Health
Vol.5 No.1(2013), Article ID:26858,7 pages DOI:10.4236/health.2013.51014
HIV prevention: Towards a “structural-plus” approach
![]()
1Health Policy Research Unit, Institute of Economic Growth, University of Delhi, Delhi, India; *Corresponding Author: ig.indrani@gmail.com
2Population Research Centre, Institute of Economic Growth, University of Delhi, Delhi, India
3Jawaharlal Nehru University, New Delhi, India
Received 15 November 2012; revised 17 December 2012; accepted 25 December 2012
Keywords: HIV; Prevention; Structural Factors; Development
ABSTRACT
Lack of integration and coordination between HIV prevention programmes and developmental programmes explain why many countries have not been able to halt the epidemic, and others still have unacceptably high prevalence. A framework is presented here with supporting evidence to argue that existing structural interventions may be unsustainable in the long run because they do not address core developmental issues or the “structural plus factors”. This problem emanates from the almost total administrative and intellectual disconnect between policies that address development issues and those that address HIV prevention. Usual prevention packages may result only in short term benefits. To get the most out of limited global resources on prevention, it is critical that planners recognize and understand that parallel policies for AIDS prevention and development are not going to be cost-effective and sustainable, and the only option is to approach prevention as well as development in an integrated manner.
1. INTRODUCTION
The last two decades of HIV/AIDS prevention and control have shown mixed effectiveness across situations. As such, new infections have stabilized in many parts of the world but the incidence continues to rise in parts of Eastern Europe, Central Asia, Oceania, Middle-East and North Africa [1]. Besides, sustained prevalence among African nations continues to dominate the international scenario. Such inconsistency in effectiveness is arguably associated with limited contextualisation of prevention efforts across “diverse settings” (Bertozzi et al., 2008, Piot et al., 2009) often conceived in terms of the class of epidemic: low-level concentrated, generalized, or hyperendemic [2]. Moreover, from a programme perspective, the developmental context is treated as the operational environment consisting of critical but non-changeable factors that impinge on behaviour and make for differential impact of HIV interventions [3]. As a consequence, the structural determinants of risk behaviour do not usually include diverse developmental factors that might explain the variation in prevalence levels across countries. This also translates into an administrative and intellectual separation between prevention policies and developmental policies that often result in unsustainable interventions for HIV prevention. This paper revisits the notion of “structural factors” in HIV interventions, examines the possibility of expanding the set comprising structural factors and analyzes the scope for integration with conventional behavioural interventions.
2. RELEVANCE OF STRUCTURAL FACTORS: A REVIEW
Successful prevention strategies are well-documented as “best-practices” in HIV prevention [4] and various taxonomies are available to classify such interventions. For instance, recent studies use the following three-way classification (Table 1): behavioural interventions, biomedical interventions, and structural interventions [5,6]. To elaborate, behavioural change interventions are supposed to reduce risk of HIV infection by influencing behaviour through knowledge, awareness and improved access to services. This comprises a range of educational, motivational, peer-group based, skills-building and community normative approaches [7]. Behavioural barriers to access critical services such as condom distribution and counselling are specifically addressed through such interventions. Biomedical interventions comprise medical interventions that help to prevent infection, reduce infectiousness, and minimize the risk of transmission and acquisition of HIV/AIDS. The goal is to moderate the
Table 1. Classification of standard HIV prevention interventions: Some examples.

influence of biological or physiological factors that may increase infectiousness or susceptibility to HIV and prevent infection from progressing after actual exposure [8]. Structural interventions like women’s empowerment and awareness-building through mass media campaigns assume importance because of the recognition that broader social, economic, political and environmental issues influence individual risk and vulnerability to HIV/AIDS, and are critical for effective prevention [9]. These factors, in turn, are closely related to the regional patterns of growth and development and generally lie outside the purview of targeted HIV/AIDS interventions.
While conventional behavioural and biomedical strategies remain at the heart of most interventions, the structural approach was relatively a more recent addition to the burgeoning literature around effective and sustainable prevention strategies [10,11]. Undeniably, the performance of behavioural change interventions to a greater extent is determined by the presence (or absence) of facilitating structural environments. For example, advocacy and training are more effective under conditions where the societal perspective is not stigmatizing and the legal environment is protective of the risk groups. In fact, advocacy and training is more effective if the structural vulnerabilities like income deprivations of risk groups are minimal. In this context, examples relating to market for unprotected commercial sex indicate that a segment of sex workers are willing to take the risk if premium clients have an inherent preference for condom-free sex [12-14]. Therefore, it follows that despite information and availability of HIV prevention strategies, it is likely that a significant amount of unprotected commercial sex will continue to occur, albeit at a higher price [13]. In a nutshell, the broader implications of these results are that interventions focusing merely on the supply side might not be very effective.
Structural interventions locate the source of health problems in factors relating to availability, acceptability, or accessibility, and are targeted at the individual, organizational, or environmental levels [15]. Such an integrated approach that considers all types of interventions together as a package is now seen as the most effective way forward for HIV prevention [7,9,16]. The efficacy of biomedical interventions depends on the context, especially structural barriers, and the extent of success of behavioural interventions that attempt to alter such barriers. Risk factors are often seen to be influenced by structural factors such as the type and level of economic growth and development, cultural practices, social norms, legal and policy environment, and the socio-economic profile of the region [11,17]. Clearly, there are multiple ways in which the underlying structural factors can manifest themselves as risk in different settings and at different times [18,19]. For instance, low potential for female labour market earnings is often taken to be an important reason why women go into prostitution [20]. Similarly, interventions with high risk population groups and bridge population alone may not be sufficient to guarantee reversal of the AIDS epidemic [21,22].
Broadening the scope of the term “structural” to include socioeconomic parameters that operate at a more macro level of the economy can help in a deeper understanding of what works in HIV prevention, where it works and why it works. Generally, development and socio-economic issues are discussed in the context of vulnerabilities of population groups to HIV and its subsequent impact, especially within developing countries [23,24], as has been done by several Human Development Reports (HDRs) with HIV/AIDS theme. There is almost total consensus that HIV programmes should be integrated or “mainstreamed” within developmental planning instruments like poverty reduction strategies, through multisectoral coordination. It has been contended that poverty on its own cannot be viewed simplistically as a driver of the HIV epidemic but as a multidimensional facilitator that influences mobility, social and economic inequalities and social capital [24,25]. A good example is of migration, which is seen as a key factor in the spread of HIV in developing countries [21,26-29]. Governance and administrative factors, political commitment, infrastructure, and human resource requirements are also seen as important variables in making interventions effective [25, 30-34].
This review indicates that there is an inherent recognition of these broader socioeconomic correlates of HIV; our contention is that this recognition has not translated into designs of prevention programmes, which continue to only recognize the traditional structural factors. For sustainable behaviour change beyond the short term, the investment seen as “structural” may have to be augmented by investing on strategies that pertain to larger macro and developmental concerns of a country. We call such factors are called “structural plus” factors and analyze how investment in these factors can help create an “enabling environment” and can enhance the effectiveness of usual structural or behaviours interventions.
3. “STRUCTURAL-PLUS” FACTORS AND HIV PREVALENCE
Human development and governance has received less analytical and programmatic attention. As such, it has a significant bearing on HIV prevalence and its implications can be discerned by some elementary analysis. For example, Figure 1 plots UNDP’s Human Development Index (HDI) values for 20 high HIV prevalence countries for the years 1995 and 2010, and reveals a negative association between HIV prevalence and human development. It is worth highlighting that these high-prevalence countries have performed differently over the years in terms of HDI as well as HIV prevalence. It is evident that HDI and HIV do not necessarily move together as indicated by the experience of Swaziland, Botswana, Lesotho, South Africa and Namibia that demonstrate dwindling prevention effectiveness despite considerable gain in HDI. Uganda is often cited as an example for successfully containing infection rates following an “ABC” (abstinence, be-faithful and condom) prevention approach during 1990s [35]. However, these effects have faded gradually due to shortage of condoms, shifts from abstinence based prevention policy and changed perceptions about risk due to availability and access to treatment [36].
Clearly, HDI is a simple aggregation of three factors that have both intrinsic and instrumental values; however, sustained improvements in HIV prevalence requires further developmental assistance, particularly in the field of economic livelihood, women empowerment, human rights, institutions and governance. Thus, for instance, if livelihood issues and lack of functioning educational institutions are critical in adolescent risk-taking behaviour, then additional and parallel investments in employment generating activities and education are indispensable. We validate this argument by presenting some cross-sectional evidence based on data from 100 countries.
In particular, we study the association between HIV

Source: [37,38]. Note: The 20 countries are: ZIM, Zimbabwe; BTS, Botswana; ZAM, Zambia; LES, Lesotho; MAL, Malawi; SWA, Swaziland; UGA, Uganda; TNZ Tanzania; RWD, Rwanda; NAM, Namibia; SAF, South Africa; CDI, Cote d’Ivoire; BUR, Burundi; CAR, Central African Republic; CAM, Cameroon; MOZ, Mozambique; GUY, Guyana; GAB, Gabon; TOG, Togo; THA, Thailand.
Figure 1. HDI and HIV prevalence for 20 high prevalence countries in 1995 & 2010.
prevalence and key developmental factors such as HDI, gender inequality, rate of growth of GDP, Gini coefficient of income inequality, and corruption index for good governance. The ordinary least squares regression results are presented in Table 2 which suggests that apart from HDI, income inequality and governance are the three most important correlates of HIV prevalence across countries. The rate at which income grows is insignificant, which is not surprising, because the quality (or composition)—rather than quantity—of growth is an important determinant of risk factors and vulnerability to HIV. Gender inequality also has expected direction of improvement (though statistically insignificant) indicating that gender equity is a desirable component of an ideal structural environment.
Furthermore, we focus on the bivariate association between HIV prevalence across countries and Gross Domestic Product (GDP), GDP per capita, GDP growth rate, public spending on health and education as a percentage of GDP, and proportion of vulnerable employment defined as unpaid family workers and own-account workers as a percentage of total employment. For analytical purposes, the World Development Indicators data for 164 countries and four different time points 1990, 1995, 2000 and 2005 is used.
The concentration index (CI) is used to examine the association between key developmental indicators and HIV prevalence [39]. HIV prevalence is defined as a dichotomous variable and countries with adult HIV prevalence exceeding one percent are defined as high prevalence countries. As such, the CI ranges between +1 and −1 and in this instance provides a measure of the extent of association in prevalence that is systematically associated with developmental indicators. If high HIV prevalence is concentrated among countries with low developmental indicators then the concentration index would be negative. The larger the value of the CI the greater is the strength of the association.
Table 3 presents the CI estimates for the association between high HIV prevalence (exceeding one percent) and various developmental indicators. The negative CI coefficients for the associations between HIV and GDP across four time points indicate that high HIV prevalence is heavily concentrated among countries ranking low in terms of GDP. For instance, we find a CI value of −0.246 in the year 1990, which gradually increases to −0.313 by 2005. The negative association between income and HIV further intensifies when GDP is adjusted for population size and defined as GDP per capita. The CI value of −0.455 for the year 1990 continues to be on the higher side throughout the decade of 1990s and is computed to be −0.388 for the year 2005.
Table 2. Cross-section regression of “structural plus” factors on HIV prevalence.

Note: *significant at 5 percent; **significant at 1 percent. The data has been obtained from World Development Indicators 2010, Human Development Report 2010, and Transparency International 2010.
Table 3. Concentration Index for association between HIV prevalence and development, with Standard Error.
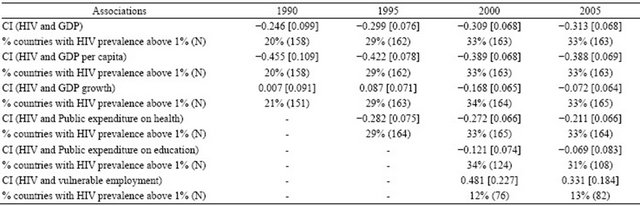
Source: Estimated using WDI indicators (1990, 1995, 2000 and 2005). Note: (.) indicates number of countries (N); [.] indicates standard error [s.e].
There is an interesting relationship between HIV prevalence and GDP growth rate: at the beginning of the 1990s there was no systematic association between growth rate and HIV prevalence (CI = 0.007) but by the end of the 1990s HIV prevalence displayed significant concentration among countries with negative or low GDP growth rates (CI −0.168 in 2000). Perhaps, a lack of concentration in 1990 can be attributed to the widespread emergence of the epidemic across contexts but subsequently countries with better growth and development were able to reduce their prevalence. The situation in the last decade suggests that countries with poor growth performance are the ones sustaining a high prevalence rate. Undeniably, public expenditure on health and education are critical components of the structural-plus matrix and the analysis suggests that HIV prevalence shares a negative association with these developmental correlates as well. Specifically, countries with relatively high public expenditure are seen to share less of the burden then compared to countries with low public health expenditure. Public expenditure on education also shares a similar relationship but because of data limitations for several countries the effects are not captured fully. Finally, a vital perspective that we observe pertains to the high proportion of vulnerable employment in an economy and its significant association with HIV prevalence. The high CI values of 0.48 for the year 2000 suggests that HIV epidemic had mostly affected countries with large share of population in vulnerable employment. This association is sustained over the decade and therefore interventions seeking to reverse the epidemic should consider quality of employment and growth as key structural-plus factors.
4. DISCUSSION AND CONCLUSION
This review and analysis indicates the centrality of “structural plus” factors in the HIV epidemic. Despite this, there has not been much integration of HIV/AIDS prevention efforts with other developmental investment across countries. One key reason is that investment decisions on vital “structural-plus” factors are not under the purview of institutions implementing National AIDS Control Programmes (NACP), and there exists an administrative as well as intellectual separation between the two streams in policymaking. NACPs have neither the mandate nor the resources to invest on activities that may have a sustainable impact on HIV prevention. Despite efforts at mainstreaming HIV/AIDS interventions into planning, budgeting and implementation, it has not been possible to really harmonize and integrate development and HIV/AIDS prevention strategies with development strategies in most countries [40].
The recent rise in infections in Eastern Europe and Central Asia indicate very clearly that mere economic growth is not sufficient to dampen the spread of the infection. This region has had fairly robust growth, but despite that it is witness to the most rapidly spreading HIV epidemic. The vulnerabilities in this region has to do with injecting drug use that developed in the mid- 1990s during the socioeconomic crisis that followed the break-up of the Soviet Union [41]. The affected groups remain the economically and socially weaker sections of the population with a strong association with unemployment [41].
Table 4 summarizes the key arguments of this paper and illustrates why a “structural-plus” approach might need more focus than the standard efforts at mainstreaming. As can be seen, countries with high adult HIV prevalence also have low HDI rank, high poverty, high income inequality and high corruption. The GDP growth rate, however, varies from negative to fairly high, with Botswana, Namibia and Mozambique displaying moderate to high rates of GDP growth.
Table 4. Selected “structural plus” indicators in 10 countries with highest HIV prevalence.
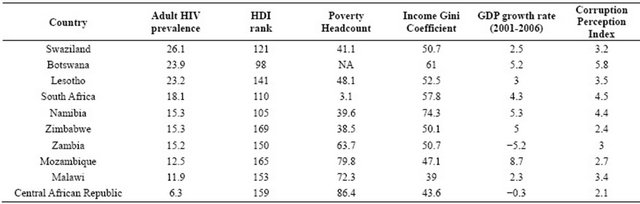
Source: The data on adult HIV prevalence is from UNAIDS, 2010. GDP growth rate, poverty headcount and Gini coefficient has been obtained from World Development Indicators 2010, Indicators for rank of countries as per human development index (HDI) is from Human Development Report 2010, and corruption perception index is obtained from Transparency International 2010.
Botswana also has better corruption indicator than the other countries, but very high inequality. Apparently, in almost all these countries, the mining sector is the key driver of GDP, exports and employment and its linkages with HIV/AIDS are well established. For instance, in a different context [21] have contended that the mining sector does not lead to a growth pattern that is consistent with human development and such patterns of growth tend to throw up a whole nexus of vulnerabilities that are conducive to a rapid spread of HIV.
Our conclusions are that prevention programmes may not be sustainable in the long run if not complemented with, and accompanied by, fundamental investment in human development that reduce poverty and inequalities on the one hand, and provide a conducive legal, political and administrative framework that permit good governance on the other. These factors go beyond the usual structural interventions that are often added to prevention programmes to make these more effective. For example, in areas with high school and college drop outs and low employment opportunities, structural interventions like syringe exchange programme or condom availability would only have limited effectiveness. Similarly, rehabilitation of sex workers would require not only political and legal interventions but also solutions where employment generation for vulnerable women has to be a key part of any package of intervention meant for sex workers.
Schemes that use peers or offer micro credit are important but not sustainable unless quantum jump that are sustainable over time are made in the economic and social status of sex workers.
The foregoing arguments are even more convincing in the context of new infections. While usual structural interventions can work at a point in time, the prevention of new infections requires continuous funding of such programmes on a long term basis to specifically address the needs of new entrants into the vulnerable pool, and may soon meet administrative and financial roadblocks, especially in developing countries. Clearly, engaging with growth that is inconsistent with human development, negatively impact on HIV prevention efforts, and result in misallocation of global funding for prevention. The most effective and sustainable prevention of HIV would continue to be an equitable growth strategy that is consistent with all round human development; only this can act as a true “enabling environment” for the usual structural factors to perform their functions. Any other option would only end up wasting global scarce resources for HIV prevention.
5. ACKNOWLEDGEMENTS
This research was supported under the “Knowledge Network Project”, a research programme consortium led by Population Council, New Delhi and funded by the Bill & Melinda Gates Foundation.
![]()
![]()
REFERENCES
- UNAIDS (2011). UNAIDS World AIDS Day Report.
- UNAIDS (2008) A Framework for Classifying HIV-prevention interventions. UNAIDS, Geneva.
- Wilson, D. and Halperin, D.T. (2008) Know your epidemic, know your response: A useful approach, if we get it right. The Lancet, 372, 423-426. doi:10.1016/S0140-6736(08)60883-1
- Makinwa, B. and O’Grady, M., Eds. (2001). Best practices in HIV/AIDS prevention collection. FHI/UNAIDS, Geneva.
- Padian, N.S., Buve, A., Balkus, J. and Serwadda Jr., D.W.C. (2008) Biomedical interventions to prevent HIV infection: Evidence, challenges, and way forward. The Lancet, 372, 585-599. doi:10.1016/S0140-6736(08)60885-5
- Galárraga, O., Colchero, M.A., Wamai, R.G. and Bertozzi, S.M. (2009) HIV prevention cost-effectiveness: A systematic review. BMC Public Health—BioMed Central, 9, S1-S15.
- Coates, T.J., Richter, L. and Caceres, C. (2008) Behavioural strategies to reduce HIV transmission: How to make them work better. The Lancet, 372, 669-684. doi:10.1016/S0140-6736(08)60886-7
- Ross, D., Dick, B. and Ferguson, J., Eds., (2006) Preventing HIV/AIDS in young people: A systematic review of the evidence from developing countries. WHO Technical Report Series No. 938, World Health Organization, Geneva.
- Gupta, G.R., Parkhurst, J.O., Ogden, J.A., Aggleton, P. and Mahal, A. (2008) Structural approaches to HIV prevention. The Lancet, 372, 764-775. doi:10.1016/S0140-6736(08)60887-9
- Campbell, C. and Williams, B. (1999) Beyond the biomedical and behavioural: Towards an integrated approach to HIV prevention in the Southern African mining industry. Social Science & Medicine, 48, 1625-1639. doi:10.1016/S0277-9536(98)00449-3
- Sweat, M.D. and Denison, J.A. (1995) Reducing HIV incidence in developing countries with structural and environmental interventions. AIDS, 9, S251-S257.
- Philipson, T.J. and Posner, R.A. (1993) Private choices and public health: The AIDS epidemic in an economic perspective. Harvard University Press, Cambridge.
- Gertler, P., Shah, M. and Bertozzi, S.M. (2005) Risky business: The market for unprotected commercial sex. Journal of Political Economy, 113, 518-550. doi:10.1086/429700
- Rao, V., Gupta, I., Lokshin, M. and Jana, S. (2003) Sex workers and the cost of safe sex: The compensating differential for condom use among Calcutta prostitutes. Journal of Development Economics, 71, 585-603. doi:10.1016/S0304-3878(03)00025-7
- Balnkenship, K.M., Bray, S.J. and Merson, M.H. (2000) Structural interventions in public health. AIDS, 14, S11- S21. doi:10.1097/00002030-200006001-00003
- Merson, M.H., O’malley, J., Serwadda, D. and Apisuk, C. (2008) The history and challenge of HIV prevention. The Lancet, 372, 475-488. doi:10.1016/S0140-6736(08)60884-3
- Sumartojo, E., Doll, L., Holtgrave, D., Gayle, H. and Merson, M. (2000) Enriching the mix: Incorporating structural factors into HIV prevention. AIDS, 14, S1-S2. doi:10.1097/00002030-200006001-00001
- David, A.C. and Li, C.A. (2010) Exploring the links between HIV/AIDS, social capital and development. Journal of International Development, 22, 941-961. doi:10.1002/jid.1707
- Parkhurst, J.O. (2010) Understanding the correlations between wealth, poverty and human immunodeficiency virus infection in African countries. Bulletin of the World Health Organization, 88, 519-526. doi:10.2471/BLT.09.070185
- Edlund, L. and Korn, E. (2002) A theory of prostitution. Journal of Political Economy, 110, 181-214. doi:10.1086/324390
- Gupta, I., Trivedi, M. and Guin, P. (2008) Understanding HIV & development: An analysis from Bellary district in Karnataka, India. UNDP, New Delhi.
- Piot, P., Kazatchkine, M., Dybul, M. and Lob-Levyt, J. (2009) AIDS: Lessons learnt and myths dispelled. The Lancet, 374, 260-263. doi:10.1016/S0140-6736(09)60321-4
- Gilbert, L. and Walker, L. (2002) Treading the path of least resistance: HIV/AIDS and social inequalities‚ Äîa South African case study. Social Science & Medicine, 54, 1093-1110. doi:10.1016/S0277-9536(01)00083-1
- Greener, R. and Sarkar, S. (2010) Risk and vulnerability: Do socioeconomic factors influence the risk of acquiring HIV in Asia? AIDS, 24, S3-S11. doi:10.1097/01.aids.0000390084.37812.30
- Kim, J., Pronyk, P., Barnett, T. and Watts, C. (2008) Exploring the role of economic empowerment in HIV prevention. AIDS, 22, S57-S71. doi:10.1097/01.aids.0000341777.78876.40
- Decosas, J. (1996) HIV and development. AIDS, 10, S69- S74.
- Soskolne, V. and Shtarkshall, R.A. (2002) Migration and HIV prevention programmes: Linking structural factors, culture, and individual behaviour—an Israeli experience. Social Science & Medicine, 55, 1297-1307. doi:10.1016/S0277-9536(01)00282-9
- Lurie, M.N., Williams, B.G., Zuma, K., Mkaya-Mwamburi, D., Garnett, G.P., Sturm, A.W., Sweat, M.D., Gittelsohn, J. and Karim, S.S.A. (2003) The impact of migration on HIV-1 transmission in South Africa: A study of migrant and nonmigrant men and their partners. Sexually Transmitted Diseases, 30, 149-156. doi:10.1097/00007435-200302000-00011
- Crush, J., Williams, B., Gouws, E. and Lurie, M. (2005) Migration and HIV/AIDS in South Africa. Development Southern Africa, 22, 293-318. doi:10.1080/03768350500253153
- Over M. (1997) The effect of societal variables on urban rates of HIV infections in developing countries. In: Ainsworth, M., Fransen, L. and Over, M., Eds., Confronting AIDS: Evidence from the Developing World, European Commission, Brussels, 39-51.
- Mahal, A. (2001) The human development roots of HIV and implications for policy: A cross country analysis. Journal of Health and Population in Developing Countries, 4, 43-60.
- Hogan, D.R., Baltussen, R., Hayashi, C., Lauer, J.A. and Salomon, J.A. (2005) Cost effectiveness analysis of strategies to combat HIV/AIDS in developing countries. British Medical Journal, 331, 1431-1437. doi:10.1136/bmj.38643.368692.68
- O’leary, A. and Martins, P. (2000) Structural factors affecting women’s HIV risk: A life-course example. AIDS, 14, S68-S72. doi:10.1097/00002030-200006001-00011
- Clark, R.C. and Vencatachellum, D. (2003) Economic development and HIV/AIDS prevalence. Economic Development and HIV/AIDS Prevalence Scientific Series. Centre Interuniversitaire de Recherche en Analyse Des Organisations, Montreal.
- Green, E., Halperin, D., Nantulya, V. and Hogle, J. (2006) Uganda’s HIV prevention success: The role of sexual behavior change and the national response. AIDS and Behavior, 10, 335-346. doi:10.1007/s10461-006-9073-y
- Dzenovska, D., Rasheed, N. and Sandkjær, B. (2005) HIV/AIDS and human development: Thematic guidance note. NHDR Occasional Paper 4. National Human Development Reports Unit, Human Development Report Office, UNDP.
- UNAIDS (2010) Global Report: UNAIDS report on the global AIDS epidemic. UNAIDS, Geneva. www.unaids.org/documents/20101123_GlobalReport_em.pdf
- UNDP (2010) Human Development Report 2010.
- Wagstaff, A, Paci, P. and van Doorslaer, E. (1991) On the measurement of inequalities in health. Social Science and Medicine, 33, 545-557. doi:10.1016/0277-9536(91)90212-U
- Rau, B. and Collins, J. (2000) AIDS in the context of development. Joint United Nations Programme on HIV/ AIDS, UNRISD.
- Avert (2012) HIV and AIDS in Russia, Eastern Europe and Central Asia. http://www.avert.org/aids-russia.htm

