Risk Factors for Conjunctival Microorganism Colonization in Adults Undergoing Intraocular Surgery 29
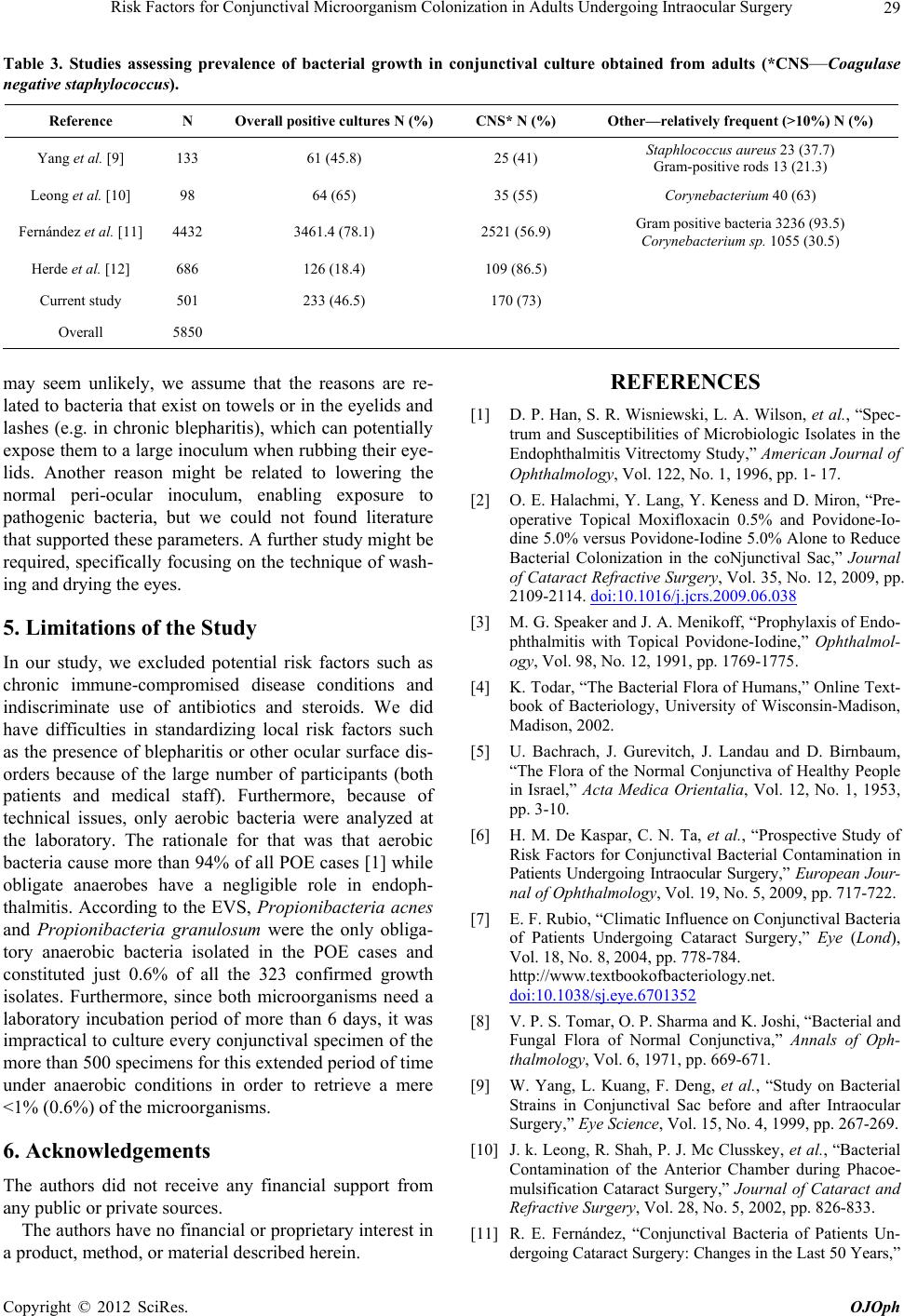
Table 3. Studies assessing prevalence of bacterial growth in conjunctival culture obtained from adults (*CNS—Coagulase
negative staphylococcus).
Reference N Overall positive cultures N (%) CNS* N (%) Other—relatively frequent (>10%) N (%)
Yang et al. [9] 133 61 (45.8) 25 (41) Staphlococcus aureus 23 (37.7)
Gram-positive rods 13 (21.3)
Leong et al. [10] 98 64 (65) 35 (55) Corynebacterium 40 (63)
Fernández et al. [11] 4432 3461.4 (78.1) 2521 (56.9) Gram positive bacteria 3236 (93.5)
Corynebacterium sp. 1055 (30.5)
Herde et al. [12] 686 126 (18.4) 109 (86.5)
Current study 501 233 (46.5) 170 (73)
Overall 5850
may seem unlikely, we assume that the reasons are re-
lated to bacteria that exist on towels or in the eyelids and
lashes (e.g. in chronic blepharitis), which can potentially
expose them to a large inoculum when rubbing their eye-
lids. Another reason might be related to lowering the
normal peri-ocular inoculum, enabling exposure to
pathogenic bacteria, but we could not found literature
that supported these parameters. A further study might be
required, specifically focusing on the technique of wash-
ing and drying the eyes.
5. Limitations of the Study
In our study, we excluded potential risk factors such as
chronic immune-compromised disease conditions and
indiscriminate use of antibiotics and steroids. We did
have difficulties in standardizing local risk factors such
as the presence of blepharitis or other ocular surface dis-
orders because of the large number of participants (both
patients and medical staff). Furthermore, because of
technical issues, only aerobic bacteria were analyzed at
the laboratory. The rationale for that was that aerobic
bacteria cause more than 94% of all POE cases [1] while
obligate anaerobes have a negligible role in endoph-
thalmitis. According to the EVS, Propionibacteria acnes
and Propionibacteria granulosum were the only obliga-
tory anaerobic bacteria isolated in the POE cases and
constituted just 0.6% of all the 323 confirmed growth
isolates. Furthermore, since both microorganisms need a
laboratory incubation period of more than 6 days, it was
impractical to culture every conjunctival specimen of the
more than 500 specimens for this extended period of time
under anaerobic conditions in order to retrieve a mere
<1% (0.6%) of the microorganisms.
6. Acknowledgements
The authors did not receive any financial support from
any public or private sources.
The authors have no financial or proprietary interest in
a product, method, or material described herein.
REFERENCES
[1] D. P. Han, S. R. Wisniewski, L. A. Wilson, et al. , “Spec-
trum and Susceptibilities of Microbiologic Isolates in the
Endophthalmitis Vitrectomy Study,” American Journal of
Ophthalmology, Vol. 122, No. 1, 1996, pp. 1- 17.
[2] O. E. Halachmi, Y. Lang, Y. Keness and D. Miron, “Pre-
operative Topical Moxifloxacin 0.5% and Povidone-Io-
dine 5.0% versus Povidone-Iodine 5.0% Alone to Reduce
Bacterial Colonization in the coNjunctival Sac,” Journal
of Cataract Refractive Surgery, Vol. 35, No. 12, 2009, pp.
2109-2114. doi:10.1016/j.jcrs.2009.06.038
[3] M. G. Speaker and J. A. Menikoff, “Prophylaxis of Endo-
phthalmitis with Topical Povidone-Iodine,” Ophthalmol-
ogy, Vol. 98, No. 12, 1991, pp. 1769-1775.
[4] K. Todar, “The Bacterial Flora of Humans,” Online Text-
book of Bacteriology, University of Wisconsin-Madison,
Madison, 2002.
[5] U. Bachrach, J. Gurevitch, J. Landau and D. Birnbaum,
“The Flora of the Normal Conjunctiva of Healthy People
in Israel,” Acta Medica Orientalia, Vol. 12, No. 1, 1953,
pp. 3-10.
[6] H. M. De Kaspar, C. N. Ta, et al., “Prospective Study of
Risk Factors for Conjunctival Bacterial Contamination in
Patients Undergoing Intraocular Surgery,” European Jour-
nal of Ophthalmology, Vol. 19, No. 5, 2009, pp. 717-722.
[7] E. F. Rubio, “Climatic Influence on Conjunctival Bacteria
of Patients Undergoing Cataract Surgery,” Eye (Lond),
Vol. 18, No. 8, 2004, pp. 778-784.
http://www.textbookofbacteriology.net.
doi:10.1038/sj.eye.6701352
[8] V. P. S. Tomar, O. P. Sharma and K. Joshi, “Bacterial and
Fungal Flora of Normal Conjunctiva,” Annals of Oph-
thalmology, Vol. 6, 1971, pp. 669-671.
[9] W. Yang, L. Kuang, F. Deng, et al., “Study on Bacterial
Strains in Conjunctival Sac before and after Intraocular
Surgery,” Eye Science, Vol. 15, No. 4, 1999, pp. 267-269.
[10] J. k. Leong, R. Shah, P. J. Mc Clusskey, et al., “Bacterial
Contamination of the Anterior Chamber during Phacoe-
mulsification Cataract Surgery,” Journal of Cataract and
Refractive Surgery, Vol. 28, No. 5, 2002, pp. 826-833.
[11] R. E. Fernández, “Conjunctival Bacteria of Patients Un-
dergoing Cataract Surgery: Changes in the Last 50 Years,”
Copyright © 2012 SciRes. OJOph