Open Journal of Molecular and Integrative Physiology
Vol. 2 No. 2 (2012) , Article ID: 19378 , 6 pages DOI:10.4236/ojmip.2012.22007
Dose-dependent effect of parathyroid hormone 1-34 fragment and its influence mechanism on the functional activity of isolated heart
![]()
1Department of Physiology, Yerevan State Medical University after M. Heratsi, Yerevan, Armenia
2Laboratory of Integrative Biology, Physiology Institute after L. A. Orbeli of RA NAS, Yerevan, Armenia
Email: annasmark@yahoo.com
Received 16 March 2012; revised 11 April 2012; accepted 5 May 2012
Keywords: 1-34 Parathyroid Hormone; Isolated Heart; Calcium; cAMP
ABSTRACT
The present investigation is the continuation of our prior clinical studies on the content of parathyroid hormone (PTH), its paracrine analog, parathyroid hormone-related protein (PTHrP) and electrolytes in blood of patients with heart failure. The results of these studies formed the basis for the nomination of the hypothesis on PTH and PTHrP compensatorymodulating effect on the contractile activity of heart. The objective of this study is to elucidate the mechanism of the compensatory-modulating effect of PTH on heart functional activity, which is realized by the study of effective doses of PTH by pharmacological analysis, using different inhibitors. The dose-dependent effect of PTH on the heart contraction rate and amplitude is studied on the frog isolated heart by the method of non-invasive registration of heart contractile activity. The method is based on the photoelectric principle of the reflected from the contractile object light ray transformation into an electric signaling. It is shown that the most effective dose that has positive chronotropic and inotropic effects on heart is 10–10 M hormone. To clarify the mechanism of PTH physiological dose action on the contractile activity of heart PTH 1-34 is combined with Ca-channel as well as phosphodiesterase blockers. The mentioned substances are applied based on the fact that PTH effect on target cells is mediated by secondary messengers, particularly calcium ions and cAMP. Based on the data obtained by combination of hormone with Verapamil (10–5 M) and Theophylline (10–4 M), we concluded on the involvement of calcium ions in the realization of chronotropic and cAMP in the inotropic effects on the heart.
1. INTRODUCTION
In recent years, particular attention is paid to the role of calcium-regulating system of the organism (parathyroid hormone (PTH), calcitonin, parathyroid hormone-related peptide (PTHrP)) in the mechanism of pacemaker manifestation and heart contractile activity [1], blood pressure regulation [2-7], renal system functioning [8], proliferation and functioning of different structures [9], in particular, the beta cells of pancreas [10] and placental trophoblast [11], as well as the development of bone tissue, etc. [12]. It is also known that pPTHrP is secreted by malignizing cells [13] and myocardial ischemized cells [14], obviously being a modulating factor in the growth and functioning of the mentioned structures. In our earlier work we demonstrated that PTH is a modulator of neuron functional activity and has “early” and “late” effects [15]. It was revealed that “early” effect of the hormone is conditioned by its direct action on the calcium conductance of membrane, and the “late” one—its influence on the metabolism-dependent component, during which the activation of phosphoinositide path occupies the central place, with the involvement of diacilglycerol (DAG) and inositol triphosphate (IP3) in the realization of hormone signal [16]. The stimulating effect of hormone on synaptic transmission is also shown [17].
Our previous clinical studies [18] revealed that the content of PTH and PTHrP increases in blood of patients with heart failure dependent on the severity of pathology. Comparing the obtained results with the literature data [14,19,20] it was assumed that PTH and PTHrP have compensatory-modulating significance in order to preserve cardiac function. A number of studies [5,7,21] indicate involvement of the major calcium-regulating factor, PTH in the regulation of heart contractile activity. Despite the research results multiplicity, some aspects of calcium-regulating system effects on the maintenance of calcium homeostasis in heart and its activity, as well as the mechanisms of its impact and influence of different fragments of hormones on the cellular level are poorly studied.
The objective of this study is to elucidate the mechanism of the compensatory-modulating effect of PTH on heart functional activity, which is realized by the study of effective doses of PTH by pharmacological analysis, using different inhibitors.
This study aims to identify the most active doses of the 1-34 fragment of parathyroid hormone and to study the mechanism of its action on pacemaker and contractile activity of isolated frog heart. The research was conducted in two stages. In the first one the impact of concentrations of 10–7 M, 10–8 M, 10–9 M, 10–10 M, 10–11 M on the functional activity of the frog isolated heart was studied in vitro. In the second stage we studied the main mechanisms, among them the messenger system involved in hormone action on the functional activity of heart by combining active concentration of the 1-34 PTH with calcium channel and phosphodiesterase blockers from the point of view of pharmacological analysis. The mentioned study is an attempt to shed more light on the involvement of calcium-regulating PTH into the compensatory-regulatory mechanism, directed to maintain the heart activity.
2. MATERIAL AND METHODS
Studies were performed on the isolated heart of frog, which was placed in a special chamber containing a nutrient Ringer solution (NaCl-0.65%, KCl-0.018%, CaCl2 -0.02%, NaH2PO4-0.01%, Na2HPO4-0.03%, pH = 7.4) with different concentrations of 1-34 PTH, and in combination with the blocker in the incubation medium. The application of the method of “isolated organs” has many advantages compared to in situ experiments, as it excludes nervous and humoral effects and enables to carry out long-term investigations by accurately changing the composition of incubation medium (certain concentration of hormones, ionic channel blockers, activators etc.). Heart contractions were recorded by the non-invasive method using a device that works on a photoelectric principle. Energetically stable light stream from the lighting source, passing through the condenser of the microscope and the isolated heart, was modulated with the frequency of its contractions. Modulated radiation passing through the microscope optics, diaphragm and projecting on the photocathode of the photoelectric multiplier resulted in a proportional change in the anodic current, which in turn was amplified by the amplifier. The signal from the amplifier output entered to the oscillograph and computer entry.
The first series of experiments were carried out by using different concentrations 10–7 M, 10–8 M, 10–9 M, 10–10 M, 10–11 M of the 1-34 fragment PTH (“Sigma”), the rate and amplitude of heart contractions were recorded. After revealing the most active, but at the same time, physiological doses of the hormone, the second series of experiments were carried out, which allowed to reveal the mechanism of PTH influence on the functional activity of the heart by hormone combination with calcium channel blocker (Verapamil, 10–5 M, “Sigma”) and phosphodiesterase (Theophylline, 10–4 M, “Sigma”). The obtained results were processed statistically by computer software package Origin-70. Each curve, reflecting dynamics of changes in the heart contraction amplitude or rate, was presented as a mean curve from 10 - 12 experimental data.
3. RESULTS AND DISCUSSION
The revealed results of the first experiment series (Figures 1(a)-(f) and 2(a)-(f)) allowed to conclude that the 1-34 fragment PTH in dynamics reliably affects the rate and amplitude of heart contractions. Change in heart rate observed under the influence of concentrations 10–7 M, 10–8 M, 10–9 M of 1-34 PTH was more expressed, however, had a wavy character, accompanied by arrhythmia, which is incompatible with a normal heart rhythm. At the same time, the mentioned hormone concentrations do not correspond to the physiological norm therefore the indicated concentrations of hormone were not used in the second series of experiments.
The most effective and closest to the physiological norm are the concentrations of the hormone 10–10 M and 10–11 M. For example, the concentration of the hormone 10–10 M increased the pacemaker rhythm of the heart, whereas in control, with the introduction of physiological saline in a similar dose, the pacemaker heart rate decreased and after the first 15 minutes was 85% of the initial value (Figures 2(a) and (e)). Similarly, in the physiological saline the amplitude of heart contractions rapidly decreased and after 20 minutes was 80% of the initial value, but the effective concentrations of the 1-34 PTH not only kept up the amplitude of heart rate for a long time, but also increased in comparison with the control by 20% - 30% (Figures 1(a) and (e)). It is assumed that PTH and, in particular, its active fragment 1-34, which regulates calcium homeostasis in blood, not only promotes activation of pacemaker heart cells, but also modulates calcium entry into cardiomyocytes, thus regulating the strength of heart contractions. It is not excluded that the increase in pumping capacity of the heart is also associated with activation of the output of calcium from intracellular depots by IP3, which formation is enhanced via parathyroid hormone [22].
To clarify the mechanism of PTH physiological dose action on the contractile activity of heart 10–10 M PTH
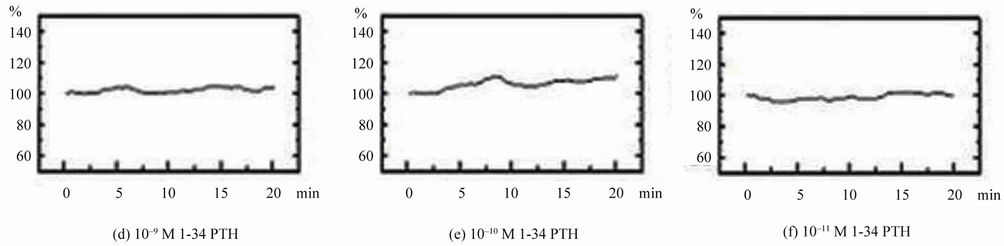
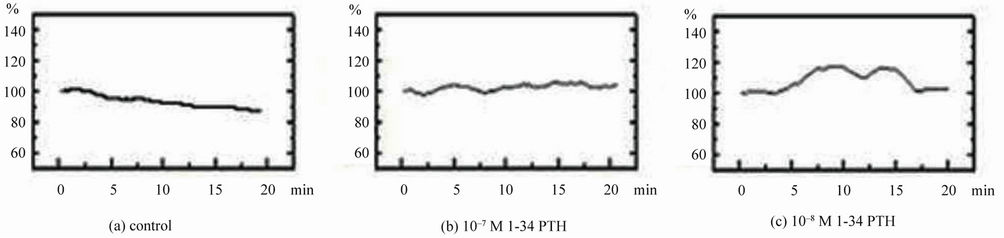
Figure 1. Changes in the amplitude of contractions of frog isolated heart under the influence of different doses of the 1-34 fragment PTH. The amplitude (in percentage) of contractions is denoted on the ordinate; time (in minutes, duration of experiment) is denoted on the abscissa.
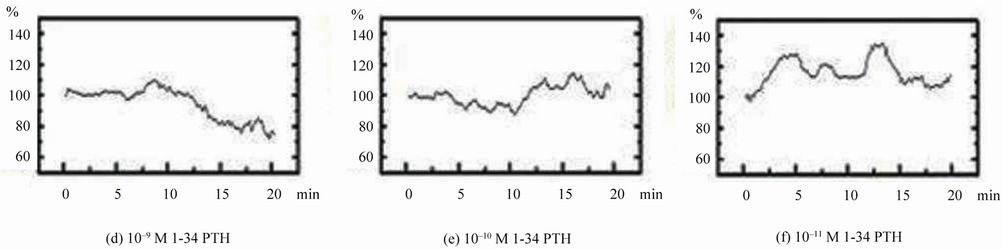
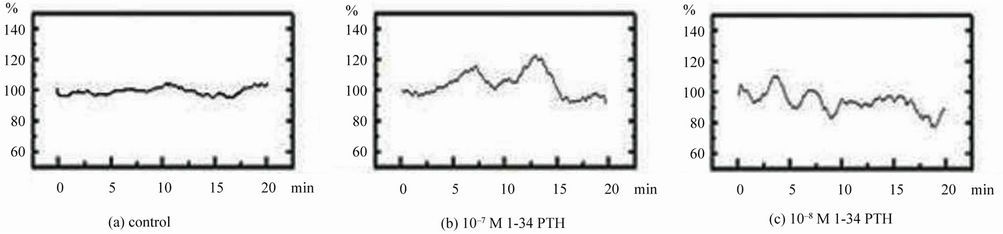
Figure 2. Dynamics of frog isolated heart contractions rate changes under the influence of different doses of the 1-34 fragment PTH. The rate (in percentage) of contractions is denoted on the ordinate; time (in minutes, duration of experiment) is denoted on abscissa.
1-34 is combined with Ca-channel as well as phosphodiesterase blockers. The mentioned substances are applied based on the fact that PTH effect on target cells is mediated by secondary messengers, particularly calcium ions and cAMP. In case of combined effect of 10–10 M PTH 1-34 with calcium channel blocker Verapamil 10–5 M, the action of hormone on pacemaker activity was not revealed (Figure 3(b)). The heart rate decreased reliably and after 17 minutes was 70% from the initial level. Leveling of PTH effect on heart rate by Verapamil assumes that in the given mechanism calcium channels are involved and thereby blockade of these channels leads to a decrease in the frequency of pacemaker discharges. These data are in line with the literature data, illustrated the essential role of ionized calcium and its channels in the functional activity of heart, particularly, in the synchronized cellular depolarization, pacemaker activity and subsequent activation of contractile proteins, i.e. in the cardiac excitation-contraction coupling [1-3,6].
Concerning to the amplitude of heart contractions, it was found that this index did not undergo significant changes, as an independent influence of the hormone on the strength of cardiac output was not blocked by Verapamil (Figure 3(a)). The amplitude of heart rate was kept up for a long time at a rather high level and correlated with the analogous parameter, which was observed in self-action of the hormone (Figure 1(e)).
In case of combination of PTH 1-34 fragment with Theophylline 10–4 M in the incubation medium additional reliable effect on the amplitude of heart response was not observed, while the rate increased (Figures 4(a), 1(e) and 4(b), 2(e)), in comparison with the single hormone effect. This suggests cAMP participation, as a secondary messenger in the mechanism of PTH effect realization on the heart contractile function. According to the obtained results, it was assumed that PTH supporting effect on the amplitude of heart contractions was mostly determined by cAMP-dependent mechanism, which is supported by the data, demonstrated an important role of cAMP in regulation cardiac muscle contraction. Increased intracellular concentration of cAMP by inhibition of phosphodiestherase, through its coupling with other intracellular messengers, increases heart contractility (inotropy) [23].
Thus, comparing the obtained results with the data of our previous studies [18], as well as with the latest published findings [24-26], we can assume that the increase of PTH levels in blood of patients suffering from heart failure has a compensatory modulating significance for supporting heart activity.
4. CONCLUSIONS
The analysis of obtained data demonstrates the possible involvement of physiological doses of PTH 1-34 fragment into heart function regulatory mechanism. It is shown that the most effective dose that has positive chronotropic and inotropic effects on heart is 10–10 M. The pharmacological analysis was performed to study the indicated effects. Based on the results of simultaneous action of 10–10 M 1-34-PTH with calcium channel
 (a) (b)
(a) (b)
Figure 3. Combined action of the 10–10 M 1-34 fragment PTH and 10–5 M Verapamil on amplitude (a) and rate (b) of contractions of frog isolated heart. The amplitude and rate (in percentage) of contractions is denoted on the ordinate; time (in minutes, duration of experiment) is denoted on abscissa.
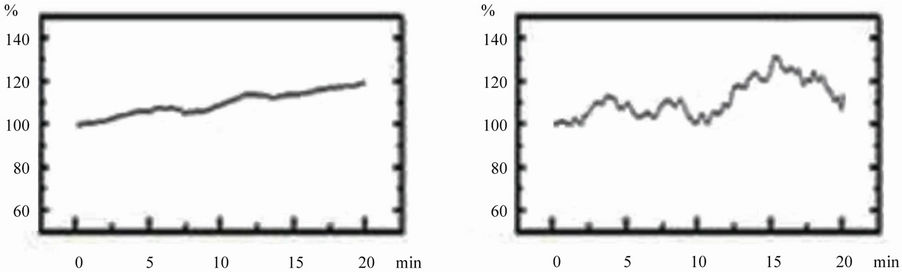 (a) (b)
(a) (b)
Figure 4. Combined action of the 10–10 M 1-34 fragment PTH and Theophylline 10–4 M on amplitude (a) and rate (b) of contractions of frog isolated heart. The amplitude and rate (in percentage) of contractions is denoted on the ordinate; time (in minutes, duration of experiment) is denoted on abscissa.
blocker Verapamil (10–5 M), which mitigated the effect of PTH on heart pacemaker activity, the assumption of calcium dependent mechanism of positive chronotropic action of PTH is put forward. Combined action of PTH with phosphodiesterase inhibitor Theophylline (10–4 M), which increases the concentration of cAMP, does not associated with an additional impact on heart contraction amplitude and it remains on the level of PTH self-action. Taking into account these results along with literature data [23] about activation of heart contractile activity by this secondary messenger, one can conclude that PTH maintains heart contraction amplitude via cAMP. The obtained data support our hypothesis about PTH compensatory-modulating action on heart, directed to maintain heart activity in patients suffering from heart failure.
Resuming the obtained data the following conclusions are made:
1) The most effective dose of 1-34 fragment PTH that regulates the contractile activity of the heart is the concentration of 10–10 M, which corresponds to a physiological dose, as it is defined in blood in norm.
2) The influence of 1-34 fragment PTH on the isolated heart is characterized by a positive chronotropic and supporting contraction amplitude effects.
3) The positive chronotropic effect induced by 1-34 PTH in vitro may be the result of activation of Ca-dependent mechanism.
4) The keeping up of the isolated heart contraction amplitude by means of PTH 1-34 is determined by the metabolism-dependent way, particularly, cAMP.
First and foremost the results of this study have important theoretical significance and are an attempt to shed more light on the involvement of calcium-regulating hormonal system including PTH into the regulatory mechanism of heart activity.
The scientific novelty of the implemented investigations is obvious and is reflected in the evidence of the scientific hypothesis on heart insufficient function protection by PTH proposed by us. In its turn it assumes the formation of a number of practical suggestions: to create methodological instructions aiming to include PTH in the heart diseases’ treatment scheme after a corresponding approbation; to observe the disorders of calcium regulating hormonal system as a risk factor of heart diseases’ development. In this aspect it is possible to suggest the elaboration of special preventive examinations which will include the study of calcium-regulating hormonal status as well as the level of calcium ions in blood.
REFERENCES
- Hara, M., Liu, Y.M., Zhen, L., et al. (1997) Positive chronotropic actions of parathyroid hormone and parathyroid hormone-related peptide are associated with increase in the current, I(f), and the slop of the pacemaker potential. Circulation, 96, 3704-3709.
- Cleemann, L. and Morad, M. (1991) Role of Ca2+ channel in cardiac excitation-contraction coupling in the rat: evidence from Ca2+ transients and contraction. Journal of Physiology, 432, 283-312.
- Levi, A.J., Brooksby, P. and Hancox, J.C. (1993) One hump or two? The triggering of calcium release from the sarcoplasmic reticulum and the voltage dependence of contraction in mammalian cardiac muscle. Cardiovascular Research, 27, 1743-1757. doi:10.1093/cvr/27.10.1743
- Ogino, K., Burkhoff, D. and Bilezikian, J.P. (1995) The homodynamic basis for the cardiac effects of parathyroid hormone (PTH) and PTH-related protein. Endocrinology, 136, 3024-3030. doi:10.1210/en.136.7.3024
- Khudaverdyan, D.N., Ter-Markosyan, A.S., Mkrtchyan, O.V. et al. (1999) The influence of parathyroid hormone on heart contractile activity. Journal of Theoretical and Clinical Medicine, 2, 3-6.
- Wang, S.Q., Song, L.S., Lakatta, E.G. et al. (2001) Ca2+ signalling between single L-type Ca2+ channels and ryanodine receptors in heart cells. Nature, 410, 592-596. doi:10.1038/35069083
- Barleta, G., De Feo, M.L., Del Bene, R., et al. (2000) Cardiovascular effects of parathyroid hormone: A study in healthy subjects and normotensive patients with mild primary hyperparathyroidism. Journal of Clinical Endocrinology & Metabolism, 85, 1815-1821. doi:10.1210/jc.85.5.1815
- Lee, K., Brown, D., Urena, P., et al. (1996) Localization of parathyroid hormone/parathyroid hormone-related peptide receptor mRNA in kidney. American Journal of Physiology, 270, F186-E191.
- Gordon, J. and Strewler, M.D. (2000) The physiology of parathyroid hormone-related protein. New England Journal of Medicine, 342, 177-185.
- Shor, R., Halabe, A., Aberbuh, E., et al. (2006) PTHrP and insulin levels following oral glucose and calcium administration. European Journal of Internal Medicine, 17, 408-411. doi:10.1016/j.ejim.2006.02.019
- Kovacs, C.S., Lannske, B., Hunzelman, J.L., et al. (1996) Parathyroid hormone-related peptide (PTHrP) regulates fetal-placental calcium transport through a receptor distinct from the PTH/PTHrP receptor. Proceedings of the National Academy of Sciences of USA, 93, 15233-15238. doi:10.1073/pnas.93.26.15233
- Strewler, G.J. (2000) The physiology of parathyroid hormone-related protein. New England Journal of Medicine, 342, 177-185. doi:10.1056/NEJM200001203420306
- Strewler, G.J. and Nissenson, R.A. (1993) Hypercalciemia in malignancy. Western Journal of Medicine, 153, 635- 640.
- Ogino, K., Ogura, K., Kinugasa, Y., et al. (2002) Parathyroid hormone-related protein is produced in the myocardium and increased in patients with congestive heart failure. Journal of Clinical Endocrinology & Metabolism, 87, 4722-4727. doi:10.1210/jc.2002-020314
- Kostyuk, P.G., Lukyanetz, E.A., Ter-Markosyan, A.S., et al. (1990) Stimulation of the neuronal calcium conductance by parathyroid hormone. Neurophysiology, 22, 373- 380.
- Kostyuk, P.G., Lukyanetz, E.A. and Ter-Markosyan, A.S. (1992) Parathyroid hormone enhances calcium current in snail neurons. Stimulation of the effect by phorbol esters. Pflügers Archiv, 420, 146-152. doi:10.1007/BF00374983
- Lutsenco, B.K., Ter-Markosyan, A.S., Khlebnikova, N.B., et al. (1987) Parathyroid hormone influence on 45Ca2+ and 3H-GABA transport in nervous ending, isolated from rat brain cortex. Bulletin of Experimental Biology and medicine, 103, 146-149.
- Arakelyan, K.P., Sahakyan, Y.A., Hayrapetyan, L.R., et al. (2007) Calcium regulating peptide hormones and blood electrolytic balance in chronic heart failure. Regulatory Peptides, 142, 95-100. doi:10.1016/j.regpep.2007.02.001
- Halapas, A, Lembessis, P, Mourouzis, I., et al. (2008) Experimental hyperthyroidism increases expression of parathyroid hormone-related peptide and type-1 parathyroid hormone receptor in rat ventricular myocardium of the Langendorff ischaemia-reperfusion model. Experimental Physiology, 93, 237-246. doi:10.1113/expphysiol.2007.039594
- Deftos, L.J., Burton, D.W. and Brandt, D.W. (1993) Parathyroid hormone-like protein is a secretory product of atrial myocytes. Journal of Clinical Investigation, 92, 727-735. doi:10.1172/JCI116643
- Smogorzewski, M, Zayed, M., Zhang, Y.B., et al. (1993) Parathyroid hormone increases cytosolic calcium concentration in adult rat cardiac myocytes. American Journal of Physiology—Heart and Circulatory Physiology, 264, H1998-H2006.
- Khudaverdyan, D.N., Ter-Markosyan, A.S. and Tadevosyan Y.V. (1997) Initiation of the Phosphoinositide Cycle by Parathyroid Hormone in Synaptosomes. Biochemistry, 62, 1109-1112.
- Klabunde, R.E. (2011) Cardiovascular Physiology Concepts. Lippincott Williams & Wilkins, Philadelphia.
- Jansen, J., Gres, P., Umschlag, C., et al. (2003) Parathyroid hormone-related peptide improves contractile function of stunned myocardium in rats and pigs. American Journal of Physiology—Heart and Circulatory Physiology, 284, H49-H55.
- Lütteke, D., Ross, G., Abdallah, Y., et al. (2005) Parathyroid hormone-related peptide improves contractile responsiveness of adult rat cardiomyocytes with depressed cell function irrespectively of oxidative inhibition. Basic research in cardiology, 100, 320-327. doi:10.1007/s00395-005-0532-9
- Zaruba, M.M., Huber, B.C., Brunner, S., et al. (2008) Parathyroid hormone treatment after myocardial infarcttion promotes cardiac repair by enhanced neovascularization and cell survival. Cardiovascular Research, 77, 722- 731. doi:10.1093/cvr/cvm080

