Open Journal of Preventive Medicine
Vol.3 No.2(2013), Article ID:30674,9 pages DOI:10.4236/ojpm.2013.32031
Physiotherapist-led home-based physical activity program versus community group exercise for middle-aged adults: Quasi-experimental comparison
![]()
1Faculty of Health, University of Canberra, Bruce, Australia; *Corresponding Author: Nicole.Freene@canberra.edu.au
2Physiotherapy, Faculty of Health, University of Canberra, Bruce, Australia
3Centre for Research & Action in Public Health, Faculty of Health, University of Canberra, Bruce, Australia
Copyright © 2013 Nicole Freene et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 18 January 2013; revised 15 March 2013; accepted 16 April 2013
Keywords: Physiotherapy; Home-based; Physical activity; Adoption; Adherence; Middle-aged
ABSTRACT
Objectives: Program method, program deliverer and participant preference may be important factors in increasing physical activity adherence and program effectiveness. To investigate this, we compared two physical activity interventions in middle-aged adults. Methods: Using a pragmatic quasi-experimental design, sedentary community dwelling 50 - 65 year olds (n = 2105) were recruited to a non-randomized 6-month community group exercise program (n = 93) or a physiotherapist-led home-based physical activity program (n = 65). The primary outcome was physical activity adherence derived from exercise diaries. Secondary outcomes included the Active Australia Survey, aerobic capacity (steptest), quality of life (SF-12v2), blood pressure, waist circumference, waist-to-hip ratio (WHR) and body mass index. Results: Home-based participants were more likely to be younger, working full-time and not in a relationship (p < 0.05). Thirty-three percent of the group participants attended ≥ 70% of group exercise sessions. Ninety percent of home-based participants received ≥ 4 of the planned 6 telephone support calls. Intention-to-treat analysis found adherence to the physical activity sessions prescribed was the same for both interventions (26% ± 28% vs. 28% ± 35%). Both interventions significantly increased the number of participants achieving self-reported “sufficient” physical activity (p ≤ 0.001) and significantly decreased waist circumference (p < 0.001) and WHR (p < 0.05). Conclusion: The physiotherapistled home-based physical activity program, requiring few resources, appears to have increased the adoption of physical activity and adherence to physical activity program requirements for sedentary middle-aged adults. The home-based program, providing equivalent health benefits to the group exercise program, may be particularly suitable for those not interested in or unable to attend a group exercise program. Clinical Trial Registration number Australian New Zealand Clinical Trials Registry (ANZCTR), ACTRN126 1000890932.
1. INTRODUCTION
The benefits of physical activity are well documented [1-3] . A number of health promotion strategies have been employed to increase the population’s physical activity levels, including group and home-based physical activity programs [4,5] . Yet few studies have directly compared group and home-based physical activity interventions, particularly over the longer term [6,7] . Fewer studies have investigated the role the physiotherapist plays in physical activity promotion [8] and no studies appear to directly target individuals not interested in group exercise.
There is some evidence that middle-aged adults prefer not to attend group programs. Large surveys in Australia, the USA and the UK report that between 41% - 73% of middle-aged adults (50 - 65 years old) prefer not to attend group sessions [9-11] . Booth [9] found that 73% of insufficiently active (less than 150 minutes per week of moderate-to-vigorous physical activity) Australian adults 40 - 59 years old were not interested in group exercise, increasing to more than 80% for those aged 60 - 78 years old. In contrast, as age increased, there was an increased preference for physical activity advice from a doctor or health professional, with more than 50% of 60 plus year olds preferring advice delivered in this way. A Cochrane review suggests that home-based programs may lead to better long term adherence to exercise compared with centre-based programs [6]. Therefore participant preference, program deliverer and program method are important considerations for physical activity program implementation.
Promoting exercise and physical activity for primary prevention of chronic disease is an area that appears to be under utilised by physiotherapists [8,12] . Physiotherapists are well equipped for this role, routinely prescribing individual exercise programs while taking into consideration a variety of comorbidities [13]. They have a strong background in disease pathologies and body systems, provide a thorough assessment, individually tailored exercise prescription and possess appropriate counselling skills to achieve an increase in physical activity [13,14] . A physiotherapist-led home-based physical activity program may be a suitable delivery option to increase the adoption and long term adherence to physical activity.
The aim of the Physical Activity at Home (PAAH) study was to compare a new, evidence-based model, a physiotherapist-led home-based physical activity program, to a “usual practice” community group exercise program to determine the health benefits, longer term adherence to physical activity and cost-effectiveness. Here we compare the outcomes of the two approaches after 6 months of intervention.
2. METHODS
2.1. Design
Using a pragmatic, quasi-experimental design the physiotherapist-led home-based physical activity program was compared to a non-randomised group exercise program, targeting middle-aged adults not interested in, or unable to attend, a group exercise program. This trial was approved by the University of Canberra Committee for Ethics in Human Research in November 2009 (Project number 09-97).
2.2. Recruitment
Between February and April 2011 two mail outs (n = 3785) were conducted and participants recruited. The Australian Electoral Commission (AEC) federal electoral roll was used to target 50 - 65 year olds in the postcode of an Australian Capital Territory (ACT) YMCA (4 suburbs). To increase the sample size, an additional two suburbs were chosen due to their geographical proximity to the local YMCA. The first letter (n = 2105) asked for expressions of interest in joining a group exercise program at the local YMCA. The second letter (n = 1680) was sent to those not interested in the group exercise program inviting them to participate in a 6 month physiotherapist-led home-based physical activity program or the completion of a number of basic health measures in their homes, “usual care”. Our original study design proposed a randomised controlled trial, allocating eligible home-based participants to a physiotherapist-led homebased physical activity program or usual care [15]. Numbers recruited for the home-based option were insufficient to meet the full original design objectives and the usual care arm was excluded. The flow of participants through the trial is illustrated in Figure 1.
2.3. Participants
All individuals who responded to the mail outs were contacted by telephone by the principal researcher to determine their eligibility. Participants were between 50 - 65 years old and were sedentary, that is, did not participate in regular moderate or vigorous exercise or physical activity for 30 minutes two or more times a week for at least 6 months [16]. They had no serious medical conditions that could limit participation in moderate physical activity, such as unstable angina, uncontrolled hypertension, diagnosed or hospitalized with chest pain, heart attack or heart surgery in the past 6 months and no severe functional impairments due to multiple medical or psychiatric conditions. They were not planning to move from the area within 2 years and only one person per household was eligible. Participants were English speaking and had appropriate cognitive skills to provide informed consent and actively engage in the physical activity program. Medical clearance screening was undertaken using the Sports Medicine Australia (SMA) Pre-Exercise Screening System [17].
2.4. Interventions
2.4.1. Physiotherapist-Led Home-Based Physical Activity Program
Assessments were conducted in participant’s homes. After baseline measures were completed motivational interviewing was used to devise an individual physical activity program [18] . A physiotherapist discussed type, frequency, intensity, duration, benefits, barriers, goals, self-monitoring and progression of physical activity, aiming to achieve 30 minutes of moderate intensity physical activity most days of the week. Participants were contacted by a physiotherapist via phone providing advice and support 2 weeks after the initial assessment and then monthly over a six month period, a total of approximately 6 phone calls per participant.
2.4.2. Group Exercise Program
Participants attended the local YMCA for their baseline measures. Measures were taken by the same physiotherapist as the home-based interventions. Participants then had a choice of four session times during business hours for the group based exercise program. A YMCA fitness instructor conducted the program at the local YMCA once a week, for 60 minutes, over 6 months. The exercise program involved upper and lower body strengthening exercises, gross motor skill training and aerobic fitness training. The exercise specifics were at the discretion of the YMCA fitness instructor, with no involvement from the physiotherapist, aiming to mimic “usual practice”. Participants were encouraged to increase their physical activity levels outside of the group sessions by the YMCA fitness instructors, aiming to achieve 30 minutes of moderate intensity physical activity most days of the week. An individual home-based exercise program was not specifically designed for this group.
Group participants were unaware that a home-based physical activity program was being conducted. No incentives were provided for either intervention to encourage compliance or adherence.
2.5. Outcome Measures
Physical activity adherence was measured using exercise diaries completed over the 6 month intervention period, a continuous measure. Exercise diaries have been found to be both reliable and valid [19]. Participants were encouraged to record date, type, duration and intensity, using the modified Borg rating of perceived exertion scale (RPE) [20], every time they were physically active. Participants were encouraged to return the diaries in the supplied prepaid envelope at the end of each month.
Average monthly adherence rates were calculated as follows: number of physical activity sessions reported as a percentage of physical activity sessions prescribed for the month [21]. The number of sessions prescribed for the month was based on the World Health Organisation (WHO) physical activity guidelines [3]. That is, 30 minutes of moderate intensity physical activity, five or more days per week, a total of 20 or more sessions per month. Moderate intensity was defined as a rating of 3 or more on the modified Borg RPE scale [22].
The Active Australia Survey (AAS) has been designed to measure participation in leisure time physical activity and to assess the participant’s knowledge of current public health messages about the health benefits of physical activity. It applies to one week preceding the interview, including walking for transport, and has been reported as reliable and valid [23,24] . The SF-12v2 is a general health status questionnaire which has a 12-item scale producing eight separate sub-scales and two component scores, physical and mental, to assess quality of life [25]. Both the SF-12v2 and the AAS were self-administered.
The 2-minute step-test (2-MST) assesses aerobic capacity, requires little space and equipment, with large studies finding it both reliable and valid [26]. Waist circumference and hip circumference were measured in centimetres using a tape measure. Resting blood pressure levels were obtained using a mercury sphygmomanometer on the right arm of seated subjects. Waist circumference, hip circumference and blood pressure were taken twice and then the average was recorded. Body mass index (kg/m2) was calculated using a portable set of scales and a stadiometer.
Sociodemographic information was also collected with questions regarding participant’s education level, relationship status, current employment status and the presence of any chronic diseases.
2.6. Data Analysis
For data that were normally distributed, independent samples t-test (2 tailed) with a 95% confidence interval was used to assess differences between interventions at baseline. Chi-square analyses were performed to determine if there were significant differences in distribution of categorical data between interventions at baseline and 6 months. Where cells had counts of less than 5, Fishers exact test was used.
Final analyses at 6 months used an intention-to-treat approach. For missing data at 6 months, we assumed no change from baseline. A one-way repeated measures analysis of covariance (ANCOVA) with a 95% confidence interval was used to determine differences within and between interventions for data that were normally distributed, controlling for age (years), relationship and employment status. McNemar and the Wilcoxon signedranks test were used to determine differences within interventions for categorical data. Significance level was set at p < 0.05. All data were analysed using SPSS version 19.0.
3. RESULTS
3.1. Recruitment
158 participants were recruited, 93 group (G) and 65 home-based (HB). The initial mail out inviting 2105 participants to take part in a group exercise program resulted in 422 replies, a 20% (95% confidence interval (CI): 18 to 22%) response rate. The second mail out sent to those not interested in the group exercise program (n = 1680), invited participants to take part in the home-based program. Sixty-seven replies were received, a response rate of 4% (95% CI: 3% to 5%).
The flow of participants through the trial to date is illustrated in Figure 1. Attempts were made to contact all participants (n = 422) interested in the group exercise program. The majority (n = 333) were screened for eligibility. Twenty-six percent (95% CI: 21% to 31%) were unable to attend the group program due to unsuitable session times. Most of these participants were then offered the home-based program, with 53 participants expressing interest.
Some of the participants interested in the group program that were unable to be contacted during the group recruitment phase were invited to take part in the home-based program with 34 showing interest. In total, 154 participants were interested in the home-based intervention. The main reasons for exclusion for both interventions are outlined in Figure 1.
The recruitment rates for the physical activity programs were similar. The home-based program recruited 3.6% (95% CI: 2.8% to 4.5%) of the invited population (65/1781) compared with 4.4% (95% CI: 3.5% to 5.3%) recruited for the group exercise program (93/2105). The recruitment of 93 participants for the group exercise program may be a slight underestimate as recruitment for
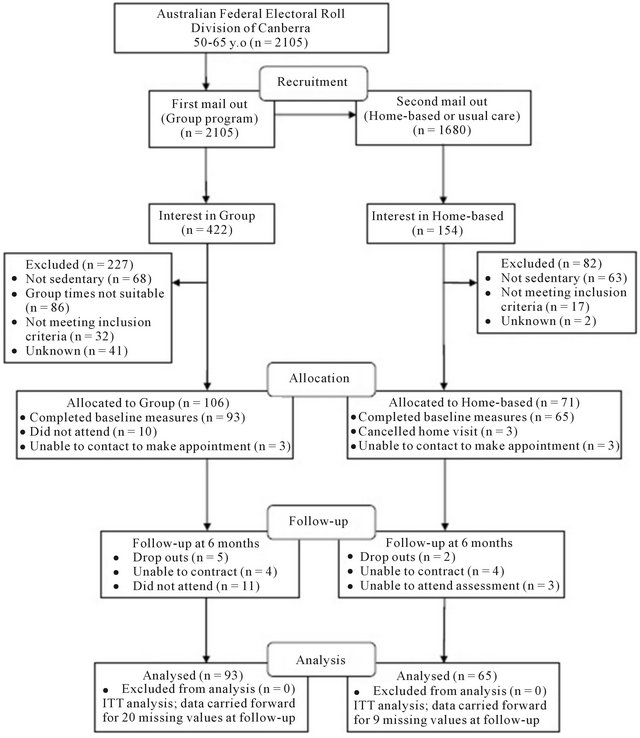
Figure 1. Flow of participants through the trial.
this intervention was limited by time constraints. The physiotherapist-led home-based physical activity program increased the total number of sedentary middle-aged adults recruited to a physical activity intervention by 82% (95% CI: 34% to 129%).
3.2. Baseline Characteristics
The home-based participants were more likely to be younger (56 vs. 59 years, p = 0.001, t = 3.306, 95% CI: 1.04 to 4.12), employed full-time (63% vs. 27%, p < 0.001, X2(2) = 21.4) and not in a relationship (41% vs. 24%, p = 0.02, X2(1) = 5.10). There were no other significant differences between interventions for all remaining outcome measures (Tables 1 and 2). The majority of participants were female (72%), tertiary educated (65%), with no history of chronic disease (73%).
3.3. Physical Activity Adherence
Self-reported adherence to the physical activity recommendations was limited due to the poor exercise diary
Table 1. Comparison of baseline and 6-month follow-up by intervention.
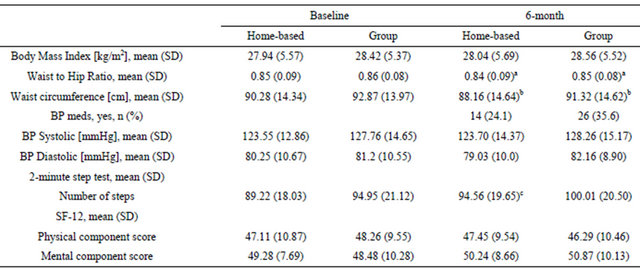
aPaired comparison repeated measures ANCOVA (baseline versus 6-month follow-up) within intervention, p < 0.05; bPaired comparison repeated measures ANCOVA (baseline versus 6-month follow-up) within intervention, p < 0.001; c6 month comparison repeated measures ANCOVA between interventions, p < 0.05.
Table 2. Physical activity characteristics at baseline and 6-month by intervention.

aPaired comparison Wilcoxon signed rank test (baseline versus 6-month follow-up) within intervention, p ≤ 0.001; b6-month comparison Chi-square analysis between interventions, p < 0.05.
return rate (Figure 2). Using an intention-to-treat analysis, assuming no adherence among non-responders, no significant difference was found between interventions for physical activity adherence to the sessions prescribed, F(1,150) = 0.35, p = 0.56 (26% ± 28% HB vs. 28% ± 35% G), nor was there any significant difference within interventions.
Using the AAS, both the home-based and group interventions significantly increased the number of participants achieving “sufficient” physical activity over the 6 month intervention period (HB 22 vs. 45%, Z = −3.43, p = 0.001; G 22 vs. 52%, Z = −4.91, p < 0.001), although there was no difference between interventions (Table 2). Home-based participants also became more aware that they could accumulate physical activity in 10 minute blocks (HB 81% vs. G 66%, X2(1) = 3.95, p = 0.047; HB p = 0.001) (Table 2).
3.4. Program Adherence
Ninety percent of home-based participants received ≥ 4 of the planned 6 telephone support calls, with mean call length 4.5 minutes. Approximately 2 phone call attempts (mean, 1.8 attempts) per participant per month were required before they were reached. Thirty-three percent of the group participants attended ≥70% of group exercise sessions.
3.5. Outcomes at 6 Months
Both interventions significantly decreased waist circumference (F(1,156) = 44.20, p < 0.001) and waist-to-hip ratio (WHR) (F(1,152) = 4.53, p = 0.04) over the intervention period with no difference between interventions (Table 1).
There was a significant difference between interventions for the 2-MST number of steps (F(1,140) = 5.52, p =

Figure 2. Exercise diary monthly physical activity adherence rates by intervention (mean, 95% CI); home-based (dashed line), group exercise (solid line). Inset Table shows number of diaries returned by month.
0.02) with group participant’s having a higher mean number of steps at baseline and 6-months (Table 1). Age (years) had a significant effect (F(1,140) = 10.53, p = 0.001) on the number of steps completed in the 2-MST, with steps decreasing as age increased. There was no significant difference for 2-MST number of steps within both the group and home-based interventions over the 6 month period (Table 1).
No physical activity-related cardiac events occurred for either intervention. Physical activity noncardiac events, including strains, sprains and fractures, were very few, similar across interventions.
4. DISCUSSION
The physiotherapist-led home-based physical activity program, requiring few resources, appears to have increased the adoption of physical activity and adherence to physical activity program requirements for sedentary middle-aged adults. The home-based program, providing equivalent health outcomes to the group exercise program, may be particularly suitable for those not interested in or unable to attend a group exercise program.
There is some evidence that a large number of community dwelling middle-aged adults may not be interested in group exercise but would undertake exercise on their own if they had access to appropriate exercise information and or supports [10]. Yet, results from this study do not support this with a low response rate (≤4%) to the second mail out offering the home-based intervention. Participants in this study were not given a choice initially whether they would like to take part in a group or home-based intervention, potentially reducing numbers interested in the home-based intervention.
Once recruited, adherence to the physical activity program requirements is an important factor for physical activity adoption. The home-based intervention appears to be superior in maintaining this adherence. This agrees with two Cochrane reviews comparing home-based and centre-based programs for increasing physical activity and cardiac rehabilitation [6,27] . Similarities also exist between adherence to the group program requirements in this study and other studies, which show that approximately 35% - 50% of the general population who start an exercise program stop within the first 6 months [28,29] .
Despite the differences in program adherence both interventions increased the number of participants achieving “sufficient” physical activity levels. This is valuable as there are well established links between an increase in physical activity and the health benefits [1]. The reduction in waist circumference and waist-to-hip ratio reflects this, measuring changes in central obesity, a known risk factor for chronic disease [30,31]. Importantly, it was found that the home-based program, requiring few resources, was just as effective as the group exercise program in producing these health benefits. This requires consideration in terms of possible cost-effectiveness, for both program provision and health utilisation costs.
Increased physical activity awareness may lead to an increased adherence to the physical activity guidelines over the longer term. At the end of the intervention period, home-based participants were more aware that physical activity could be accumulated in 10 minute blocks when compared to group exercise participants. Motivational interviewing used by the physiotherapist in this study may be an important factor in increasing this awareness and possibly increasing long term physical activity adherence, requiring further investigation [9].
Using intention-to-treat analysis, adherence to the physical activity sessions prescribed during the intervention period appears to be the same for both interventions. For the actual exercise diaries returned (Figure 2), physical activity adherence increases and then decreases slightly over the 6 month intervention period for both interventions, showing a similar pattern for exercise adherence as reported by King [21]. On average, all participants completed 26% - 28% of the prescribed sessions, which equates to 1 - 2 sessions of ≥30 minutes MVPA per week. Data from the AAS tells us that more participants became “sufficiently” active over the intervention period, with half of all participants completing ≥ 150 minutes MVPA in ≥5 sessions by the end of the intervention period, which does not agree with the exercise diary data. There are a number of limitations to the exercise diary data, including poor return rate, potential over-reporting and the possibility that only those participants that were physically active returned their diaries. Therefore this data should be interpreted cautiously.
The participants recruited for this study were typical of participants that are recruited for studies similar to this, that is, predominantly female and well-educated, creating a gender and education bias [32] . The ACT population has a higher level of education and physical activity as compared to the national average [33,34], and this is reflected in this sample. In terms of socio-economic advantage and disadvantage within the ACT, the suburbs targeted provide a broad cross-section according to the socio-economic index for area (SEIFA). However relative to the rest of Australia, these suburbs would be considered relatively advantaged [35].
One of the strengths of this trial is that the medical and functional inclusion criteria were quite broad proposing that there is some benefit from physical activity for almost everyone. The recruitment method also attempts to minimize self-selection and recruitment of highly motivated volunteers by using the electoral roll [32] . The electoral roll allowed targeting of the suburbs within the same postcode as the community group exercise program, minimising a potential location barrier. Recruitment and providing the home-based intervention by telephone should also limit selection bias as phone coverage is widespread in Australia. Both physical activity programs were provided free of charge, potentially increasing recruitment of eligible participants.
The lack of a randomised control group, “usual care”, to assess the effectiveness of the physiotherapist-led home-based physical activity intervention is a significant limitation. There is some evidence though that there is no difference in outcomes between a randomised control trial and a patient preference trial when comparing programs, in studies similar to this one. Dalal [27] found that whether patients were randomly allocated to a home-based or hospital-based cardiac rehabilitation program or they got to choose their type of program, made no difference to the clinical outcomes. The lack of blinding is also a potential cause of bias, as the principal researcher conducted all assessments and provided the home-based intervention.
In conclusion, the home-based physical activity program delivered by a physiotherapist offers potential to increase the recruitment of sedentary middle-aged adults to a physical activity intervention, particularly if they are not interested in, or unable to attend, a community group exercise program. The physiotherapist-led home-based physical activity program, requiring few resources, produced equivalent health benefits to the group exercise program and appears to have a lower attrition rate with an increased adherence to the program requirements.
5. ACKNOWLEDGEMENTS
We are grateful to all the staff at the YMCA Chifley who provided in-kind support in the form of two fitness instructors, administrative support and a venue for four exercise groups once a week for 6 months and group participant assessments. We would like to thank all the women and men who were participants in this trial.Funding for this study was provided by the Faculty of Health, University of Canberra Research Training Scheme.
REFERENCES
- Warburton, D.E.R., Nicol, C.W. and Bredin, S.S.D. (2006) Health benefits of physical activity: The evidence. CMAJ: Canadian Medical Association Journal, 174, 801-809. doi:10.1503/cmaj.051351
- Booth, F.W., Gordon, S.E., Carlson, C.J. and Hamilton, M.T. (2000) Waging war on modern chronic diseases: Primary prevention through exercise biology. Journal of Applied Physiology, 88, 774-787.
- World Health Organization (2004) Global strategy on diet, physical activity and health. World Health Organization, Geneva.
- Muller-Riemenschneider, F., Reinhold, T., Nocon, M. and Willich, S.N. (2008) Long-term effectiveness of interventions promoting physical activity: A systematic review. Preventive Medicine, 47, 354-368. doi:10.1016/j.ypmed.2008.07.006
- Hillsdon, M., Foster, C. and Thorogood, M. (2005) Interventions for promoting physical activity. Cochrane Database of Systematic Reviews (Online), 1, Article ID: CD003180.
- Ashworth, N.L., Chad, K.E., Harrison, E.L., Reeder, B.A. and Marshall, S.C. (2005) Home versus center based physical activity programs in older adults. Cochrane Database of Systematic Reviews (Online), 1, Article ID: CD004017.
- Van der Bij, A.K., Laurant, M.G. and Wensing, M. (2002) Effectiveness of physical activity interventions for older adults: A review. American Journal of Preventive Medicine, 22, 120-133. doi:10.1016/S0749-3797(01)00413-5
- Shirley, D., Van der Ploeg, H.P. and Bauman, A.E. (2010) Physical activity promotion in the physical therapy setting: Perspectives from practitioners and students. Physical Therapy, 90, 1311-1322. doi:10.2522/ptj.20090383
- Booth, M.L., Bauman, A. Owen, N. and Gore, C.J. (1997) Physical activity preferences, preferred sources of assistance, and perceived barriers to increased activity among physically inactive Australians. Preventive Medicine, 26, 131-137. doi:10.1006/pmed.1996.9982
- Wilcox, S., King, A.C., Brassington, G.S. and Ahn, D.K. (1999) Physical activity preferences of middle-aged and older adults: A community analysis. Journal of Aging & Physical Activity, 7, 386-399.
- Yardley, L., Kirby, S. Ben-Shlomo, Y., et al. (2008) How likely are older people to take up different falls prevention activities? Preventive Medicine, 47, 554-558. doi:10.1016/j.ypmed.2008.09.001
- Sheedy, J., Smith, B., Bauman, A., et al. (2000) A controlled trial of behavioural education to promote exercise among physiotherapy outpatients. Australian Journal of Physiotherapy, 46, 281-289.
- Australian Physiotherapy Association (2009) Position Statement: Chronic disease and physiotherapy. http://www.physiotherapy.asn.au/policy-and-communications/position-statements
- O’Donoghue, G. and Dean, E. (2010) The physiotherapist’s role in contemporary health care in Ireland: Responding to 21st century indicators and priorities. Physiotherapy Ireland, 31, 4-9.
- Freene, N., Waddington, G., Chesworth, W., Davey, R. and Goss, J. (2011) “Physical Activity at Home (PAAH)”, evaluation of a group versus home based physical activity program in community dwelling middle aged adults: Rationale and study design. BMC Public Health, 11, 883. doi:10.1186/1471-2458-11-883
- Wilbur, J., McDevitt, J.H., Wang, E., et al. (2008) Outcomes of a home-based walking program for AfricanAmerican women. American Journal of Health Promotion, 22, 307-317. doi:10.4278/ajhp.22.5.307
- Department of Health and Aging, Australia Government (2005) Sports Medicine Australia (SMA) Pre-exercise screening system 2005. http://sma.org.au/wp-content/uploads/2009/05/new_pre_screening.pdf
- Thompson, D.R., Chair, S.Y., Chan, S.W., et al. (2011) Motivational interviewing: A useful approach to improving cardiovascular health? Journal of Clinical Nursing, 20, 1236-1244. doi:10.1111/j.1365-2702.2010.03558.x
- Duncan, K.A. and Pozehl, B. (2002) Staying on course: The effects of an adherence facilitation intervention on home exercise participation. Progress in Cardiovascular Nursing, 17, 59. doi:10.1111/j.0889-7204.2002.01229.x
- Borg, G.A.V. (1982) Psychophysical bases of perceived exertion. Medicine & Science in Sports & Exercise, 14, 377-381. doi:10.1249/00005768-198205000-00012
- King, A.C., Haskell, W.L., Young, D.R., Oka, R.K. and Stefanick, M.L. (1995) Long-term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation, 91, 2596-2604. doi:10.1161/01.CIR.91.10.2596
- Norton, K., Norton, L. and Sadgrove, D. (2010) Position statement on physical activity and exercise intensity terminology. Journal of Science and Medicine in Sport, 13, 469-502.
- Brown, W.J., Trost, S.G., Bauman, A., Mummery, K. and Owen, N. (2004) Test-retest reliability of four physical activity measures used in population surveys. Journal of Science and Medicine in Sport, 7, 205-215. doi:10.1016/S1440-2440(04)80010-0
- Brown, W.J., Burton, N.W., Marshall, A.L. and Miller, Y.D. (2008) Reliability and validity of a modified selfadministered version of the Active Australia physical activity survey in a sample of mid-age women. Australian and New Zealand Journal of Public Health, 32, 535-541. doi:10.1111/j.1753-6405.2008.00305.x
- Ware Jr., J., Kosinski, M. and Keller, S.D. (1996) A 12- item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Medical Care, 34, 220-233. doi:10.1097/00005650-199603000-00003
- Rikli, R.E. and Jones, C.J. (1999) Development and validation of a functional fitness test for community-residing older adults. Journal of Aging & Physical Activity, 7, 129-161.
- Dalal, H.M., Evans, P.H., Campbell, J.L., et al. (2007) Home-based versus hospital-based rehabilitation after myocardial infarction: A randomized trial with preference arms—Cornwall Heart Attack Rehabilitation Management Study (CHARMS). International Journal of Cardiology, 119, 202-211. doi:10.1016/j.ijcard.2006.11.018
- Jancey, J., Lee, A., Howat, P., et al. (2007) Reducing attrition in physical activity programs for older adults. Journal of Aging & Physical Activity, 15, 152-165.
- Hong, S.Y., Hughes, S. and Prohaska, T. (2008) Factors affecting exercise attendance and completion in sedentary older adults: A meta-analytic approach. Journal of Physical Activity & Health, 5, 385-397.
- National Health & Medical Research Council (2004) Clinical practice guidelines for the management of overweight and obesity in adults 2004. Department of Health and Ageing, Australian Government, Canberra, 48.
- World Health Organization (2008) Waist circumference and waist-hip ratio. Report of a WHO expert consultation. World Health Organization, Geneva.
- Jancey, J., Howat, P., Lee, A., et al. (2006) Effective recruitment and retention of older adults in physical activity research: PALS study. Perth Active Living Seniors Project (PALS). American Journal of Health Behavior, 30, 626-635. doi:10.5993/AJHB.30.6.9
- Office of the Chief Health Officer (2010) Australian Capital Territory Chief Health Officer’s Report 2010. ACT Health, Communications and Marketing Unit, Canberra.
- Australian Bureau of Statistics (2006) Physical activity in Australia: A snapshot, 2004-05. Australian Bureau of Statistics, Canberra.
- Australian Bureau of Statistics (2008) Census of population and housing: Socio-Economic Indexes for Areas (SEIFA), Australia—Data only 2006 (cat. no. 2033.0.55.001). Australian Bureau of Statistics, Canberra.

