Open Journal of Pediatrics
Vol. 2 No. 2 (2012) , Article ID: 19877 , 3 pages DOI:10.4236/ojped.2012.22029
Congenital sepsis caused by Eikenella corrodens
![]()
1University of Virginia School of Medicine, Charlottesville, USA
2Pediatric Infectious Disease Group, Inova Health System Hospital for Children, Fairfax, USA
3Department of Pediatrics, Inova Health System Hospital for Children, Fairfax, USA
Email: jcrewalk@kidspid.com
Received 30 November 2011; revised 2 May 2012; accepted 11 May 2012
Keywords: Neonatal Sepsis; Intrauterine Infection; Chorioamnionitis
ABSTRACT
Eikenella corrodens is a part of normal human oral flora and a rare cause of intrauterine and neonatal infections. We describe a case of congenital E. corrodens sepsis with positive blood cultures at birth in the setting of low maternal risk factors for infection. Our case is one of two reported cases of congenital E. corrodens sepsis resulting in newborn survival.
1. INTRODUCTION
Eikenella corrodens is a slow-growing, facultative anaerobic gram-negative bacillus that is known to cause serious human illnesses. Known cases include head and neck infections, meningitis, endocarditis, intra-abdominal infections, skin infections, and infection after human bite wounds [1]. The bacterium is a part of human oral, upper respiratory and gastrointestinal flora, and as such, it has classically been associated with exposure to human oral secretions. It is susceptible to a wide range of antibiotics, such as ampicillin, gentamicin, penicillin G, trimethoprim-sulfamethoxazole, amoxicillin-clavulanic acid, cefotaxime, and ceftriaxone [2]. Interestingly, it is typically resistant to metronidazole and clindamycin, which are usually effective in treating infections caused by human oropharyngeal flora. Co-infection is also observed, especially with streptococci species [1]. While E. corrodens may cause a variety of infections, obstetric and neonatal infections are much less common.
Materno-fetal infections caused by E. corrodens have been associated with preterm labor and neonatal morbidity and mortality. Reports of such cases have typically involved chorioamnionitis [3]. Different routes of infection have been proposed, including hematogenous spread from the oral cavity or from bite wounds, as well as ascending vaginal infection following oral-genital sex during pregnancy [4]. While more recent studies have shown an increase in gram-negative bacteria as a cause of neonatal infections, E. corrodens remains a rare etiology of neonatal sepsis [5].
We searched the literature for reported cases of congenital Eikenella sepsis with positive blood cultures at birth. We describe the fourth case.
2. CASE
A 30 year-old woman, gravida II para I, was admitted at 33 weeks and 2 days gestation for preterm labor. On the day of delivery, the mother was afebrile, although she had an elevated white blood cell count of 19,900/mm3. The mother was otherwise healthy and had received prenatal care throughout her pregnancy. Prenatal testing was negative for human immunodeficiency virus, hepatitis B virus, rubella, and syphilis. The mother denied periodontal disease or any history of a human bite. For a living, she trained German Shepherds, but denied any bites or wounds from the dogs. She also denied any oral-genital contact, dental work, or drug use during her pregnancy.
Rupture of membranes occurred at delivery, and a male infant was born vaginally. The delivery was complicated by cord prolapse. The amniotic fluid and placenta were not grossly inflammatory, however maternal blood and placental cultures were not sent, and the placenta was not examined histologically. Other than the increased white blood cell count, the mother had no signs of infection and was not treated with antibiotics.
After delivery, the infant showed signs of respiratory distress and was given a dose of surfactant. The infant weighed 1395 grams, with Apgar scores of 5, 8, and 9 at 1, 5, and 10 minutes respectively. His heart rate at birth was 80 beats per minute, which increased to 120 beats per minute after respiratory support via bag valve mask. His temperature was 36.7˚C rectal and his blood pressure was 61/31 mmHg. He was subsequently placed on continuous positive airway pressure and intravenous (IV) fluids. The infant was initially started on IV ampicillin and gentamicin. When preliminary culture results showed gram-negative rods, cefotaxime was addedon day of life (DOL) 2 for double gram-negative coverage. A chest x-ray demonstrated diffuse haziness but no focal infiltrate. On DOL 1, his white blood cell count was 2990/mm3. His differential showed 12% neutrophils, 1% bands, 47% lymphocytes, 31% monocytes, and 2% eosinophils. He was neutropenic with an absolute neutrophil count (ANC) of 388. His lumbar puncture was traumatic with 3 white blood cells/mm3, 6100 red blood cells/mm3, glucose 36 mg/dl, and protein 210 mg/dl. The cerebrospinal fluid culture was negative.
Blood cultures obtained at 30 minutes of life eventually grew E. corrodens and coryneform gram-positive rods. E. corrodens was reported as susceptible to trimethoprimsulfamethoxazole and ceftriaxone. Repeat blood cultures were negative. The infant’s white blood cell count increased over the next few days, peaking at 28,000/mm3 with an ANC of 11,700 on DOL 5. He maintained a normal core body temperature during the duration of his hospital stay.
The infant improved clinically on antimicrobial therapy. By DOL 4, he was weaned from continuous positive airway pressure to high flow nasal cannula without complications. By DOL 13 he was weaned to room air. He received nasogastric tube feeds during the first four weeks of life due to oxygen desaturation while breastfeeding. He showed no evidence of brain abscess or other lesions on head ultrasound. Repeated surveillance cultures of his nasopharynx, skin, and rectum were negative for Methicillin Resistant Staphylococcus aureus (MRSA), Vancomycin Resistant Enterococcus (VRE)and Serratia and Pseudomonal species. Cefotaxime was discontinued on DOL 5. He otherwise completed a 10- day course of gentamicin and 14-day course of ampicillin. As the positive blood cultures were obtained at 30 minutes of life, it is most likely that the infection was acquired in utero.
3. DISCUSSION
Three cases of congenital E. corrodens sepsis with positive blood cultures at birth have previously been described (see Table 1). Two of these cases were associated with extreme prematurity and death of the neonates shortly after birth. Additionally, both cases were associated with maternal risk factors for E. corrodens infection. All three cases involved chorioamnionitis, and only one case resulted in survival.
In their case series, Garnier et al. [3] summarized seven cases of E. corrodens chorioamnionitis. In these cases, the mothers had evidence of infection, such as fever, positive placental and amniotic fluid cultures, and placental histology consistent with chorioamnionitis. Five of these neonates survived, all of whom were given antibiotics at birth. In the case reported by Kostadinov & Pinar [6], twins were born at 23 weeks gestation to a mother with necrotizing chorioamnionitis. One twin survived with antibiotic therapy, while the other died with evidence of sepsis and funisitis.
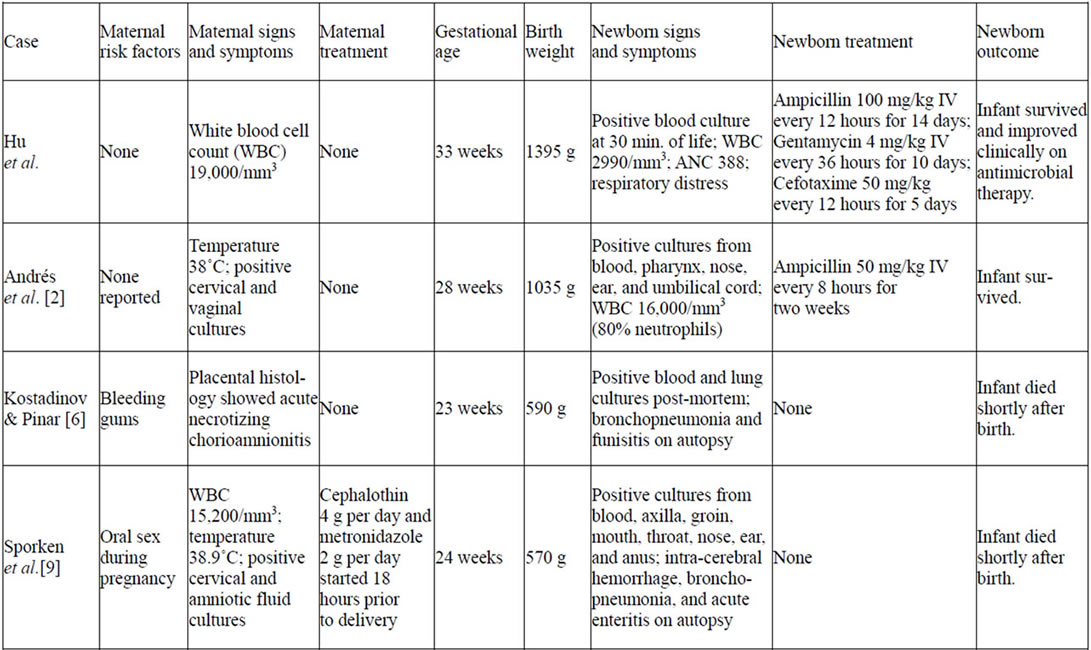
Table 1. Reported cases of congenital sepsis caused by Eikenella corrodens.
Two additional cases of neonatal E. corrodens infection have been described. In 2007, Bueno et al. [7] reported the case of a full-term neonate who presented on DOL 5 with fever and lethargy. He was found to have a positive blood culture and was successfully treated with antibiotics. More recently in 2009, Jadhav et al. [4] reported a case of Eikenella chorioamnionitis associated with frequent oral sex during pregnancy and tongue piercing in both the mother and her partner. Their case suggested ascending vaginal infection and hematogenous spread from tongue piercing as potential routes for E. corrodens intrauterine infection.
We describe a case in which preterm labor associated with congenital E. corrodens sepsis occurred in the absence of overt chorioamnionitis. Allaker et al. [8] found E. corrodens in the dental plaque of 62% of the healthy dogs studied, which may have been a potential risk factor. However, the mother denied any dog bites or injuries. Aside from this, the mother did not have any apparent risk factors for Eikenella bacteremia or ascending infection. Her only sign of possible infection was an elevated white blood cell count. This may have been an indication of early chorioamnionitis, which may explain the route of fetal infection.
Most notably, our case is one of only two reported cases of congenital E. corrodens sepsis associated with survival of the newborn. This is likely related to the fact that two of the prior cases of congenital sepsis occurred at a very early gestational age. However, early recognition and treatment with effective antibiotics should not be underemphasized. In the case reported by Sporken et al. [9], the mother received a first-generation cephalosporin and metronidazole prior to delivery, which were not effective against E. corrodens. Her cultures grew a strain of Eikenella that was susceptible to most other antibiotics. In the case described by Andrés et al. [2], the newborn was treated appropriately with ampicillin beginning on day 1 of life. The infant in their case survived.
In our case, a high index of suspicion for infection as the cause of preterm delivery led to the finding of bacteremia caused by an unexpected pathogen. This demonstrates that E. corrodens, while an uncommon cause of materno-fetal infection, may cause congenital sepsis and preterm delivery in the absence of clinical maternal infection. The infant in our case survived secondary to increased gestational age, probable early onset of chorioamnionitis, and the prompt administration of appropriate antibiotics.
REFERENCES
- Paul, K. and Patel, S.S. (2001) Eikenella corrodens infections in children and adolescents: Case reports and review of the literature. Clinical InfectiousDiseases, 33, 54-61. doi:10.1086/320883
- Andrés, M.T., Martín, M.C., Fierro, J.F. and Méndez, F.J. (2002) Chorioamnionitis and neonatal septicaemia caused by Eikenella corrodens. Journal of Infection, 44, 133-134. doi:10.1053/jinf.2001.0871
- Garnier, F., Masson, G., Bedu, A., Masson, P., Decroisette, E., et al. (2009) Maternofetal infections due to Eikenella corrodens. Journal of Medical Microbiology, 58, 273-275. doi:10.1099/jmm.0.002568-0
- Jadhav, A.R., Belfort, M.A. and Dildy, G.A. (2009) Eikenella corrodens chorioamnionitis: Modes of infection? American Journal of Obstetrics & Gynecology, 200, 4-5. doi:10.1016/j.ajog.2008.10.053
- Stoll, B.J., Hansen, N., Fanaroff, A.A., Wright, L.L., Carlo, W.A., et al. (2002) Changes in pathogens causing early-onset sepsis in very-low-birth-weight infants. New England Journal of Medicine, 347, 240-247. doi:10.1056/NEJMoa012657
- Kostadinov, S. and Pinar, H. (2005) Amniotic fluid infection syndrome and neonatal mortality caused by Eikenella corrodens. Pediatric and Developmental Pathology, 8, 489-492. doi:10.1007/s10024-005-0010-2
- Bueno, E.C., Romero Gomez, M.P., Saez Nieto, J.A., Teres, F.O., Segura, S.A. and Garcia, P.P. (2007) Sepsis neonatal por Eikenella corrodens. Anales de Pediatría, 67, 603-604.
- Allaker, R.P., Langlois, T. and Hardie, J.M. (1994) Prevalence of Eikenella corrodens and Actinobacillus actinomycetemcomitans in the dental plaque of dogs. Veterinary Record, 134, 519-520. doi:10.1136/vr.134.20.519
- Sporken, J.M., Muytjens, H.L. and Vemer, H.M. (1985) Intra-uterine infection due to Eikenella corrodens. Acta Obstetricia et Gynecologica Scandinavica, 64, 683-684. doi:10.3109/00016348509158216

