Open Journal of Nursing
Vol.3 No.2(2013), Article ID:32981,7 pages DOI:10.4236/ojn.2013.32037
Health-promoting behavior is positively associated with diabetic control among type 2 diabetes patients*
![]()
1Division of Endocrinology and Metabolism, Chang Gung Memorial Hospital, Taiwan
2Department of Diagnostic Radiology, Chang Gung Memorial Hospital, Taiwan
3Graduate Institute of Nursing, Chang Gung University of Science and Technology, Taiwan
Email: #meiyen@gw.cgust.edu.tw
Copyright © 2013 Chia-Pei Chen et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 31 March 2013; revised 15 April 2013; accepted 10 May 2013
Keywords: Type 2 Diabetes Mellitus (T2DM); Health-Promoting Behaviors
ABSTRACT
Background: The increasing prevalence of type 2 diabetes mellitus (T2DM) poses a major public health challenge throughout the world. It is a major healthcare issue among the elderly. This study was to identify the association between the health promoting behaviors and the diabetic control of type 2 diabetes mellitus (T2DM) patients. Methods: Cross sectional and descriptive research designs were used in this study. Participants were enrolled from three medical centers in northern, central and southern Taiwan during August, 2010 and June, 2011. The instruments encompassed biochemical indicators, and the preliminary developed scale of diabetes mellitus and health promotion (DMHP). Results: A total of 323 participants with T2DM were included in this study. The results showed 1) a high percentage of the participants used cigarette smoking, alcohol drinking and betel nut chewing, which were not conducive to adopting health promoting behaviors; 2) a high percentage of patients showed abnormal blood glucose, dyslipidemia, and elevated blood pressure; 3) few of the participants practiced ideally health promoting behaviors; and 4) practicing health-promoting behavior was positively associated with fasting blood glucose (FBG) and HbA1c levels. Conclusions: Patients with higher health promotion scores had better diabetic control. Less physical activity was found among those addicted to cigarette, alcohol and betel nut consumption. The findings suggest that health care providers should assess health promoting behaviors first for each diabetic patient.
1. INTRODUCTION
According to the statistics of Taiwan National Health Insurance, the prevalence of diabetes among Taiwanese adults aged 40 - 59 years is 11.4% and rises to 21.8% for people older than 60 years [1]. The mortality rate attributable to diabetes has been increasing, indicating a worrying emerging problem. Since 1990, the mortality rate of diabetic patients has increased dramatically and has been one of the top five causes of death. The standardized mortality rate in accordance with the ICD-10 classification was 26.6/105. It was higher than that of other developed countries including the USA (16.6/105), UK (5.3/105) and Japan (4.5/105) [1]. Evidence-based studies on type 2 diabetes mellitus (T2DM) indicated that the mechanisms of pathogenesis of T2DM comprise 1) impaired insulin secretion from pancreatic β-cells; 2) increased glucagon release from pancreatic α-cells; 3) abnormal hepatic gluconeogenesis; 4) muscular insulin resistance; 5) increased renal glucose reabsorption; 6) impaired insulin secretion attributable to elevated plasma levels of free fatty acids arising from increased lipolysis; 7) incretin dysfunction (release/action) and 8) hyperinsulinemia leading to attenuated and delayed responses in the hypothalamic satiety center due to dysfunction of cranial neurotransmitters [2,3].
The American Diabetes Association [4] published lifestyle modification behaviors for diabetic patients, which included healthy eating, being active, monitoring, taking medications, problem solving, and reducing risks. Studies have demonstrated that “healthy eating” behaviors could lead to significantly lower HbA1c levels among diabetic patients [4,5]. A weekly 150-minute moderateintensity exercise can improve glycemic control. These exercises include cardiopulmonary function-improving activities such as brisk walking, biking, badminton, tai chi, and aerobics mediated by repeated exercise involving large muscle groups [3,6]. “Taking medications” indicates oral anti-hyperglycemic agents and insulin injections, alone or in combination, which can effectively assist diabetic patients to achieve glycemic control and reach target levels. Meanwhile, smoking cessation may reduce the incidence of diabetic complications [3,7]. Given that diabetic foot ulceration can affect up to 25% of diabetic patients through their lives [7,8], learning about foot care is also an important diabetes self-care behavior. In addition, periodontal disease has been considered the sixth major diabetic complication, since periodontal infection vitiates metabolic control of the condition [4,9]. Therefore, it is essential to promote oral hygiene among diabetic patients. Studies have also found that patients with diabetes are more likely to develop depression. Hence, better outcomes of self management can be achieved through family and peer support [7,10].
The ideal of diabetic control was mainly assessed by measuring fasting blood glucose (FBG), glycated hemoglobin (HbA1c), blood pressure (BP), and low density lipoprotein-cholesterol (LDL-C) [1,4]. Reduced incidences of diabetes related complications have been reported when blood glucose, blood pressure and blood lipid are well controlled [4,11,12]. Some studies have shown that T2DM can be prevented or postponed by practicing the recommended healthy behaviors. For example, practicing of diabetes prevention programs in the USA and Finland have contributed to reducing the incidence rates by 58% [13-16]. From the standpoint of diabetes related health education, the fundamental practices entailed by “improving healthy behaviors and self-management of patients” have been repeatedly emphasized by experts. Although favorable health behaviors for patients with T2DM have been suggested in many studies, the broad spectrum of study scopes was derived from various perspectives on diet, exercise, oral hygiene, foot care, risk taking, social support and self-care [5,17,18]. In consequence, no simplified instrument for assessing the association of health behaviors and related health status in daily practice was available. Multiple therapeutic approaches are required for diabetic patients rather than simply relying on medications. This concept has been widely reported by many investigators but is often ignored, especially in medically-oriented clinical units. Therefore, the purpose of this study was to identify the association between practicing health promoting behaviors and diabetic control among T2DM patients.
2. METHODS
2.1. Study Design and Participants
A cross-sectional survey and descriptive design were used in this study. The participants were selected by purposive sampling in three medical centers in Northern, Central and Southern Taiwan during the period between August, 2010 and June, 2011. The inclusion criteria were: 1) patients diagnosed with T2DM by physicians; 2) adults aged 20 years and over; 3) patients fully independent in managing their daily lives; 4) patients able to complete the questionnaires by either self-administration or interview in Mandarin and Hokkien dialects; and 5) patients who agreed to sign an informed consent before being enrolled, after comprehensive explanation of the study.
2.2. Instruments
Demographic data, including gender, age, marital status, residential type, educational attainment and personal histories of cigarette smoking, alcohol consumption and betel nut chewing were collected.
Health promoting behavior was measured using the type 2 Diabetes Mellitus Health Promotion (DMHP) Scale and was preliminarily developed in this study. Face validity was examined by a critical review of the literature, professional critiques and pilot trials. Eleven experts were involved in the professional critiques and a content validity index (CVI) of 0.97 was obtained. A 5-point scale was used to cover the range between “never” and “always”. After the exploratory factor analysis, the simplified version of the DMHP was made up of six dimensions of factor structures: exercise behavior, risk reducing, enjoy-life, stress-management, health responsibility and a healthy eating. The final version of the DMHP scale consisted seven items related to “exercise” behaviors (e.g. 150 minutes of cumulative exercise per week, or daily 30-minute periods of exercise for five days, or indoor exercise activities during bad weather), seven items on “risk reducing” behaviors (e.g. examining the feet daily for redness and for swelling as well as cracks, inspecting the inside of shoes before wearing). In addition, there were four items associated with “enjoy life” behaviors (e.g. belief in meaningful life, I am content with myself), four related to “stress management” behaviors (e.g. arrangement for medication, try to understand the reasons, continue to work after diagnosis, and getting relaxation from bad moods), three related to “health responsibility” behaviors (e.g. regular outpatient visits, having eyes and cholesterol examined periodically, brushing teeth after eating) and five concerning “healthy eating”-related behaviors (e.g. 1-2 dishes of vegetables every day, avoidance of high fat foods). The internal consistency revealed that Cronbach’s α coefficient was 0.90, alpha coefficients for the subscales ranged from 0.63 to 0.88, and the total variance explained was determined as 58.4%.
Diabetic control was assessed by a BP measurement on the day of interview and the results of the latest blood laboratory tests within three months. According to the guidelines of the Diabetes Association of the Republic of China [12] and ADA [4], the ideal health indicators were determined by the biochemical indicators of FBG 90 ~ 130 mg/dl, HbA1c 7%, BP 130/80 mmHg, and LDL-C 100 mg/dl.
2.3. Ethical Issues and Procedure
Before this study was commenced, the interviewing procedures in compliance with privacy protection and ethical considerations were approved by the researchers’ Institutional Review Board (Chang Gung Memorial Hospital, No 98-1452B). The study objectives were explained in detail by interviewers from four senior certified diabetes educators. Signed informed consents were obtained from those who agreed to participate in the study.
2.4. Statistical Analysis
Descriptive and inferential statistics were processed using SPSS 15.0 software. Demographic variables, total DMHP scores, and subtotal scores of behaviors related to “exercise”, “risk reducing”, “enjoy life”, “stress management”, “health responsibility” and “healthy eating” were analyzed by t-tests or one-way ANOVA. The relationships between DMHP scores and diabetic control were evaluated by Pearson’s product moment correlation coefficient.
3. RESULTS
3.1. Demographic Characteristics
Among the total of 327 participants with T2DM, four failed to complete the questionnaires, hence the valid data were 323 subjects. Findings show that the participants were mostly male (65.9%) and the average age was 59.33 years (SD = 11.58). The mean duration of diabetes was 8.56 years (SD = 7.57) and the mean BMI was 25.81 (SD = 4.12). Most participants were overweight (67%), 50.4% had only primary school education or less. There were 15.8%, 23.6% and 9.9% still using the cigarette, alcohol and betel-nut, respectively. Blood glucose tests revealed abnormal FBG in 63.8% of the participants. An increase in HbA1c (≧7%) was found in 67.2%, among whom 21.8% had HbA1c levels higher than 9%. Abnormal BP and disordered LDL-C were found in 67.5% and 47.2% of the participants, respectively.
Regarding the practice of health-promoting behaviors, (Table 1) shows that 10 behaviors were rated below 3, a frequency between “never and sometimes”, including four items related to “exercise” behaviors (e.g. willing to do exercise during bad weather), five associated with “risk reducing” behaviors (e.g. daily inspection of feet and toes, teeth brushing or flossing after meals) and one related to “healthy eating” behaviors. In general, 22 of the 30 items were practiced at a frequency under usually. Only eight behaviors were rated as “usually and always”, including “e.g. I am content with myself; after having been diagnosed with diabetes, I continue my activities with friends”.
3.2. Relationships between Cigarette Smoking, Alcohol Drinking, Betel-Nut Chewing and Health-Promoting Behaviors
Higher scores in “healthy eating” behaviors were found in females than males (p < 0.01) (Table 2). Those younger than 50 years revealed a higher score in “risk reducing” behaviors than the other age groups (p < 0.001). In the “health responsibility” dimension, the group aged 60 - 69.9 years showed better performance than the group aged over 70 years (p < 0.05). Married participants revealed higher scores in “enjoy life” (p < 0.05) and “stress management” (p < 0.05) than single participants. College-educated participants showed higher total DMHP (p < 0.001), “risk reducing” (p < 0.001) and “healthy eating” (p < 0.001) scores.
(Table 3) shows that non-smoking participants had higher total DMHP scores (p < 0.05) and behaviors related to “healthy eating” (p < 0.01) than smokers. “Never” or “sometimes” alcohol drinkers revealed significantly higher scores in “stress management” behaviors than “usually” drinkers (p < 0.05). Participants who “never” chewed betel nuts showed significantly higher scores in total DMHP (p < 0.05) and “exercise” (p < 0.05) than those who were currently addicted to betel nut chewing (p < 0.05).
3.3. Health-Promoting Behaviors Associated with Diabetic Control
In general, six dimensions and the total DMHP score were negatively associated with FBG and HbA1c (Table 4). Additionally, participants with higher scores of “exercise” behaviors had lower FBG (p < 0.05) and HbA1c (p < 0.001). There was a negative correlation between “exercise” behaviors and systolic pressure, diastolic pressure and LDL-C, although these results did not reach statistical significance. The “risk reducing” behavior scores showed significant negative correlation to the FBG levels (p < 0.05) and systolic pressure (p < 0.05). Higher “enjoy life” scores were associated with lower levels of HbA1c
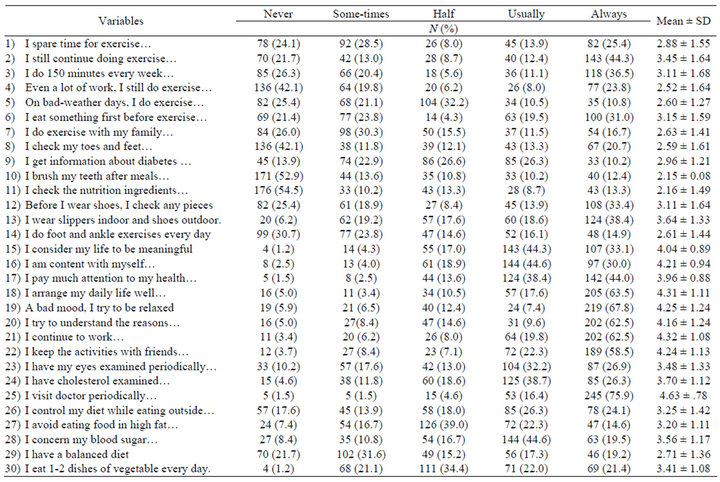
Table 1. Frequency of practicing health promoting behaviors.
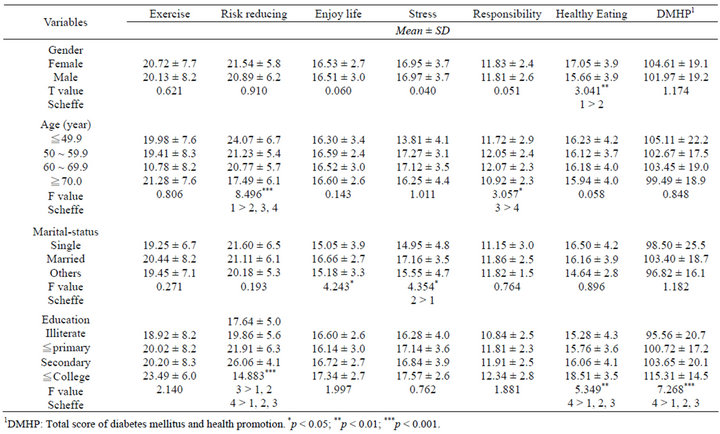
Table 2. Association of demographic characteristics and health promoting behaviors.
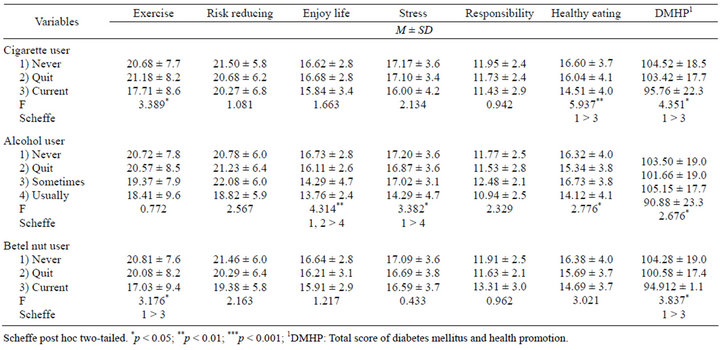
Table 3. Association between cigarette, alcohol, betel-nut consumption and health promoting behaviors.
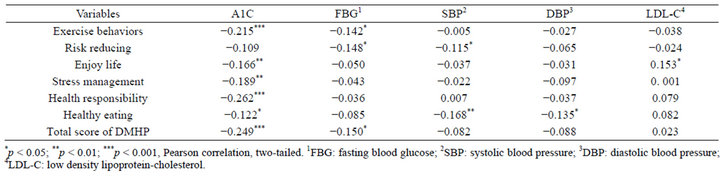
Table 4. The relationships between health promoting behaviors and diabetes control.
(p < 0.01) and LDL-C (p < 0.05). The scores for “stress management” (p < 0.01) and “health responsibility” behaviors (p < 0.001) were also significantly negative correlated with HbA1c. In addition, higher “healthy eating” scores were negatively associated with HbA1c (p < 0.05), systolic pressure (p < 0.01) and diastolic pressure (p < 0.05). Furthermore, the total DMHP scores showed negative correlations with both HbA1c (p < 0.001) and FBG (p < 0.05).
4. DISCUSSION
Although the subjects were non-randomly selected in medical centers, the demographic data were consistent with some previous domestic studies [9,17]. For example, higher percentages of males (65.9%) and those with low educational attainment were observed; many participants were persistently addicted to cigarette smoking, alcohol drinking and betel nut chewing. This study also found that if participants did not indulge in cigarette smoking, alcohol drinking and betel nut chewing, they engaged in more health-promoting behaviors. Health care providers should note that subjects with any of the three addictions are not inclined to practice health-promoting behaviors. Therefore, appropriate individually-tailored strategies are required. Some studies have shown that addiction to nicotine, alcohol and betel nuts may negatively affect the control of vasculopathy, blood glucose and blood lipids for diabetic patients [19]. However, abstinence from these three addictions was still impossible for many participants. This might be explained by the fact that most socio-economically disadvantaged individuals exhibit higher rates of smoking and lower rates of smoking cessation [20]. Therefore, further in-depth investigation is needed to develop effective strategies to help diabetic patients to reduce or quit smoking and betel nut chewing.
High percentages of participants with abnormal FBG (63.8%), HbA1c (67.2%) and BP (67.5%) were found in this study. These findings raised concerns about the participants sourced from medical centers and whether they were more ill. Similar results were reported in a study related to T2DM patients mainly from primary healthcare institutions in the communities of central and southern Taiwan, which showed that patients diagnosed for an average duration of nine years had abnormal FBG, HbA1c and BP in 58%, 57.1% and 68.1% of cases, respectively [21]. It also suggested that patients with diabetes were all poorly controlled in community healthcare institutions or medical centers. Future research is needed to investigate the causes of persistent high rates of abnormal indicators, since the government has invested huge amounts of manpower and funding in the health care system for the treatment of diabetic patients.
Female participants showed better performance in “healthy eating” behaviors than males in this study, which is consistent with the results of previous studies demonstrating better self-care behaviors in women with diabetes [22]. Some papers have reported that better self-care behaviors are associated with those who live with and are supported by their families [17]. In this study, we observed similar results showing that spouse-accompanied participants had higher scores in “stress management” behaviors. In agreement with the outcomes of previous studies, we also found that participants with higher educational attainment had better health promoting behaviors [9]. Therefore, it is suggested that the future implementation programs for promoting healthy behaviors should emphasis on those who are male, older, with lower educational attainment and insufficient family support.
In general, better control of HbA1c was associated with more active health promoting behaviors, including “exercise”, “enjoy” life, “stress management”, “health responsibility” and “healthy eating”. It was consistant with the conclusions of other studies [23]. For example, “healthy eating” behaviors significantly lowered HbA1c levels [24]. Diabetic patients could achieve and maintain significantly better glycemic control, lowering the risk of cardiovascular diseases, managing body weight and reducing the levels of FBG and HbA1c by regular exercise [25]. In addition, Gleeson-Kreig et al. [18] indicated that those with stronger family and social support presented better self-care behaviors. However, we only observed eight items of health-promoting behaviors performed at “always” frequency in this study (Table 2). Therefore, continuous interventions on health-promoting behaviors still need to be strengthened for T2DM patients in medical centers.
The study was limited by certain factors: all the subjects were medical center-based, sampling was non-randomized, survey design was cross-sectional, and analysis was descriptive. In consequence, inferences from the results and causal explanations were restricted. For a future study, it is suggested that T2DM patients from communities are included in the sampling. Differences between urban and rural areas as well as socio-economic background should also be considered. A study design in conjunction with patients from communities, giving individualized health-promoting behaviors oriented by different backgrounds, may more substantially indicate the effectiveness of the DMHP Scale in assessing the health status of T2DM patients.
5. CONCLUSION
This study indicated that practicing health-promoting behaviors led to better control of FBG and HbA1c. Many participants were still addicted to cigarette smoking, alcohol drinking and betel nut chewing, which are not conducive to practicing health promoting behaviors. Further, the proportion of participants who often practiced health promoting behaviors remained low. Therefore, health care providers should assess health promoting behaviors for each diabetic patient before giving any counseling.
REFERENCES
- Department of Health (DOH), Executive Yuan, Taiwan (2001) Annual report for health statistics of national health insurance. http://www.doh.gov.tw/CHT2006/DM/DM2_2_p02.aspx?class_no=440&now_fod_list_no=11587&level_no=3&doc_no=79126
- DeFronzo, R. (2009) From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes, 58, 773. doi:10.2337/db09-9028
- World Health Organization (WHO) (2011) Diabetes. http://www.who.int/topics/diabetes_mellitus/en/
- American Diabetes Association (ADA) (2008) Standards of medical care in diabetes. Diabetes Care, 32, S62-S63.
- Aikens, J.E., Bingham, R., Piette, J.D. (2005) Patientprovider communication and self-care behavior among type 2 diabetes patients. The Diabetes Educator, 31, 681- 690. doi:10.1177/0145721705280829
- Haskell, W.L. and Lee, I.M. (2007) Physical activity and public health: Updated recommendation for adults from the American college of sports medicine and the American Heart Association. Circulation, 116, 1081-1093. doi:10.1161/CIRCULATIONAHA.107.185649
- Miller, D.K. and Fain, J.A. (2006) Diabetes self-management education. NCNA, 41, 655-666. doi:10.1016/j.cnur.2006.07.010
- Singh, N., Armstrong, D.G. and Lipsky, B.A. (2005) Preventing foot ulcers in patients with diabetes. JAMA, 293, 217-228. doi:10.1001/jama.293.2.217
- Wang, H.F., Tang, W.R. and Liu, H.E. (2008) Related factors of diabetes mellitus disease features and quality of life: The report of a regional teaching hospital in central Taiwan. Endocrinology & Diabetology, 21, 1-15.
- Scollan-Koliopoulos, M. (2004) Consideration for legacies about diabetes and self-care for the family with a multigenerational occurrence of type 2 diabetes. Nursing & Health Sciences, 6, 223-227. doi:10.1111/j.1442-2018.2004.00196.x
- American Association of Diabetes Educators (AADE) (2008) AADE7TM Self-Care Behaviors. The Diabetes Educator, 34, 445-449. doi:10.1177/0145721708316625
- The Diabetes Association of the Republic of China (2010) Clinical care guidelines for diabetes. The Diabetes Association of the Republic of China, Taipei.
- Hamman, R.F., Wing, R.R. and Edelstein, S.L. (2006) Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care, 29, 2102-2107. doi:10.2337/dc06-0560
- Laaksonen, D.E., Lindstrom, J. and Lakka, T.A. (2005) Physical activity in the prevention of type 2 diabetes: The Finnish diabetes prevention study. Diabetes, 54, 158-165. doi:10.2337/diabetes.54.1.158
- Knowler, W.C., Barrett-Connor, E. and Fowler, S.E. (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England Journal of Medicine, 346, 393-403. doi:10.1056/NEJMoa012512
- Tuomilehto, J., Lindstro, J. and Eriksson, J.G. (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. The New England Journal of Medicine, 344, 1343-1350. doi:10.1056/NEJM200105033441801
- Chang, H.Y., Chiou, C.J. and Lin, M.C. (2004) A population study of the self-care behaviors and their associated factors of diabetes in Taiwan: Results from the 2001 national health interview survey in Taiwan. Preventive Medicine, 40, 344-348. doi:10.1016/j.ypmed.2004.06.012
- Gleeson-Kreig, J., Bernal, H. and Woolley, S. (2002) The role of social support in the self-management of diabetes mellitus among a Hispanic population. Public Health Nursing, 19, 215-222. doi:10.1046/j.0737-1209.2002.19310.x
- Kim, J., Kim, K. and Moon, J. (2011) Alcohol use behaviors and risk of metabolic syndrome in South Korean middle-aged men. BMC Public Health, 11, 489. doi:10.1186/1471-2458-11-489
- Harwood, G.A., Salsberry, P. and Ferketich, A.K. (2007) Cigarette smoking, socioeconomic status, and psychosocial factors: Examining a conceptual framework. Public Health Nursing, 24, 361-371. doi:10.1111/j.1525-1446.2007.00645.x
- Chen, M.Y., Huang, W.C., Peng, Y.S., Guo, J.S., Chen, C.P., Jong, M.C. and Lin, H.C. (2011) Effectiveness of a health promotion program for farmers and fishermen with type 2 diabetes in Taiwan. Journal of Advanced Nursing, 67, 2060-2067. doi:10.1111/j.1365-2648.2011.05678.x
- Aljasem, L.I., Peyrot, M., Wissow, L., et al. (2001) The impact of barriers on self-efficacy and self-care behavior in type 2 diabetes. The Diabetes Educator, 27, 393-404. doi:10.1177/014572170102700309
- Irwin, M.L., Mayer-Davis, E.J., Addy, C.L., et al. (2000) Moderate-intensity physical activity and fasting insulin levels in women: The cross-cultural activity participation study. Diabetes Care, 23, 449-454. doi:10.2337/diacare.23.4.449
- Jones, H., Edwards, L. and Vallis, T.M. (2003) Changes in diabetes self-care behaviors make a difference in glycemic control: The diabetes stages of change study. Diabetes Care, 26, 732-737. doi:10.2337/diacare.26.3.732
- Yokoyama, H., Emoto, M. and Araki, T. (2004) Effect of aerobic exercise on plasma adiponectin levels and insulin resistance in type 2 diabetes. Diabetes Care, 27, 1756- 1758. doi:10.2337/diacare.27.7.1756
NOTES
*The authors declare that they have no competing interests.
CC and MC designed the study conception and wrote the manuscript. YP and HW carried out statistical analysis and supervision. HY par- ticipated in data collection. All authors contributed to manuscript development, and read and approved the final manuscript.
#Corresponding author.

