Open Journal of Nursing
Vol.3 No.1(2013), Article ID:29546,6 pages DOI:10.4236/ojn.2013.31012
The problem-based learning integrated with simulation to improve nursing students’ self-efficacy
![]()
Department of Nursing, Inha University, Incheon, South Korea
Email: *sohnmin@inha.ac.kr
Received 20 January 2013; revised 27 February 2013; accepted 8 March 2013
Keywords: Nursing Education; Nursing Process; Problem-Based Learning; Simulation; Undergraduate Nursing Students
ABSTRACT
Introduction: The purposes of this study were to describe the simulation integrated with problem-based learning (SIM-PBL) module to educate the nursing process for clients with hypertension and to evaluate its effectiveness on nursing students’ self-efficacy (SE). Methods: This study was a one group preand posttest design. Twenty five students received a 5-hour SIM-PBL program focused on nursing care of clients with hypertension. A newly developed self-report questionnaire was used to assess SE in four areas of the nursing process with a scale of 0 (not at all confident) to 10 (totally confident). The four areas were subjective data assessment, physical examination, prioritizing nursing care and health promotion advices. Results: At baseline, students’ SE ranged from 5.5 ± 1.4 (prioritizing nursing care) to 7.6 ± 1.4 (subjective data assessment). After SIM-PBL education, all areas of nursing process presented statistically significant improvements of SE. The improvements were most noticeable in prioritizing nursing care. Conclusion: The SIM-PBL module was effective in improving the students’ self-efficacy in the nursing process for patients with hypertension. Further studies are recommended in developing SIM-PBL modules for diverse nursing topics and evaluating their effectiveness in various aspects of students’ competency.
1. INTRODUCTION
The educational challenges confronting nursing schools in the twenty-first century are far more difficult than their counterparts faced in years past. Patients are sicker, present faster changing manifestations, and stay for a shorter time in the hospital. Nursing schools have access to fewer clinical sites and expert instructors due to increased awareness of patient safety and the global nursing shortage. In the current environment, students are at high risk of fewer clinical hours, low quality clinical practicum, and limited experience of a nurse’s various roles. Students have few chances to practice nursing skills and spend most of their time in observation rather than actively engaged in the learning process to improve their decision making, critical thinking, and problem solving.
Problem solving is acknowledged to be one of the most important competencies students must acquire during their nursing education. Problem-based learning (PBL), which is designed to improve students’ problem solving capabilities, was integrated into health education in the early 1960 s [1]. In PBL, learning derives from problem-based instruction rather than discrete, topicfocused education [2]. Nursing education has adopted the PBL method, and its effectiveness has been proved in various facets of nursing education [3]. To maximize the effectiveness of PBL, Harden and Davis [4] suggested that it should be the continuum between theoretical and clinical learning. However, in nursing education, PBL has been used mostly in didactic courses and rarely for clinical practicum.
Simulation in nursing education, another innovative teaching strategy, mimics clinical situations. It gives nursing students the opportunity to achieve clinical competency through cognitive, psychomotor, and affective learning experiences in various scenarios [5]. Of the various types of simulation, high-fidelity simulation offers highly sophisticated case scenarios and involves equipment that can be used to solve the problems [5]. High fidelity simulation has been shown to be effective in educating students about critical care [6], medication administration [7], patient safety [8], basic nursing skills [9], and communication skills [10].
In this study, the researchers show how PBL and simulation have been integrated to maximize their effectiveness in clinical nursing education. Previous studies have indicated that simulation, coupled with PBL, can offer nursing students a more integrated learning process and a wider spectrum of clinical education. Simulation integrated with problem-based learning (SIM-PBL) has been used to improve clinical competency [11], critical assessment [12], academic achievement [13], problem solving [9], and self-efficacy (SE) [14] for nursing and medical students.
Of all the potential clinical topics that are suitable for a SIM-PBL module, we selected the nursing process for patients with hypertension. In fact, PBL mirrors the nursing process, which is the fundamental framework of clinical nursing education. Nursing process is an organizing framework for professional nursing practice that uses scientific reasoning and problem solving [15]. Furthermore, hypertension is one of the most prevalent chronic health conditions in Korea: 27% of adults older than 30 have the condition [16].
The selected topic offers nursing students a broad spectrum of learning opportunities, from health assessment to health promotion. This study’s objectives were to describe the use of a SIM-PBL module to educate students on the nursing process for patients with hypertension and to evaluate the module’s effectiveness on students’ self-efficacy (SE).
2. METHODS
2.1. Design and Study Participants
This study used a one-group pretest-posttest design. Over the course of 2 years, 25 nursing students from two cohorts were recruited to participate in the study: 11 students from the 2010 class and 14 students from the 2011 class. Data were collected from September 1, 2010 to September 15, 2011.
The researchers used a convenience sampling method with nursing students who were enrolled in third year of a 4-year baccalaureate program at a university in Incheon, South Korea. Sample size could not be calculated because the SIM-PBL program was part of the regular curriculum, and students who wanted to enroll in the SIMPBL course had to be included in the study. Students could enroll in the SIM-PBL course if they were enrolled in the third-year of the nursing program and had at least one semester of clinical practicum experience. Students were excluded if they had taken a leave of absence during the previous semester or had any previous experience with simulation-based learning.
2.2. SIM-PBL: Module Development and Contents
A focus group was formed to develop the SIM-PBL module: It included faculties and research nurses experienced in critical care and nursing education. The module comprised a 2-hour didactic session and a 3-hour SIMPBL session. The didactic session included a lecture on the nursing process for patients with hypertension and health promotion strategies; the SIM-PBL session comprised a PBL session and a simulation session. After a scenario was presented, students were to develop a care plan for the patient and to practice nursing care during the PBL session. The case for this SIM-PBL scenario involved a middle-aged man who visits a community health center. An overweight smoker, he was recently diagnosed with hypertension. Students were required to demonstrate their nursing care plan within 15 minutes of the simulation session.
During the SIM-PBL session, students were expected to achieve the learning objectives as a group, which included assessment using interview and a cardiovascularfocused physical examination; prioritizing the nursing diagnosis, expected outcomes, and nursing interventions; and providing health promotion advice. Because the patient in question did not have any signs or symptoms of hypertension, the students’ nursing intervention consisted of health promotion advice. The students also had to demonstrate therapeutic communication and professional attitude during the session.
Debriefing, which is an essential part of integrating the learning experience, is a question/answer method designed to reveal whether the learning objectives were achieved in a safe and correct way. In this study, the questions used for debriefing were adapted from recommendations of the National League of Nursing [5]. The instructor questioned the students about their experience, the patient’s health problems, priorities for nursing care, and therapeutic communication. Participants were also asked to identify the most important thing that they learned from the scenario and what they would change if they have another chance to participate in the same scenario.
2.3. SIM-PBL: Module Operation
The SIM-PBL session, which was held a week after the didactic session, consisted of orientation, the PBL session, the simulation session, debriefing, and breaks. After the instructor had briefed the students about the scenario, they were randomly assigned to groups of three or four. The PBL session was held in a designated room, which was equipped with an examination bed, desk, chairs, and a white board. During the session, students were encouraged to actively participate in group discussions and to practice their interview questions for patients, physical examination skills, and health promotion advice. Students were informed that a simulation session involving the same scenario would follow, but all of the activities should be finished within 15 minutes. They had to prioritize all activities using problem-solving strategies.
The simulation session occurred in a simulation laboratory, which was equipped with a SimMan® (Laerdal, Toronto, ON, Canada), a high fidelity simulation performance program. Once a student group entered the simulation room, they were expected to conduct themselves as if they were encountering a real patient. They could review the patient’s medical record and medication administration record. If they wished additional information, they could actually talk to the simulator; the instructor, acting as the patient, responded to them by microphone. After the simulation was completed, all of the participants attended a debriefing session to review videotapes of their performance during the simulation and to provide feedback to each other through in-depth discussion.
2.4. Measurements
Measurements included the students’ age, gender, and SE in the nursing process for patients with hypertension. To assess SE, the researchers developed a questionnaire based on Bandura’s social cognitive theory [17]. In that theory, SE is defined as individuals’ judgment of their own capabilities to perform actions required to attain target goals. In this study, we defined that SE is the nursing students’ perceived confidence in the nursing process in a given scenario.
Four areas of the nursing process were identified in this study: subjective data assessment, physical examination, prioritizing nursing care, and health promotion advice. Subjective data assessment included 9 items that assess symptoms, past and family history and health behaviors related to cardiovascular disease. Each area of the nursing process included 9 to 5 items of detail activities students are expected to perform. Students were asked to indicate their level of confidence for each question item a scale that ranged from 0 (not at all confident) to 10 (absolutely confident). The total SE scores for each area of the nursing process represent the mean of SE scores for each question and can range from 0 to 10. Content validity was confirmed by the expert panel of two nursing faculty, a research nurse, and a simulation coordinator. The Cronbach’s alpha coefficients for each area were 0.87 (subjective data assessment), 0.89 (objective data assessment), 0.94 (prioritizing nursing care) and 0.91 (health promotion advice). Cronbach’s alpha for all questions was 0.95.
2.5. Data Collection
This study was approved by the Institutional Review Board of the university where data collection occurred. Informed consent was exempted because the SIM-PBL course is part of the regular curriculum, and data collection was considered to be a routine evaluation process for course development. Nonetheless, one of the researchers (not the instructor) informed the students that the study’s data could be used for research purposes as well and that this process would not affect their grade. Baseline data collection occurred at the beginning of the didactic session. Posttest data were collected immediately after the SIM-PBL session and the debriefing session, which was held 1 week after the didactic session.
2.6. Data Analysis
SPSS version 18.0 (SPSS, Chicago, IL, USA) was used for statistical analysis. Explorative descriptive analysis was performed to validate data entry and to examine the nature of the data. Skewness and kurtosis of the total scores for each area were determined, and the scores were all normally distributed despite the small sample size. We could not find any major changes of curriculum and any statistical difference in SE between the two cohorts. Therefore, the data were pooled. We used the paired t test to evaluate the relationship between SIMPBL and SE by comparing SE scores of the pretest and posttest. All statistical tests were performed with α = 0.05 in a two-tailed test.
3. RESULTS
Participants were all women. Their mean age was 20.9 ± 1.2 years. Tables 1 and 2 present the means of SE scores for each area of the nursing process. At baseline, prioritizing nursing care showed the lowest SE among the four areas, followed by physical examination, health promotion advice, and subjective data assessment. All of the areas showed statistically significant SE improvement after the SIM-PBL instruction.
Table 1 presents the SE scores for subjective data assessment and physical examination. After the intervention, SE improved in 4 out of 9 items in subjective data assessment; the improvements were statistically significant for assessment of symptoms (t = 2.95, p = 0.007), exercise (t = 2.26, p = 0.033), weight and calculating body mass index (t = 2.45, p = 0.022), and medication compliance (t = 2.10, p = 0.046). In objective data assessment, after the intervention, SE improved in 3 out of 5 items, and the improvements were statistically signifycant at assessment of jugular vein distension (t = 2.23, p = 0.035), location of point of maximum impulse (t = 2.08, p = 0.048), and listening heart sounds (t = 2.77, p = 0.010). Critical thinking showed the most distinctive improvement in SE scores after the SIM-PBL experience (Table 2). All 4 items in critical thinking showed statistically significant improvement in SE scores; the improvements were statistically significant for prioritizing nursing diagnosis (t = 4.36, p < 0.001), prioritizing the expected outcomes (t = 5.60, p < 0.001), prioritizing interventions (t = 4.54, p < 0.001), and selecting the way
Table 1. Means (SD) of self-efficacy in subjective data assessment and physical examination (N = 25).
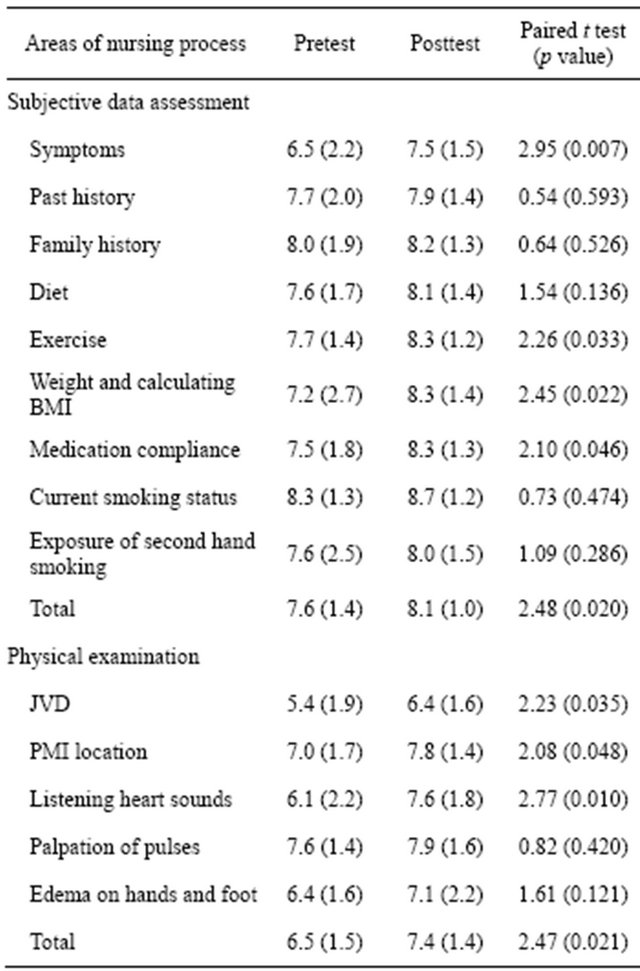
Abbreviations: SD = Standard deviation; BMI = Body mass index; JVD = Jugular vein distension; PMI = Point of maximum impulse.
to evaluate expected outcomes (t = 5.71, p < 0.001). SE in health promotion advice is also presented at Table 2. In health promotion advice, after the intervention, SE improved in 3 out of 5 items; the improvements were statistically significant for smoking cessation (t = 2.83, p = 0.009), diet (t = 2.06, p = 0.049) and taking medication as ordered (t = 2.10, p = 0.047).
4. DISCUSSION
This study was conducted to describe a SIM-PBL module for patients with hypertension and to evaluate the relationship between the SIM-PBL module and SE in the nursing process. Three findings are particularly noteworthy.
First, SE in the nursing process improved for all 4 areas, and most of the improvements were statistically significant despite the small sample size. In particular, SE improvement was most noticeable in prioritizing nursing care. Students’ ability to prioritize problems is not an easy skill to master; PBL targets this area of learning.
Table 2. Means (SD) of SE in prioritizing nursing care and health promotion advice (N = 25).
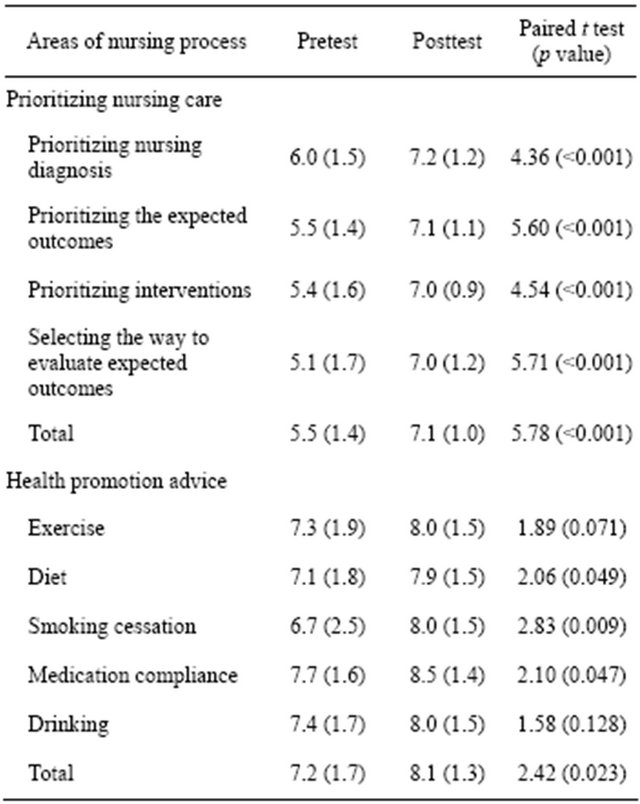
Abbreviations: SD = Standard deviation; SE = Self-efficacy.
The substantial improvement in prioritizing nursing care may indicate that PBL was well-integrated with simulation and resulted in a higher level of learning. PBL emphasizes an integrative way of learning through small group, self-directed study with a faculty member who acts as a facilitator [18]. The SIM-PBL was able to present these essential PBL attributes successfully.
Second, student competency in physical examination noticeably improved. Although health assessment is a key component of the nursing curriculum, nursing faculty have often observed that nursing students’ skills are quite disappointing, especially in the clinical environment. Traditionally, instructors have taught students in the laboratory how to take a detailed history and to perform a complete physical examination, absent any clinical context. Such an approach to the physical examination is time-consuming and is rarely performed in hospitals, where most of the clinical practicum occurs. In this study, the researchers noticed that students lacked confidence in cardiovascular-focused physical examination before they participated in the clinical scenario, but improved after the SIM-PBL session. This observation is consistent with the results of previous studies that evaluated physical examination capabilities in nurses [19] and nursing students [20]. Simulation [21], PBL [19] or SIMPBL [11] have been alternative ways to improve students’ ability to perform the physical examination appropriately in varied clinical situations. Furthermore, previous studies have shown that SIM-PBL is better than PBL alone in teaching those skills to nursing students [11] and medical students [12].
Finally, SIM-PBL was also effective in enhancing the students’ skill in health behavior assessment and communication of health promotion advice. Although both activities depend heavily on verbal communication between student and simulator (i.e., an instructor conversing by microphone), the students’ confidence improved compared with that of the control group, and the change was statistically significant. Traditionally, nursing students have learned the skill of giving health promotion advice in a classroom or in a community-based practicum; it was often based on the intensive health promotion education project. However, like health assessment, providing health promotion advice to patients is a nursing skill that is more often needed in acute care clinical settings. Health promotion advice should be case specific and individualized that is, based on a patient’s specific needs and clinical conditions. In that context, health promotion advice should be provided with, not separate from, other nursing care. For example, nursing students must learn how to provide health promotion advice on such topics as smoking cessation, healthy diet, and exercise as they perform health assessment, administer medications, and provide meals. Thus, SIM-PBL could be an excellent methodology to teach nursing students how to provide health promotion advice in an almost-real clinical environment.
This study has several limitations. First using a onegroup pretest and posttest design without a control group may undermine the effect of SIM-PBL on SE in the nursing process. Second, the small sample size may have resulted in low power to meet the study purposes. Third, the study participants were recruited by convenience sampling from one university. Thus, generalizability is limited. Finally, potential confounding factors such as learning style, grades and potential unique characteristics of each cohort were not assessed.
5. CONCLUSION
The SIM-PBL module was developed to teach undergraduate nursing students how to care for patients with cardiovascular disease. The module was successfully applied and demonstrated statistically significant relationships with nursing students’ SE. A more advanced research design is recommended for the future, one that uses random selection and random assignment of the control and intervention groups and collects information about potential confounding factors. In doing so, the legitimate effectiveness of SIM-PBL can be more critically evaluated.
6. ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2011-0009627).
![]()
![]()
REFERENCES
- Profetto-McGrath, J. (2005) Critical thinking and evidence-based practice. Journal of Professional Nursing, 21, 364-371. doi:10.1016/j.profnurs.2005.10.002
- Solomon, S. (2011) Problem-based learning. In: Bradshaw, M.J. and Lowenstein, A.J., Eds., Innovative Teaching Strategies in Nursing and Related Health Professions, 5th Edition, Jones and Bartlett, Sudbury.
- Hwang, S.Y. and Kim, M.J. (2006) A comparison of problem-based learning and lecture-based learning in an adult health nursing course. Nurse Education Today, 26, 315-321. doi:10.1016/j.nedt.2005.11.002
- Harden, R.M. and Davis, M.H. (1998) The continuum of problem-based learning. Medical Teacher, 20, 317-322. doi:10.1080/01421599880733
- Hovancsek, M.T. (2007) Using simulations in nursing education. In: Jeffries, P.R., Ed., Simulation in Nursing Education, National League for Nursing, New York, 1-9.
- McGaughey, J. (2009) Acute care teaching in the undergraduate nursing curriculum. Nursing in Critical Care, 14, 11-16. doi:10.1111/j.1478-5153.2008.00303.x
- Thompson, T.L. and Bonnel, W.B. (2008) Integration of high-fidelity patient simulation in an undergraduate pharmacology course. Journal of Nurse Education, 47, 518- 521. doi:10.3928/01484834-20081101-10
- Gantt, L.T. and Webb-Corbett, R. (2010) Using simulation to teach patient safety behaviors in undergraduate nursing education. Journal of Nursing Education, 49, 48- 51. doi:10.3928/01484834-20090918-10
- Lee, W.S., Cho, K.C., Yang, S.H., Roh, Y.S. and Lee, G.Y. (2009) Effect of problem-based learning combined with simulation on the basic nursing competency of nursing students. Journal of Korean Academy of Fundamental Nursing, 16, 64-72.
- Kameg, K., Howard, V.M., Clochesy, J., Mitchell, A.M. and Suresky, J.M. (2010) The impact of high fidelity human simulation on self-efficacy of communication skills. Issues in Mental Health Nursing, 31, 315-323. doi:10.3109/01612840903420331
- Liaw, S.Y., Chen, F.G., Klainin, P., Brammer, J., O’Brien, A. and Samaraseker, D.D. (2010) Developing clinical competency in crisis event management: An integrated simulation problem-based learning activity. Advances in Health Sciences Education, 15, 403-413. doi:10.1007/s10459-009-9208-9
- Steadman, R.H., Coates, W.C., Huang, Y.M., Matevosian, R., Larmon, B.R., McCullough, L. and Ariel, D. (2006) Simulation-based training is superior to problem-based learning for the acquisition of critical assessment and management skills. Critical Care Medicine, 34, 151-157. doi:10.1097/01.CCM.0000190619.42013.94
- Kim, J.Y. and Choi, E.Y. (2008) Learning element recognition and academic achievement of nursing student receiving PBL with simulation education. Journal of Korean Academy of Adult Nursing, 20, 731-742.
- Chu, M.S., Hwang, Y.Y. and Park, C.S. (2006) Development and application of PBL module using simulator. Journal of Korean Academy of Fundamental Nursing, 13, 182-189.
- Ackley, B.J. and Ladwig, G.B. (2010) Nursing diagnosis handbook. A guide to planning care. Mosby, St. Louis
- Korean Centers for Disease Control and Preventions. (2009) Korea national health and nutrition examination surveys. http://knhanes.cdc.go.kr
- Bandura, A. (1997) The anatomy of stages of change. American Journal of Health Promotion, 12, 8-10. doi:10.4278/0890-1171-12.1.8
- Walton, H.J. and Matthews, M.B. (1989) Essentials of problem-based learning. Medical Education, 23, 542-558. doi:10.1111/j.1365-2923.1989.tb01581.x
- Distler, J. (2008) Problem-based learning: an innovative approach to teaching physical assessment in advanced practice nursing curriculum. International Journal of Nursing Education Scholarship, 5, Article 23. doi:10.2202/1548-923X.1577
- Ko, I.S., Kim, H.S., Kim, I.S., Kim, S.S., Oh, E.G., Kim, E.J., Lee, J.H. and Kang, S.W. (2010) Development of a scenario and evaluation for simulation learning of care for patients with asthma in emergency units. Journal of Korean Academy of Fundamental Nursing, 17, 371-381.
- Kern, D.H., Mainous, A.G., III, Carey, M. and Beddingfield, A. (2011) Simulation-based teaching to improve cardiovascular exam skills performance among third-year medical students. Teaching and Learning in Medicine, 23, 15-20. doi:10.1080/10401334.2011.536753
NOTES
*Corresponding author.

