Health
Vol.09 No.03(2017), Article ID:74890,22 pages
10.4236/health.2017.93038
Illness Experience in a Very Low Income/Poor District of Rio de Janeiro, Brazil: Tuberculosis, Medication Adherence and Common Mental Disorders
Gisele O’Dwyer1*, Valéria Lino1, Nádia Rodrigues1, Monica Kramer1, Ines Reis1, Vera Frossard1, Eliane Vianna1, Lucília Elias1, Carlos Eduardo Estellita-Lins2
1National School of Public Health, Rio de Janeiro, Brazil
2Institute of Scientific and Technological Communication and Information in Health, Rio de Janeiro, Brazil

Copyright © 2017 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: February 10, 2017; Accepted: March 21, 2017; Published: March 24, 2017
ABSTRACT
Introduction: Tuberculosis is a global health problem. Improving medication adherence is an important attribute concerning the outcome of tuberculosis treatment. This study investigates illness experience of patients belonging to a low-income district within Manguinhos catchment area. Narrative studies are able to unfold features concerning patient adherence and co-occurrence of de- pressive symptoms. Methods: Twenty-three patients under treatment were interviewed using McGill Illness Narrative Interview (MINI-McGILL), besides depression screening with “Self-Report Questionnaire-20” (SRQ-20) and “Beck Depression Inventory” (BDI). Results: Explanatory models disregarded airborne microorganism contagion, known but not considered relevant while bohemian or deviant lifestyle was rather perceived as a causal model. Patients mentioned contiguous events suggesting pneumonia or influenza misdiagnosis before final tuberculosis diagnosis (testing or suspicion). Therapeutic path- ways were erratic, suggesting low literacy level and postponed or inadequate diagnosis accuracy. Emergency units or private services usually stood for primary care units considered first choice by planners. Expressions such as “dreadful/shameful disease” or “very heavy illness” acknowledged stigma. Research data detected the importance of social network role, highlighting the family through financial and affective support. Hopelessness and depression were closely related to illness suffering and adversities. The percentage of patients for positive common mental disorder and depression approaches 30%. Conclusion: Tuberculosis remains a stigmatizing disease. Building effective health services networks, comprising treatment facilities, community and fa- mily resources are very important to improve medication adherence. Effective tuberculosis management through health teams training seems necessary. Incorporating simple screening instruments for depression assessment might pro- mote well-being and patient adherence.
Keywords:
Tuberculosis, Patient Adherence, Depression, Common Mental Disorders, Primary Health Care, Social Support, Health Sevices Accessibility

1. Introduction
Tuberculosis (TB) is a global health problem. Along with acquired immunodeficiency syndrome (AIDS), it makes up one of the leading causes of death around the world. Despite the advances in diagnosis and treatment, the possibility of cure in almost all cases of TB remains one of the greatest global threats. The non-adherence to the ant tuberculosis therapy (NAATT) makes up one of the main barriers to fight against this disease [1] .
The adherence to long-term treatments is a worldwide problem of striking magnitude. In developed countries, non-adherence occurs in 50% of cases, with even higher percentage in poor ones. Without a system to identify the determinants of this kind of behavior, advances in biomedical technology will fail to reduce the burden of chronic diseases. Access to therapy is necessary, but insufficient for successful treatment [2] .
In relation to TB, many factors influence the NAATT and they are related to: 1) individual and sociodemographic characteristics, such as social support, knowledge and beliefs about illness and treatment; 2) the health system, like the structure of services that involve the delivery process, coordination among the health services and professional training; and 3) the pharmacological therapy, as the duration of treatment, toxicity, cost and dosage of drugs [2] [3] [4] . Economic aspects are also important. Poor, unemployed and homeless individuals are hard to find and this constitutes another barrier to the adherence. Despite these multiple causes of NAATT, it is common to assign patients the responsibility for the treatment adherence and abandonment [5] . The non-adherence contributes to the worsening of the patient’s health, the drug resistance, the spread of the disease and an increase in the cost of treatment.
Changes in mental status such as drug use, depression, anxiety, and emotional stress also contribute to the NAATT [2] . The association of depression to tuberculosis also has been investigated in other countries. In Manila, Philippines, 17% of 561 patients under directly observed treatment in 12 public services suffered from depression [6] . In a tertiary care hospital, in India, 84% out of the 147 patients presented depressive symptoms over a period of 15 months of observation [7] . Moderate to severe levels of depression and anxiety was present in 72% of 65 patients examined in a primary care unit in Pakistan over three months [8] . In Taiwan, China, a National Health System retrospective cohort study with 9020 individuals with newly diagnosed tuberculosis evidenced that the risk of depression was 1.5 times higher in these patients [9] . Ugarte-Gil et al. examined the influence of depression on abandonment of the treatment or death. The risk for these two occurrences was 3.5 times higher in depressed groups compared to those without mood disorder [10] .
The literature about proposals for intervention to promote adherence to the treatment reveals no consensus on the most effective strategy. A qualitative stu- dy performed in Rio de Janeiro, Brazil, concluded that adherence-promoting strategies in the treatment of TB should include links and interpersonal care between professionals, families and sick individuals [11] . Volmink and Garner suggest interventions aimed at reducing social barriers, especially for patients in situations of greater vulnerability. These patients should be under more coercive approaches that do not promote the autonomy of individuals [12] . Considering the cultural context and specific populations, it is fundamental to create strategies appropriate to local realities.
Kleinman and Good have investigated the health-disease-care and coined the concept of experience of illness [13] , highlighting the importance of personal experiences in this process [14] . The notion of experience of illness involves both the way in which individuals perceive and assign meaning, as the therapeutic itinerary, that is, the ways and steps by which they find solutions to deal daily with their current condition. Knowing the difficulties encountered in the therapeutic itinerary, the mental disorders associated with the disease and the type of social support for the patients, can lead to the elaboration of strategies to increase the adherence to the treatment. The objectives of this study were to know the illness experience of patients with TB, to identify the factors associated to the NAATT from patients’ point of view and to examine the relationship between depressive symptoms and adherence to anti-TB treatment.
2. Methodology
This is a qualitative study performed at the primary care unit of the Oswaldo Cruz Foundation, in the city of Rio de Janeiro, Brazil. This unit provides services to 43,000 residents of the Manguinhos District, where sanitary issues are still unsolved, most houses have a single room, and monthly family income is usually lower than the minimum wage. The inclusion criteria of the study were: to be over 18 years of age, have been living and receiving care in the district of Manguinhos by the local family health professionals, diagnosed with TB or being treated in the year 2013. The sample was constructed by recruiting subjects using the drug dispensing records from the pharmacy. All eligible individuals were contacted, both adherents and non-adherents to treatment. The expected was a sample of 40 - 50 subjects. The flow of patient recruitment for interviews and participation in the study occurred in three different ways: a) through the approach of patients with TB with consultation previously scheduled in the routine of the service; b) by telephone contact, after identification of TB cases; c) by means of an invitation letter delivered at the home of patients diagnosed with TB.
Participants were interviewed throughout the year 2013 and 2014 with the Portuguese version of the “McGill Interview of Illness” (MINI) [15] and two instruments for identification of common mental disorders and depression, the Self-Report Questionnaire-20 (SRQ-20) [16] and the Beck Depression Inventory (BDI) [17] respectively. The interviews lasted 60 to 90 minutes and, at the end of it, participants received a basket with basic food items.
Data Analysis
We used the thematic content analysis technique to analyze the text. Fluctuating and deepening readings by the researchers led to the definition of cores of senses and to the identification of the six thematic categories listed below. To identify the presence of common mental disorders from the BDI and the SQR-20, the following cut-off points were used: <10 vs. ≥10 and <8 vs. ≥8 points, respectively [16] [17] .
The study kept the anonymity of the participants using identification code numbers ranging from 1 to 23, prefixed by the letter “P” was used to differentiate the respondents. It was obtained written informed consent from participants. The Ethics and Research Committee of the National School of Public Health approved it in 2013 under the n˚ 1691.7813.3.0000.5240.
3. Results and Discussion
Twenty-three patients with TB were interviewed. Thirteen out of the twenty-three patients were females (Table 1). This preponderance of women differs from the profile normally assigned to TB but it can be an at random finding. In 2013, 62 cases of TB were diagnosed by the local family health professionals and in 2014, 46 cases. The incidence rate of TB in Mangunhos was 2185/100,000 in 2013 and 2212/100,000 in 2014. The local mortality was 36/100,00 in 2013 and 22/100,00 in 2014.
The six thematic categories identified in the analysis were: 1) Stigma; 2) Information and Communication; 3) Causes of TB; 4) Therapeutic Itinerary and Treatment; 5) Social Support; 6) Impact on Life.
Table 1. Distribution of socio demographic characteristics in the study population.
3.1. Stigma
Tuberculosis was labeled by respondents as being “awful”, “heavy” and “that”. This phenomenon has been described in the literature as an attempt to disguise the designation of the disease due to the fear that if speaking out the real name of the disease, it would “attract evil to you” [18] . In the nineteenth and twentieth centuries, TB acquired a romantic connotation when portrayed by poets and artists but the aspects associated with the its spread, contagion, and lethality associated it with death. It was not long before the disease became a taboo with stigma and consequent isolation of the patient [18] .
The concept of Stigmata according to Goffman is the “process or the status of the individual who is disabled for full social conviviality” [19] . This happens when individuals have some attribute or deviant characteristics for their time. Until nowadays, the negative aspects of TB and the stigmatization of the patient are the most persistent features of TB in different countries and cultures [20] [21] . On the other hand, recent study in Sao Paulo, Brazil, showed that not all the 110 subjects recruited for the study were ashamed to talk to their families about the disease and 60% of them talked openly about the disease. It is important to note that the less stigma associated with the diseases resulted in higher knowledge and access to information [22] .
Several testimonials have expressed fear of death, rejection and abandonment due to the disease’s severity. Psychologists, anthropologists, and sociologists have observed the “nuisance” when speaking of the disease mainly in poorer communities [23] . The stigma surrounding the disease and consequent social isolation can lead to anxiety and depression. The next talk illustrates the association between social isolation and depression:
“I was thinking of killing myself. My husband did not let me do it. I picked up a bunch of pills to take, he did not let me, and neither God did. It was very difficult. Being rejected by the people, by friends, by family, by everyone. I wish they (family) came to see me, but nobody came. The only person who showed up, I asked a lot to God was my brother.” P. 19 “Some people stopped to talk.” P. 13 “Some people drifted away in disgust.” P. 15 “The People of the street judge me much, avoid me.” P. 16
The Brazilian Government’s campaigns disclose the association between TB to HIV and the two national control programs request testing for HIV infection in all patients with TB and vice versa, as the early diagnosis can improve the prognosis of both of them [24] . Although well intentioned, this strategy increases the feelings of social isolation, depression and rejection of some individuals. In many cases both the diagnosis of TB and HIV infections are given at the same time. In Manguinhos, the prevalence rate of co-infection is above 10% (data collected in the service itself). The narratives below illustrate the problem:
“It is a disease just like HIV, people is not aware, there’s a lot of prejudice and ignorance.” P. 1 “I didn’t even talk to anyone due to the fear of prejudice. HIV and tuberculosis are the worst diseases that exist.” P. 6
In the study, there were also reports of stigma associated with suffering within the health service. An interviewee alleged to feel like an animal during the consultation at the health service and abandoned the treatment for this reason. After the appropriate reception, she established a relationship of trust and confidentiality with the doctor and remained in treatment, as shown in the following speech:
“I had a lot of excitement with Doctor Celina ... Exciting is to raise your esteem. Some doctors seem to like lowering the esteem, have disgust, don’t put their hands on it when they are going to do a treatment ... end that excitement of you. Next month will I go back there? Then I will find that doc, be treated like an animal. Will I be treated in such a place? The excitement ends, it’s all over.” P. 14
Another patient in the present study with multidrug-resistant to TB demonstrated sorrow, felt judged and disrespected by the doctor who attributed abandonment to treatment as the sole cause of multidrug-resistant TB, although he denied:
“The doctor all the time she punches the same button that the disease came back because I hadn’t take the medicine, but I have the conviction that I took. However, I took, I’m sure about that! But there is not another situation, another condition for which you have multi-drug resistant tuberculosis? So I didn’t agree with her, but also not debated, at the beginning I even struggled with her, she always was emphatic on this point, so I preferred not to argue, it was what she thought, with the experience that she had.” P. 1
The relationship established among peers is fundamental to the development of trust. It is important the professional welcoming posture and greater understanding of their numerous difficulties for the treatment [25] [26] . From the professional point of view, there is an accumulation of functions, lack of preparation when dealing with the patient in addition to precariousness of working links. From the patients ‘point of view, there is difficulty in expressing themselves, situations of transference, emotional and financial instability.
In relation to the multidrug-resistant TB, the most frequent causes are multiple abandonments of treatment and inappropriate treatments. However, the infection by another patient with multidrug-resistant TB [18] , the lack of emotional support, negligence on the part of professionals, and the disorganization of the health services [27] are also reason that contribute to the abandonment. With the implementation of the Family Health Strategy Units, all these problems have been minimized, but there is still a long way to go.
3.2. Communication and Information
The TB disease is an “old acquaintance” of Manguinhos’ population. It is the second most prevalent infectious disease in this territory coming immediately after Dengue fever [28] . Manguinhos presents one of the worst Human Development Indexes of the city of Rio de Janeiro. The incidence rate of TB (above 100/ 100,000 inhabit) [29] reveals the relationship between poverty and social determinants that promote transmission of TB. Therefore, this study demonstrates that the disease is part of the reality of individuals represented by several reports of cases of TB in friends, neighbors and relatives. Four patients had already had an episode of TB. Eleven reported TB in the family with some dramatic experiences. The presence of hemoptysis showed the severity of the disease.
“My sister, I saw her putting blood through her mouth, but I didn’t know what it was, then I saw how she lost weight so fast, my mom took her to the emergency room, she was already fading, and wasn’t holding walk.” P. 19
In the last decade, there has been increase in social mobilization in TB control. The PNCT/Ministry of health has invested in the media as an important outlet for relaying information and dissemination about the disease. The Global Fund Project “Strengthening of the Directly Supervised Treatment Strategy (DOTS) in Large Urban Centers with High Burden of TB in Brazil” financed actions and outreach activities about the disease according to regional specificities of the country. There was a huge production of information material, booklets and posters [30] . In this study, five patients have reported familiarizing themselves with the disease through television or billboards. A singer who participated in the campaigns was quoted a couple of times indicating the effectiveness of campaigns with popular artists. These media resources captured the perception that TB has been healing information. An interviewee immediately identified her symptoms to be probably TB because of a billboard advertisement she saw of her favorite samba singer promoting the need of seeking treatment for TB.
“Then I saw the campaign passing on television. I think that was Thiaguinho talking about it. I thought ... Oh my God ...” P. 18 “For the first time I saw it on Thiaginho poster, that famous singer. There is one poster near the complex with him. Close to Brazil Avenue. It was written: ‘TB has cure’. I was already illness with tuberculosis.” P. 15
Workplace posters were also mentioned, but without specifying, the information conveyed. Only one interviewee remembered having to read about the persistent cough. One of the interviewees said that they only started reading the posters after being affected by the disease. This goes to show the importance of the information being conveyed to targeted audiences.
“Yeah ... It’s like this. Once in a while, you hear about a campaign. I particularly only got acquainting about tuberculosis when I got sick and not before that. I suffer from the evil that 99% of people suffer too. I feel that, the ignorance of people for not knowing the risks, what you can and what you cannot do to avoid it. Only when the people get sick they know what can be done and what can’t.” P. 1
However, it was noted that five people said they did not have any reference about TB from the media. The lack of access to information through the media could be explained by several factors such as the lack of education, low socioeconomic status, and the lack of individual interest [27] .
Another relevant factor for the communication of information on the treatment and risk of contamination arising from doctor-patient relationship is illustrated through the following example:
“Keeps the House well aired, takes plenty of water, eats healthily, take the medicine on an empty stomach always at the same time.” P. 9
As a result of this study, a campaign was conducted on the primary care unit to sensitize professionals and users about the use of mask. These actions have helped to improve the acceptance of this practice in order to reduce the risk of contagion. The service offers masks to anyone with persistent cough, especially for patients with TB. The professionals seek to encourage the use of this in the first few weeks of treatment.
“She saw that I was coughing a lot, she told me to put the mask on. The mask was expendable. Then she said that I was suspected of tuberculosis.” P. 15
The importance of information about TB is critical to overcoming myths, enlarge open conversations on the topic about forms of transmission and how to take care of a person [22] .
3.3. The Causes of Tuberculosis
This category brought together the reasons why respondents attributed causality to their illness. Six main causes were identified by explaining the occurrence of TB and they are: 1) The unruly style of life; 2) The contagion; 3) The pulmonary fragility by handling chemical agents at work; 4) Something unexpected; 5) As a result of magic causes; and 6) The genetic predisposition.
The most cited cause of TB by almost all respondents is an unruly style of life that resulted in sleeping late, consumption of alcohol, smoking, drug use and unhealthy eating habits. The association with exposure to cold temperature was also cited many times: expose to the cold during the early morning hours, ingestion of cold beer, and sleep with wet hair. The recurrent perception that the disease is due to an unruly life style suggests the individual culpability by the illness:
“It was the drinking habit, many nights without sleeping, and the lack of adequate food intake.” P. 21 “I’ve never smoked. I’ve never had alcohol. I have a ruled life. How did I end up in a situation like that? It’s very complicated.” P. 23
Despite the current knowledge about the etiological agent of the disease, previous concepts permeate through time. TB remains a disease that shames an individual and considered worthy of censure and guilt [18] .
Although several reports pointed out the fear of infecting family members, suggesting the occurrence of awareness about an infectious agent, the person-to- person contagion was not always perceived as the primary cause of the disease. Working with chemical agents such as detergents and chlorine, as well as the work of cleaning and contact with dirt, mold and dust was pointed out as causative agents.
Another understanding of causality of TB was regarding to work overload with negative impact on sleep, feeding, and immunity, suggesting the perception that the main causal sense stems from a body weakened, tired, underfed or intoxicated:
“A little bit sloppy about my life, I wasn’t looking for feed when I got home; I was drinking beer, smoking a lot and going to sleep without lunch, things like that. And I worked at night.” P 8 “It was an oversight, because I ate crap instead of taking care of my health and I was getting a lot of ice. I didn’t take care of myself.” P. 19 “I’ve always worked a lot, always had stress at work.” P. 22
A man with multidrug-resistant TB tries to comprehend the difficulty in healing this disease:
“Just because I have worked with poison, that could be investigated, all of a sudden, it would be valid to do a biopsy of the lung, something more specific that could identify something that could causing this trouble I’m having to answer the treatment.” P. 1
People inhibiting this deadly disease described tuberculosis as an unimaginable, unexpected disease without specific causation:
“Never crossed my mind.” P. 1 “I did not expect. It looks like a shock that you take.” P. 10 “[∙∙∙] but I didn’t expect this was going to happen to me.” P. 17 “My aunt was feeling so great, she was a powerful black woman and out of the blue she started coughing and she was gone just like that.” P. 14
Witchcraft and spiritual determinants were also significant causalities for TB, as a consequence of jealousy and punishment:
“[∙∙∙] toll for being happy” P. 9, said a mother who got sick during breastfeeding; “[∙∙∙] a woman who put evil eye.” P. 4 “A woman out of envy, I don’t know if she did a ‘macumba’ to destroy me. But not of a heart attack, but slowly dying.” P. 11
Often, diseases such as TB are associated with a person’s imagination, traditional beliefs of the moral nature of health, illness, and human suffering. They symbolize many of the anxieties that people have as stated in the case of divine punishment. Diseases that are more than just a medical condition have become metaphors of everyday life [19] . To Susan Sontag, it is important that the disease is to not be mistaken for a metaphor [31] . Strategies that consider this view could contribute to the demystification of the disease.
Tuberculosis as a genetic predisposition was pointed out by a respondent due to generations of family members that have been affected by the disease. Many respondents had close relatives with TB. This then conforms to the high rates of prevalence of TB in the territory of Manguinhos and its social determinants [29] . However, for the respondents, the behavioral causes are what prevail. This strengthens the concept people have about the etiology and the contagion of the disease is not restricted to the health service because, they include a big difference of understandings and possibilities, which can be considered social constructions of the disease [32] .
3.4. Therapeutic Itinerary
The care and treatment for tuberculosis, as well as all the treatments and care activities in the Unified Health System (SUS), a universal system for the entire Brazilian population, have no cost to the patient. In the case of tuberculosis, care and subsequent treatment should occur in the primary care units. However, given the symptoms, the patient has access to various types of services.
The most common therapeutic itinerary of the patients in this study was emergency and private services instead of PHC units, as shown in Figure 1. In addition, patients who receive an incorrect first diagnosis of the disease and then an ineffective initial treatment, delay their recovery. His worsening carries, generally, results in forwarding the patient to PHC, when the diagnosis is completed and it can be started the TB treatment (Figure 1). The patients recognized that their journey to the start of treatment was harmful to their health, as shown in the following statements:
Figure 1. Most common therapeutic itinerary of the patient of tuberculosis. (ER = Emergence Room unit; BAAR = Alcohol-Acid Bacilli Resistant; TB = Tuberculosis).
“Why are you going to the doctor? The doctor says that you have a disease and you later discover that you have another disease. What kind of doctor is that? The doctor said my problem was depression.” P. 20 “The first time the doctor said it was the beginning of pneumonia. Then I took the medication. I got better. When I took the x-ray, that doctor who said it was pneumonia told me to go to a clinic and tell them there that I’m with tuberculosis.” P. 5
Several respondents reported that they had sought a private doctor that has been serving in the local community for several years because of his great receptiveness to the community.
“Yeah, with Doctor Cabral. He examined me, told me to take an x-ray, in return to show the test results for him, he gave me a referral to come here.” P. 6
This situation occurs in other places like São Paulo, where specialized services such as the emergency rooms have been more resolute than PHC units [33] . In Rio de Janeiro, during the period from 1998 to 2004, 28% to 33% of the cases of TB were reported in hospitals, while in São Paulo in 2005, this percentage was 42% [34] .
Since its inception, the PHC has been considered a paradigm in the health system. It reorganizes the system, opening the gateway of attention networks, articulating referrals to the secondary and tertiary levels and also reducing health expenditures [35] . However, in relation to the actions for TB control, there is a lack of coordination between services and sectors [36] . Studies shows that certain barriers need to be transposed to the TB care in the PHC so that they can be more satisfactory [37] . Some difficulties to assist patients in the PHC were identified as the lack of training of the teams, inclusive in relation to the knowledge of the mechanisms of transmission and detection of cases in addition to the shortage of network of support for TB diagnosis [26] [33] .
The search for health care depends on several factors related to users that present signs and symptoms of feeling sick as well as the decision to seek a health service. A study on therapeutic itinerary in Ribeirão Preto, São Paulo, showed that 69%, 16% and 15% of users preferred emergency services, PHC unit and other services, respectively, as stated in this research. Several explanations can be given, but a major factor is the resolute capacity of the ER units with greater access to tests and their operating regime (24 hours) [25] .
Respondents showed that the initial diagnosis of pneumonia or flu and the use of emergency services, and private services as their first choice of care generated a journey between services and delays in diagnosis. The same was observed in other studies that showed the inefficiency of the resolution of the case on the first visit. Some authors attribute this to low specificity of symptoms presented by users for decision-making, clinical examination times, and the shortage in professional training. In a systematic review about delay in diagnosis and treatment of TB in health services in India, 23 studies showed the median time between the appearance of the patient’s symptoms and health service demand was 18.4 days. Health units demand for diagnoses to be as long as 31 days and diagnosis to initiate effective treatment for 2.5 days. Therefore, the median total time was around two months (55.3 days) which increases the risk of disease transmission and worsening of the disease in the community. There was an emphasis that late diagnosis was related to the qualification of the services that were sought. About 48% of patients initially went to private doctors, and on average, they went to 2.7 health professionals before the diagnosis [38] . Another systematic review in relation to diagnosis and treatment delay pointed out that the central problem was a vicious cycle of repeated queries to health units with the prescription of antibiotics and difficulty in accessing specialist services [39] . Another study on TB in Ethiopia noted that more than half of the patients have postponed the trip to the public family clinics because they preferred alternative treatments (religious) or private institutions [40] . In another Brazilian study, managers gave their opinions on aspects related to diagnostic delay. The causes identified were due to users and health services. When it talks about users, the speech was of fear, prejudice, and lack of information. When it talks about the health services, the causes are structural difficulties and lack of qualification [41] .
It was observed in this study the difficulty in applying the diagnostic examination of sputum (Alcohol-Resistant Acid Bacilli-BAAR) even in the presence of persistent cough especially in areas with high prevalence of the disease. The chest x-ray was regularly requested to diagnosis TB. Literature data corroborate these results. According to national data, 14% of the TB cases didn’t go through any bacteriological test to define the diagnosis [42] . Our study has detected the delay in establishing the diagnosis has reached the limit of six months from the first visit.
Some initially put Comorbidities diagnosis have been a confusion with others that have similar symptoms such as two studies that was done involving a person with hypertension and other kidney failure. One interviewee was vehement when trying to sensitize the doctor that what she was feeling was not a result of hypertension because his malaise was quite different from the symptoms of hypertension. As stated earlier, the initial symptoms of TB are nonspecific. Malaise, tiredness, fatigue, lack of appetite are all elements that contribute to confusion with other illnesses. In addition, this confusion often deepens the importance of patient’s report and the interpretation of a health professional for decision-making. Other points to be raised would be the requirements to provide training for the diagnosis of TB and the workload of the professionals.
In the two cases with pleural effusion (water in the pleura-sac), it was hard to get the examination (thoracic puncture) for diagnostic clarification. This fact points to the difficulty of integrating the health care network that works so disjointed and it has difficulty to access other levels of assistance. In reality, there is a bottleneck in the system with low resolution of suspected cases of TB, especially for those who need more complex tests [26] .
We see the need of investment to cut down delays in diagnosing TB cases, whether to health services, the user and/or reference system and against reference ...
3.5. Social Support
We have detected the importance of social support for the treatment of TB as many participants have cited the family as the most important network of material and social support (food preparation, home remedies, and follow-up to the health service and during treatment). The family serves as a support network that helped the individual against isolation and the stigma surrounding the disease. In General, the family performed the social support in the figure of spouse, father, mother, children, brothers, sister-in-law, uncles, and grandparents:
“I had my husband’s attention, he went with me every time I needed to see the doctor, my family had no trouble, then raised a high self-esteem.” P. 14 “My brothers helped, they have deposited money in my account, or took the money and did shopping for me. Juices, medicine, vitamins, porridge.” P. 3
During the interviews, there were reports stating the disease raised awareness to family members:
“I became more noticeable; I won a ‘good morning’.” P. 14 “They give me the strength to make the right treatment. They take care.” P. 4
In the interviews, in only few reports the family stayed away. In one of the cases, it was a complete state of abandonment. The patient said he only got support from neighbors that offered him food. He was then forwarded to social services by the interviewers.
In the literature, the role of social support has been shown to be relevant to the adherence and the success of treatment. It may ease the burden on both the patient and family [43] [44] [45] [46] . Recent study showed that the presence of family or friends could be very decisive in matters relating to the maintenance of treatment, as it assists in the daily routines of basic health care and the compliance with the timetables of the medication [47] [48] .
Respondents demonstrated the religiosity in some lines, despite the support from the Church has been less commented:
“I asked God, only God. I wasn’t looking for praying or other things. I am from the Assembly of God, Evangelical religion. Just asking for God, praying, calling for help, because we know that God left the doctors to take care of us, and He is the doctor of doctors so we are treated by our doctors here on Earth, and we are also care by the power of God, and I’m alive here, and God had mercy on me.” P. 10 “My whole family is evangelical. And I was born within the Gospel. I was outside, but we end up holding more, asking the God to force my way through.” P. 23
In one of the interviews, the help from believers of the Church was more explicit:
“The brothers of the Church used to go there to pray together.” P. 2
On the other hand, there was a statement in which the respondent rejected the conversation that was offered by a religious representative because it was unwelcoming:
“No, no. Even my mother-in-law took a person in hospital, a pastor, who spoke a few things that I didn’t like it, he said it was punishment and I think it’s not punishment, it is a disease, and diseases are everywhere and I’m a normal person. I don’t think as a punishment or as a penalty, because I do not deserve any punishment or penalty.” P. 9
Respondents said that there is a need for emotional support from the health service, including homecare by the health team:
“She explained to me straight, doc. [∙∙∙] The doctor is super cool. She is playful. She is my friend.” P. 15 “The nurses, they used to go at my house take the medicine for me. I just want to thank them, the doctor who also treated me very well, none of them treated me badly, and they just wanted me feeling well.” P. 19
3.6. Impact on Life
The first impact presented refers to symptoms and difficulty in dealing with them. The main symptom reported was persistent cough followed by tiredness, phlegm, chest pain and fever. Hemoptysis occurred in only two cases. Six respondents said there was blood in their spit, which became the main differential symptom in relation to relatives and acquaintances that have had the disease. The hemoptysis has always been dramatic since the dawn of time, being associated to death. Prior to the existence of effective treatment, TB represented a largely incurable disease. In Brazil, writers described hemoptysis in their books, as Dinah Queiroz’s (“Then we’re told that the peach blossoms, whose rosy color resembled the white linen of the blood-colored handkerchiefs, coincided with the propitious seasons to hemoptysis”) and Manoel Bandeira (“We’ve also witnessed symptoms such as fever, hemoptysis, dyspnea and night sweats, a whole life that could have been existed and it has not”) [49] . The horror linked with death led to stigmatization and isolation.
The negative aspects of treatment have also affected the participants’ lives. In the early stages of treatment, nausea was the main side effect of the medication, as well as malaise, dizziness, weakness, yellow or red urine. The recommendation of fasting and difficulties in swallowing the pills were mentioned a few times as negative aspects of treatment, contributing to the NAATT:
“I think people also stop the treatment because of the reaction that the medicine gives. It is very difficult. The doctors talk about that when we will begin the treatment, the medicine is bad, the treatment is not easy, but to be cured it’s needed to go through this. [∙∙∙] My husband said: “that’s weird, you’re more or less, then you take your medicine and you get worse.” P. 17 “Oh it’s boring ∙∙∙ a big pill. Bad to swallow. I started thinking about stop taking this stuff. I’m good now. I talked to the doctor that I was good already [∙∙∙] because I wasn’t coughing anymore. I wasn’t having fever anymore. I got weight. I’m not feeling pain in the back anymore. Then I thought I was good already.” P. 6 “The pill was making me very weak, it gave me nausea and it gave me sickness motion. Every time I took the pill I threw up, I didn’t eat well, I wasn’t sleeping very well, I wasn’t working how I used to work. I complained a lot about this pill. I said: that doesn’t work, for the love of god.” P. 2
There were some difficulties that were pointed out in relation to treatment, which includes those mentioned above. They interfere with the adherence and in the efficacy of the treatment of TB. A qualitative study of the adherence in patients HIV/AIDS and TB/HIV coinfected showed that the changes in habits both in social life and in professional activities negatively influenced on adherence. The knowledge, perceptions, beliefs, and expectations that the patient has on the disease and its treatment may influence the way of dealing with the disease itself [50] . Other factors, such as anxiety about the possible adverse effects, the possibility of forgetting to take medication, the frustration with the health care team, and the lack of personal motivation, can also adversely affect the continuity of treatment [51] . There are some examples of the research that corroborate the literature.
Some respondents reported alternative treatments, such as “prayers”, home medicine as milk and roots. Such elements are present in the following lines:
“He has a tent of roots. If you have any questions, he picks up a book and shows the root and what is good, for which function.” P. 11
It was observed that in some lines, the cure was justified by the figure of God:
“God is in charge of these things; I don’t believe in coincidence. I believe in ‘jesuscidence’; I had willpower to cure this disease, and I believe there is a God, because if today there are people cured, it is because God healed [∙∙∙].” P. 10
It was noted that despite the patience perception on the current status of the cure for TB, it generates fear especially with the attachment of the possibility of death. According to Porto (2007), “Even if you admit to be a curable disease, there is a belief that there’s always something inside. Outdated ideas appear as that crystallized in the popular imagination” [18] . It is worth mentioning that the side effects and the fear of death compose a pair, which results in distress and depression. The following speech is an example that expresses the feeling of discouragement of a respondent with multidrug-resistant TB, due to the difficulty in healing:
“And, yeah I’ve been so mad lately because even I know I had a commitment with the medication I have to take, the improvement is not like I expect. So, lately, I’ve been so mad, very sad and I cry sometimes because of this.” P. 1
In this study, it was observed that although PHC was not the place of choice for the first attendance of the patients interviewed. While initiating the treatment, patients, unanimously demonstrated honest satisfaction with the service after it starts.
“She was nice. The treatment I had was very good here. I appreciate a lot. Give me good words. I recovered.” P. 15
Almost all respondents believe that the TB resulted from harmful habits. One of the most cited impacts was the change of behavior: not drinking, not smoking, feeding well, sleeping well and making sure one is not exposed to cold. Some respondents said that the idea of getting sick is as a way to become a better human being.
“When it’s raining a lot I don’ go out because I don’t want to get a lot of rain.” P. 39 “I sleep well now, I have lunch, then I fall into bed and I’m just going to wake up just the other day when I have to go to work.” P. 14
Changes in the how to face the life have also been reported.
“It changed my life in order to give value to my friends. Give value to my health. Give love to my loved ones.” P. 21 “I’m always with my head held high. But I wasn’t like that. Today I’m giving more value to things and fighting more. Become more flexible, I was very radical.” P. 17 “I think there are things we need to pass on life to be a little more noble. And I really thought that I had to go through this to be a little bit less pedantic, have a little more humility.” P. 9
There were also reports of financial, emotional impact, with prejudice in the love life of the couple and the family, in leisure and at work, as expressed in the following speech:
“Not to mention that it’s also causing wear on my relationship, because it’s been three years since my wife practically lives just to take care of me, we are not doing things like go out, to live a normal life, because of my situation, I’m taking remedies [...] Life changes, marital problem, there is no room for recreation because lack financial resource.” P. 1
Some respondents emphasized their lack of knowledge about the healing of the disease have taken a significant impact on their depressive state as well as driving them into a state of despair:
“I started treating for a couple months, three months [...] Then I said ‘Oh, I don’t want anything else, I already got this disease, I’m going to die. I went into depression, for me there weren’t any cure; I didn’t have any solution, so why should I go to the doctor? Why would I take care of myself? Then I gave up.” P. 14 “I went to the bathroom to look at me and all I saw was bone, I couldn’t see my body anymore. I gave up everything, I believe I had no reason to live, like, it seems my whole world was over, my life. I thought I was going to die.” P. 22
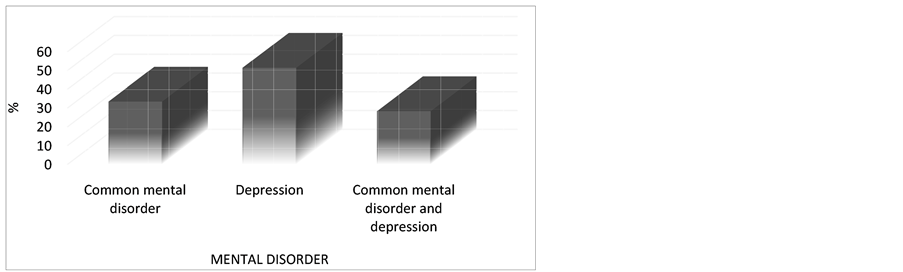
During the patient’s reports, we observed that psychological aspects or experiences related to sadness, depression or anxiety were not significant in coding. However, the application of the instruments (BDI and SQR-20) revealed that about half of the patients with TB were classified as having depression and about 30% were classified only with common mental disorder. The percentage of patients for positive common mental disorder and for positive depression also approaches 30% (Figure 2).
1). The prevalence rate of depression in the State of Rio de Janeiro according to the data collected by the National Health Research in 2013 is about 6.0% [52] . This result is below the proportion found in this study among TB patients. The prevalence rate of common mental disorder showed is this study did not differentiate significantly from data found in other studies whose focus was not TB patients. Lucchese et al. (2014), who investigated PHC patients, ranked the 31.47% of the investigated as possible cases of mental disorder [53] .
The presence of common mental disorders and their influence in treatment of several diseases is the subject of concern in the area of health. There are a few published works regarding the association of depression or depressive states among patients with TB. In a study conducted in the Philippines, a prevalence rate of 16.8% found patients with TB as being in a depressive state. However, the rates were lower than present studies [6] . A systematic review showed a greater frequency in relation to the common and lower in relation to depression [54] . Some studies indicate a strong association between the non-adherence and depression for HIV/TB coinfected patients [55] [56] ; showing the need for an early approach in other to decrease the suffering of the patient as well as increasing the success of treatment for TB and ultimately decrease the mortality rate.
Figure 2. Evaluation of the presence of common mental disorder and depression among tuberculosis patients. (*It was used the scale “Self Reporting Questionnaire” (SQR20) for sorting of the presence of common mental disorder-cut-off “≥8”; It was used the scale of the “Beck Depression Inventory (BDI)” for classification of depression-cut-off “≥10”.)
4. Final Considerations
This study presents manifold findings concerning tuberculosis experience in Man- guinhos, RJ, Brazil. Qualitative studies have been developed to understand patient adherence and especially on chronic or long lasting treatment schedule. This is the first paper from research efforts focused on tuberculosis treatment using MINI McGILL narrative interview. Similar environments may enhance analogous therapeutic pathways, nevertheless cultural and social dimension circumscribes closely some labels, causal attributions and salient prototypes related to current health problems that belong to this very community. TB diagnosis was slow, uncertain, and either over or undervalued; stigma often led to isolation or refraining from TB disclosure (or any related health problem). Primary care units in poor income areas are still requiring strategic approaches to promote treatment adherence.
Media resources helped on disease elucidation and health information contributed to service access and rational utilization. PHC facilities should develop health education agenda including tuberculosis patients and their relatives. Therapeutic itineraries stressed the necessity of care network reorganization―from acess point to full recovery.
National policy on PHC recommends closer bonds involving patient and health staff (physician or GP). This study suggests that patients do not seek immediately doctor or nurse support, sometimes remaining open to different pathways to care-religious examples, pregnant prototypes, etc. The principle of integrality, ancillary in Brazilian SUS, is cogent to care-network building tasks―ranging from diagnosis, follow-up and referral system. Training health teams in TB diagnosis and treatment are paramount, as well as surpassing difficulties of adherence and stigma reproduction. It is necessary to endeavor social networks comprising family resources and support.
The social network usually involved friends (usually neighbours), family (usually living together) and religious staff (priests, “mediums”, sorcerers, etc.)―being considered helpful and responsible for treatment continuity. Relationship with PHC staff, understanding of treatment complexity and its phases, and feeling safe and secure with the regular functioning of the unit, plant or facility were motivating and allowed medicament adherence, minimum self-care strategies, and habits change or rethinking.
Common mental disorders or depression in TB patients were troubling enough to suggest that screening instruments for depression might be adopted in routine assessment at health services (PHC). Patients’ experiences of TB are associated with a complex set of meanings and reasoning styles that include social, moral and spiritual values. Suffering, hopelessness and despair do not prevent these people from drugs, parties and bohemian lifestyle nor from religious beliefs and practices ranging from Spiritism or neo-pentecostalism to afro-brazilian rituals. Discussing needs of mental health support or treatment were beyond this study scope, although it showed some strategies of coping that might be mitigating some problems but did result directly in treatment drop-out or medicament non-adherence. As a limitation of the research, the prevalence and treatment of the investigated persons were not compared with normal persons.
Further qualitative studies are necessary to unveil the complexity of such experiences.
Acknowledgements
We thank the agreement TEIAS/FIOCRUZ (Integrated Territory of Health Care/Fundação Oswaldo Cruz) between the municipality of Rio de Janeiro and the Oswaldo Cruz Foundation for financial support for research.
Cite this paper
O’Dwyer, G., Lino, V., Rodrigues, N., Kramer, M., Reis, I., Fro- ssard, V., Vianna, E., Elias, L. and Estellita- Lins, C.E. (2017) Illness Experience in a Ve- ry Low Income/Poor District of Rio de Ja- neiro, Brazil: Tuberculosis, Medication Adherence and Common Mental Disorders. Health, 9, 534-555. https://doi.org/10.4236/health.2017.93038
References
- 1. WHO (2015) Global Tuberculosis Report. World Health Organization, Geneva.
- 2. WHO (2003) Adherence to Long-Term Therapies: Evidence for Action. In: WHO, Ed., WHO Adherence to Long-Term Therapies Global Adherence Interdisciplinary Network, Geneva, 209 p.
- 3. Brasil, P.E. and Braga, J.U. (2008) Meta-Analysis of Factors Related to Health Services That Predict Treatment Default by Tuberculosis Patients. Cadernos de Saúde Pública, 24, s485-s502.
https://doi.org/10.1590/S0102-311X2008001600003 - 4. Araujo, G. and Tr, G. (2006) Adesão ao tratamento anti-hipertensivo: Uma análise conceitual. Revista Eletrônica de Enfermagem, 8, 259-272.
- 5. Reiners, A.A., Azevedo, R.C., Vieira, M.A. and de Arruda, A.L. (2008) Bibliographic Production about Adherence/Non-Adherence to Therapy. Ciência & Saúde Coletiva, 13, 2299-2306.
https://doi.org/10.1590/S1413-81232008000900034 - 6. Masumoto, S., Yamamoto, T., Ohkado, A., Yoshimatsu, S., Querri, A.G. and Kamiya, Y. (2014) Prevalence and Associated Factors of Depressive State among Pulmonary Tuberculosis Patients in Manila, The Philippines. International Journal of Tuberculosis and Lung Disease, 18, 174-179.
https://doi.org/10.5588/ijtld.13.0335 - 7. Mandaknalli, R. and Giriraj, B. (2015) Prevalence of Depression in Tuberculosis Patients in a Terciary Care Hospital. Scholars Journal of Applied Medical Sciences, 3, 3.
- 8. Sa, A. (2010) Co-Morbidit Anxiety and Depression among Pulmonary Tuberculosis Patients. Journal of the College of Physicians and Surgeons—Pakistan, 20, 2.
- 9. Shen, T.C., Wang, C.Y., Lin, C.L., Liao, W.C., Chen, C.H., Tu, C.Y., et al. (2014) People with Tuberculosis Are Associated with a Subsequent Risk of Depression. European Journal of Internal Medicine, 25, 936-940.
- 10. Steinberg, S. and Fleming, P. (2000) The Geographic Distribution of AIDS in the United States: Is There a Rural Epidemic? The Journal of Rural Health: Official Journal of the American Rural Health Association and the National Rural Health Care Association, 16, 11-19.
- 11. Ferreira, J., Engstrom, E. and Alves, L. (2012) Adesão ao tratamento da tuberculose pela população de baixa renda, moradora de Manguinhos, Rio de Janeiro: As razões do (im)provável. Cadernos de Saúde Coletiva, 20, 5.
- 12. Volmink, J. and Garner, P. (2007) Directly Observed Therapy for Treating Tuber- culosis. The Cochrane Database of Systematic Reviews, No. 5, CD003343.
https://doi.org/10.1002/14651858.CD003343.pub3 - 13. Kleinman, A. and Good, B. (1985) Culture and Depression: Studies in the Antropo- logy and Cross-Cultural Psychiatry of Affect and Disorder. University of California Press, Los Angeles, 521 p.
- 14. Kleinman, A. (1988) The Illness Narrative: Suffering, Healing and the Human Condition. Basic Books, New York, 269 p.
- 15. Leal, E.M., Souza, A.N., Serpa, O.D., Oliveira, I.C., Dahl, C.M., Figueiredo, A.C., et al. (2016) The McGill Illness Narrative Interview—MINI: Translation and Cross- Cultural Adaptation into Portuguese. Ciencia & Saude Coletiva, 21, 2393-2402.
https://doi.org/10.1590/1413-81232015218.08612015 - 16. Santos, K.O., Araújo, T.M. and Oliveira, N.F. (2009) Factor Structure and Internal Consistency of the Self-Reporting Questionnaire (SRQ-20) in an Urban Population. Cadernos de Saúde Pública, 25, 214-222.
https://doi.org/10.1590/S0102-311X2009000100023 - 17. Paranhos, M., Argimon, I. and Werlang, B. (2010) Propriedades psicométricas do Inventário de depressão de Beck-II (BDI-II) em adolescentes. Avaliação Psicológica, 9, 9.
- 18. Pôrto, A. (2007) Social Representations of Tuberculosis: Stigma and Prejudice. Re- vista de Saúde Pública, 41, 43-49.
https://doi.org/10.1590/S0034-89102007000800007 - 19. Goffaman, E. (1891) Estigma—Notas sobre a manipulação da identidade deteriorada.
http://disciplinas.stoa.usp.br/pluginfile.php/92113/mod_resource/content/1/Goffman%3B%20Estigma.pdf - 20. Lewis, J.N., Storck, C.F. and McArdell, T.L. (1993) Geographic Distribution of AIDS Patients Diagnosed at Eight Baltimore Hospitals. Maryland Medical Journal, 42, 761-764.
- 21. Deribew, A., Abebe, G., Apers, L., Jira, C., Tesfaye, M., Shifa, J., et al. (2010) Prejudice and Misconceptions about Tuberculosis and HIV in Rural and Urban Commu- nities in Ethiopia: A Challenge for the TB/HIV Control Program. BMC Public Health, 10, 400.
https://doi.org/10.1186/1471-2458-10-400 - 22. Freitas, I.M.D., Popolin, M.P., Touso, M.M., Yamamura, M., Rodrigues, L.B.B., Santos Neto, M., et al. (2015) Factors Associated with Knowledge about Tuberculosis and Attitudes of Relatives of Patients with the Disease in Ribeirão Preto, São Paulo, Brazil. Revista Brasileira de Epidemiologia, 18, 326-340.
https://doi.org/10.1590/1980-5497201500020004 - 23. Mendes, M. (1998) A clientela e os profissionais de saúde diante da tuberculose. Dissertação de mestrado, Faculdade de Ciência Médica/UNICAMP, Campinas/São Paulo.
http://www.bibliotecadigital.unicamp.br/document/?code=vtls000128959 - 24. MS MdS (2011) Manual de recomendações para controle da tuberculose no Brasil. Ministério da Saúde, Brasília.
https://www.nescon.medicina.ufmg.br/biblioteca/imagem/manual_recomenda%C3%A7oes_controle_tuberculose.pdf - 25. Beraldo, A.A., Arakawa, T., Pinto, E.S., Andrade, R.L., Wysocki, A.D., da Silva Sobrinho, R.A., et al. (2012) Delay in the Search for Health Services for the Diagnosis of Tuberculosis in Ribeirao Preto, Sao Paulo. Ciencia & Saude Coletiva, 17, 3079- 3086.
https://doi.org/10.1590/S1413-81232012001100024 - 26. Monroe, A.A., Gonzales, R.I., Palha, P.F., Sassaki, C.M., Ruffino Netto, A., Vendramini, S.H., et al. (2008) Involvement of Health Primary Care Teams in the Control of Tuberculosis. Revista da Escola de Enfermagem da USP, 42, 262-267.
https://doi.org/10.1590/S0080-62342008000200008 - 27. Couto, D.S.D., Carvalho, R.N., Azevedo, E.B.D., Moraes, M.N.D., Pinheiro, P.G.O.D. and Faustino, E.B. (2014) Fatores Determinantes Para o Abandono do tratamento da tuberculose: Representações dos usuários de um hospital público. Saúde em Debate, 38, 572-581.
- 28. Schütz, G., Pivetta, F. and Engstron, E. (2012) Contexts of Manguinhos’ Teias- School. In: Ensp/Fiocruz, Eds., The Integrated Area of Health Attention in Manguinhos: We Are All Learners, Rio de Janeiro, 25-37.
- 29. SMS SMdS (2016) Coordenadoria de Saúde da &AACUTE;rea de Planejamento 3.1 (CAP 3.1). Secretaria Municipal de Saúde, Rio de Janeiro.
http://cap31.blogspot.com.br/ - 30. Fiotec (2016) Mostra interativa do Fundo Global TB: Fiotec.
http://www.fiotec.fiocruz.br/index.php - 31. Sontag, S. (1978) Illness as Metaphor. McGraw-Hill Ryerson Ltd., Toronto.
https://monoskop.org/images/4/4a/Susan_Sontag_Illness_As_Metaphor_1978.pdf - 32. Souza, S.S., Silva, D.M.G.V. and Meirelles, B.H.S. (2010) Representações sociais sobre a tuberculose. Acta Paulista de Enfermagem, 23, 23-28.
https://doi.org/10.1590/S0103-21002010000100004 - 33. de Oliveira, M.F., Arcencio, R.A., Ruffino-Netto, A., Scatena, L.M., Palha, P.F. and Villa, T.C. (2011) The Front Door of the Ribeirao Preto Health System for Diagno- sing Tuberculosis. Revista da Escola de Enfermagem da USP, 45, 898-904.
https://doi.org/10.1590/S0080-62342011000400015 - 34. SES_SP SEdS-S (2015) Boletim Epidemiológico Paulista. São Paulo.
http://www.saude.sp.gov.br/resources/ccd/homepage/bepa/edicao-2015/edicao_140_-_agosto_2.pdf - 35. Starfield, B. (2002) Atenção primária: Equilíbrio entre necessidades de saúde, equilíbrio e tecnologia Brasília: UNESCO. Ministério da Saúde.
http://www.dominiopublico.gov.br/download/texto/ue000039.pdf - 36. Barrêto, A.J., de Sá, L.D., Nogueira, J.E.A., Palha, P.F., Pinheiro, P.G., de Farias, N.M., et al. (2012) Organization of Health Services and Tuberculosis Care Manage- ment. Ciencia & Saude Coletiva, 17, 1875-1884.
https://doi.org/10.1590/S1413-81232012000700027 - 37. Villa, T.C. and Ruffino-Netto, A. (2009) Performance Assessment Questionnaire Regarding TB Control for Use in Primary Health Care Clinics in Brazil. Journal Brasileiro de Pneumologia, 35, 610-612.
- 38. Sreeramareddy, C.T., Qin, Z.Z., Satyanarayana, S., Subbaraman, R. and Pai, M. (2014) Delays in Diagnosis and Treatment of Pulmonary Tuberculosis in India: A Systematic Review. The International Journal of Tuberculosis and Lung Disease, 18, 255-266.
https://doi.org/10.5588/ijtld.13.0585 - 39. Storla, D.G., Yimer, S. and Bjune, G.A. (2008) A Systematic Review of Delay in the Diagnosis and Treatment of Tuberculosis. BMC Public Health, 8, 15.
https://doi.org/10.1186/1471-2458-8-15 - 40. Mesfin, M.M., Newell, J.N., Walley, J.D., Gessessew, A. and Madeley, R.J. (2009) Delayed Consultation among Pulmonary Tuberculosis Patients: A Cross Sectional Study of 10 DOTS Districts of Ethiopia. BMC Public Health, 9, 53.
https://doi.org/10.1186/1471-2458-9-53 - 41. De Sá, L.D., Barrêto, A.J., Nogueira, J.E.A., Cunha, F.T., Palha, P.F. and Villa, T.C. (2013) The Discourse of Health Managers on Aspects Related to the Delay in Tuberculosis Diagnosis. Revista da Escola de Enfermagem da USP, 47, 1170-1177.
https://doi.org/10.1590/S0080-623420130000500022 - 42. Guerra, L., Rego, L. and Conde, M. (2008) Diagnosis of Pulmonary Tuberculosis in Patients with Negative Acid-Fast Staining in Sputum. Rio de Janeiro.
http://sopterj.com.br/profissionais/_educacao_continuada/curso_tuberculose_9.pdf - 43. Torrens, A.W., Rasella, D., Boccia, D., Maciel, E.L., Nery, J.S., Olson, Z.D., et al. (2016) Effectiveness of a Conditional Cash Transfer Programme on TB Cure Rate: A Retrospective Cohort Study in Brazil. Transactions of the Royal Society of Tropical Medicine and Hygiene, 110, 199-206.
https://doi.org/10.1093/trstmh/trw011 - 44. Wingfield, T., Boccia, D., Tovar, M.A., Huff, D., Montoya, R., Lewis, J.J., et al. (2015) Designing and Implementing a Socioeconomic Intervention to Enhance TB Control: Operational Evidence from the CRESIPT Project in Peru. BMC Public Health, 15, 810.
https://doi.org/10.1186/s12889-015-2128-0 - 45. Rocha, C., Montoya, R., Zevallos, K., Curatola, A., Ynga, W., Franco, J., et al. (2011) The Innovative Socio-Economic Interventions against Tuberculosis (ISIAT) Project: An Operational Assessment. The International Journal of Tuberculosis and Lung Disease, 15, S50-S57.
https://doi.org/10.5588/ijtld.10.0447 - 46. Chirinos, N.E., Meirelles, B.H. and Bousfield, A.B. (2015) Social Representations of TB Patients on Treatment Discontinuation. Revista Gaúcha de Enfermagem, 36, 207-214.
https://doi.org/10.1590/1983-1447.2015.esp.56723 - 47. Freitas, I.M., de Almeida, J., Pinto, I.C., Villa, T.C.S., Brunello, M.E.F., Pinto, P.F.P.S., et al. (2012) Knowledge and Perception about Tuberculosis of Patients’ Fa- milies under Directly Observed Treatment at a Health Service in Ribeirão Preto-SP, Brazil. Texto Contexto—Enferm, 21, 642-649.
https://doi.org/10.1590/S0104-07072012000300020 - 48. Nogueira Jde, A., Trigueiro, D.R., de Sa, L.D., da Silva, C.A., Oliveira, L.C., Villa, T.C., et al. (2011) Family Focus and Community Orientation in Tuberculosis Control. Revista Brasileira de Epidemiologia, 14, 207-216.
- 49. Antunes, J.L.F., Waldman, E.A. and Moraes, M.D. (2000) A tuberculose através do século: ícones canônicos e signos do combate à enfermidade. Ciencia & Saude Coletiva, 5, 367-379.
https://doi.org/10.1590/S1413-81232000000200010 - 50. Sousa Filho, M.P.D., Luna, I.T., Silva, K.L.D. and Pinheiro, P.N.D.C. (2012) Pa- cientes vivendo com HIV/AIDS e coinfecção tuberculose: Dificuldades associadas à adesão ou ao abandono do tratamento. Revista Gaúcha de Enfermagem, 33, 139- 145.
https://doi.org/10.1590/S1983-14472012000200020 - 51. Melchior, R., Nemes, M.I., Alencar, T.M. and Buchalla, C.M. (2007) Challenges of Treatment Adherence by People Living with HIV/AIDS in Brazil. Revista de Saúde Pública, 41, 87-93.
https://doi.org/10.1590/S0034-89102007000900014 - 52. IBGE, FIOCRUZ (2014) Pesquisa Nacional de Saúde 2013: Percepção do estado de saúde, estilo de vida e doenças crônicas Rio de Janeiro.
http://biblioteca.ibge.gov.br/biblioteca-catalogo?view=detalhes&id=291110 - 53. Lucchese, R., Sousa, K.D., Bonfin, S.D.P., Vera, I. and Santana, F.R. (2014) Prevalência de transtorno mental comum na atenção primária. Acta Paulista de Enfermagem, 27, 200-207.
https://doi.org/10.1590/1982-0194201400035 - 54. Araújo, G.S.D. (2014) Pereira SM, dos Santos DN. Revisão sobre tuberculose e transtornos mentais comuns.
- 55. Kehbila, J., Ekabe, C.J., Aminde, L.N., Noubiap, J.J., Fon, P.N. and Monekosso, G.L. (2016) Prevalence and Correlates of Depressive Symptoms in Adult Patients with Pulmonary Tuberculosis in the Southwest Region of Cameroon. Infectious Diseases of Poverty, 5, 51.
https://doi.org/10.1186/s40249-016-0145-6 - 56. Duko, B., Gebeyehu, A. and Ayano, G. (2015) Prevalence and Correlates of Depression and Anxiety among Patients with Tuberculosis at WolaitaSodo University Ho- spital and Sodo Health Center, WolaitaSodo, South Ethiopia, Cross Sectional Study. BMC Psychiatry, 15, 214.
https://doi.org/10.1186/s12888-015-0598-3