than rehab alone. In our Stroke patients, the specific aim was also to try to reverse super-sensitivity from traducing into chronic pain and therefore to prevent the chronic shoulder pain in hemiparetic arm after stroke. Moreover, advocates of this approach explain these effects on the basis of the fact that anaesthetic nerve blocks, performed in conjunction with a rehabilitation program, can provide the window of opportunity to proceed with effective rehabilitation. The action of the block provides prompt analgesia and pain relief but above all acts preventing chronic pain between different ways: avoiding a persistent “noxa patogena” does not permit pathological biomechanical adaptations (e.g. raising up of humeral head during gleno humeral joints movements) and it is postulate to reduce the “wind up effect” leading to chronic pain.
9. Conclusion
The results of this report suggest that neural modulation by repetitive nerve blocks may help to alleviate refractory hemiparetic shoulder pain and it could be an attractive treatment offering clear advantages. Current evidence was scarse but given the high prevalence of shoulder pain in stroke survivors and their contraindications, the potential adverse effects of some treatments (i.e., oral anti-inflammatory drugs) and the invasive nature of other treatments (i.e., joint infiltrations), we believe we should need studies of higher methodological quality. Thus, it would be advantageous to carry out prospective, double blinded-controlled clinical trials to confirm the efficacy of suprascapularis nerve blocks integrated in a wellplanned rehabilitation program. In stroke patients with chronic pain conditions, a multifaceted approach (treatment that includes rehabilitation, pain management and psychological intervention) still remains essential.
REFERENCES
- I. Lindgren, A. C. Jönsson, B. Norrving and A. Lindgren, “Shoulder Pain after Stroke,” A Prospective PopulationBased Study Stroke, Vol. 38, 2007, pp. 343-348.
- L. Bender and K. McKenna, “Haemiplegic Shoulder Pain: Defining the Problem and Its Management,” Disability & Rehabilitation, Vol. 23, No. 16, 2001, pp. 698-705. doi:10.1080/09638280110062149
- C. M. Dean, F. H. Mackey and P. Katrak, “Examination of Shoulder Positioning after Stroke: A Randomised Controlled Pilot Trial,” Australian Journal of Physiotherapy, Vol. 46, No. 1, 2000, pp. 35-40.
- M. Widar, L. Samuelssonn, S. Karlsson-Tivenius and G. Ahlstrom, “Long-Term Pain Condition after a Stroke,” Journal of Rehabilitation Medicine, Vol. 34, 2002, pp. 165-170. doi:10.1080/16501970213237
- K. Walsh, “Management of Shoulder Pain in Patients with Stroke,” Postgraduate Medical Journal, Vol. 77, No. 912, 2001, pp. 645-649. doi:10.1136/pmj.77.912.645
- D. Le Bars and J. C. Willer, “Physiology of Pain. Enciclopedié Medico Chirurgicale. I-36-020-A10. Anaesthesia,” 2005.
- G. Varrassi, A. Paladini, F. Marinangeli and R. Gabor, “Neural Modulation by Block and Infusion,” Pain Practice, Vol. 6, No. 1, 2006, pp. 34-38. doi:10.1111/j.1533-2500.2006.00056.x
- C. C. Gunn, “Neuropathic Pain: A New Theory of Chronic Pain of Intrinsic Origin,” Annals of Royal College Physical Surgery of Canada, Vol. 22, 1989, pp. 327-330.
- D. L. Brown, “Somatic or Sympathetic Block for Reflex Sympathetic Dystrophy. Which Is Indicated?” Hand Clinics, Vol. 13, No. 13, 1997, pp. 485-497.
- L. DiLorenzo, M. Pappagallo, R. Gimigliano, et al., “Pain Relief in Early Rehabilitation of Rotator Cuff Tendinitis: Any Role for Indirect Suprascapularis Nerve Block?” Europa Medicophysics, Vol. 42, No. 3, 2006, pp. 195-204.
- S. Shah, F. Vanclay and B. Cooper, “Efficiency, Effectiveness and Duration of Stroke Rehabilitation,” Stroke, Vol. 21, 1990, pp. 241-246. doi:10.1161/01.STR.21.2.241
- M. R. Wassef, “Suprascapular Nerve Block. A New Approach for the Management of Frozen Shoulder,” Anaesthesia, Vol. 47, No. 47, 1992, pp. 120-124. doi:10.1111/j.1365-2044.1992.tb02007.x
- H. M. Werteheim and E. A. Rovenstine, “Suprascapular Nerve Block,” Anesthesiology, Vol. 2, No. 2, 1941, pp. 541-545. doi:10.1097/00000542-194109000-00006
- D. Thw, et al., “Indirect Suprascapular Nerve Block Tecnique.” http//.epf.planet.qc.ca/drdahan on May 2004
- G. C. Feigl, F. Anderhuber, C. Dorn, W. Pipam, M. Rosmarin and R. Likar, “Regional Anesthesia and Pain Medicine,” The Long Journey of Epidural Steroid Injections, Vol. 32, No. 6, 2007, pp. 488-494.

