Journal of Biomedical Science and Engineering
Vol.5 No.11(2012), Article ID:24777,3 pages DOI:10.4236/jbise.2012.511086
Microbiological flora of mobile phones of resident doctors
![]()
1Department of Microbiology, Dr SC Government Medical College, Nanded, India
2Department of Community Medicine, Datta Meghe Institute of Medical Sciences, Nagpur, India
Email: zahirquazi@rediffmail.com
Received 23 December 2011; revised 22 February 2012; accepted 10 August 2012
Keywords: Health Care Personnel; Mobile Phones; Nosocomial Infection
ABSTRACT
Background: Many studies revealed that devices like stethoscope, mobile phones can act as an important source of microbes capable of causing nosocomial infections. Hence there is need of defining their role in spreading infection, so that we can take some preventive measures against it. Aims: To screen the mobile phones of resident doctors and perform microbeological study of the organisms isolated. Setting: Resident doctors working at Tertiary Care Hospital. Methods: Swabs of 50 mobile phones of resident doctors were taken by sterile cotton swab and inoculated on Blood agar, MacConkey agar, Sabaraud’s dextrose agar. Isolated organisms were processed according to standard protocol. Results: Swabs of mobile phones of 50 resident doctors were analyzed for presence of micro-organisms. Out of the 50 samples, 30 (60%) were contaminated with micro-organisms. 32 micro-organisms were isolated from 50 mobile phones as shown in table 3. Among 32 isolates, Coagulase negative Staphylococci 23 (71.87%) was the dominant organism followed by Diphtheroids 7 (21.87%), Aspergillus niger 2 (6.25%). Also proportion of contamination of mobile phones of male resident doctors was more than female resident doctors. Conclusion: Mobile phones may act as a potential source of micro-organisms and spread nosocomial infections. Hence proper infection control practices like proper hand washing, decontamination of mobiles should be routinely practiced.
1. INTRODUCTION
Today mobile phones have become an essential accessory of life. While working in hospital mobile phones of health care personnel often become contaminated with micro-organisms. These mobile phones could act as a reservoir of infection which may facilitate patient to patient transmission of micro-organisms in hospital setting.
Doctors and healthcare staff working in intensive care units and operating units are highly exposed to deadly micro-organisms. These mobile phones used by health care personnel often become carriers and spread microorganisms wherever they are taken along.
Colonized micro-organisms in the devices of health care personnel may be transmitted to patient even if patients do not have direct contact with mobile phones. Nosocomial infection may be caused in patients with weak immune system but micro-organisms may not cause any harm in patients with strong immune system [1].
Hence the present study was undertaken with objecttives to screen mobile phones of health care personnel for the presence of micro-organisms, to isolate and identify the micro-organisms with the help of standard laboratory techniques, and to compare micro-organisms profile among male and female resident doctors.
2. MATERIALS & METHODS
This was a cross-sectional study. Swabs of mobile phones of 50 resident doctors were taken. All resident doctors of all age group and of both genders who were ready for consent were included in this study. This study was carried out from 1st January 2011 to 28th February 2011 at Tertiary Care Hospital.
Sterile cotton swab moistened with sterile normal saline was used to collect the specimen. Swab was rotated on the sides, back and over the keypad of mobiles [2]. The swabs were immediately inoculated and streaked onto blood agar, MacConkey’s agar, Sabaraud’s dextrose agar. Plates were incubated aerobically at 37˚C for 24 hrs. Isolated organisms were processed according to colony morphology, gram stain. Organisms were identified according to standard protocol [3]. Tests for identification of gram positive cocci included Catalase, Coagulase (slide and tube). Fungus growth was observed for 2 weeks [1].
3. RESULTS
A total of 50 mobile phone swabs of resident doctors were analyzed for presence of micro-organisms. It was revealed that of the 50 mobile phones, 30 (60%) were contaminated with micro-organisms (Table 1).
32 micro-organisms were isolated from 50 mobile phones as shown in Table 2. Among 32 isolates, Coagulase negative Staphylococci 23 (71.87%) was dominant organism followed by Diphtheroids 7 (21.87%), Aspergillus niger 2 (6.25%).
In 28 swabs the growth was monomicrobial while in two swabs growth was polymicrobial.
In this study among 50 resident doctors, 25 were male resident doctors and 25 were female resident doctors. Out of 25 male resident doctors, mobile phones of 19 (76%) male doctors were contaminated and out of 25 female resident doctors, 11 (44%) mobile phones were contaminated. On applying appropriate statistical test i.e. Chi-square test, this difference was significant (Table 3). It suggested that proportion of contamination of mobile phones of male resident doctors was more than contamination of mobile phones of female resident doctors.
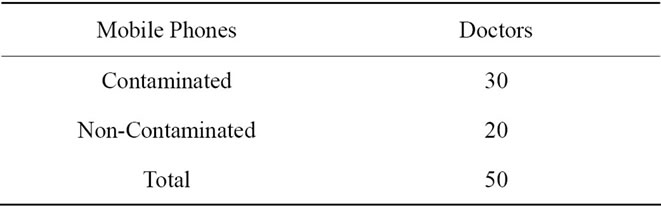
Table 1. Microbial contamination of mobile phones of Resident doctors.
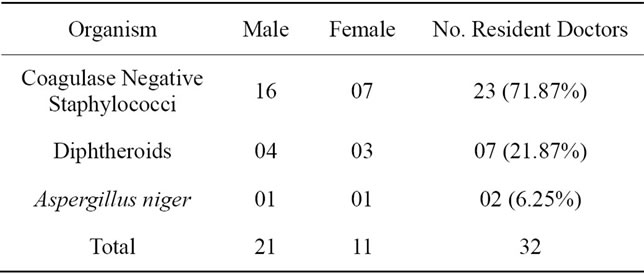
Table 2. Organisms isolated from mobile phones of resident doctors.

Table 3. Organisms isolated among Male and Female resident doctors.
4. DISCUSSION
The present study was conducted at Tertiary Care Hospital. A total of 50 mobile phone swabs of resident doctors were analyzed for the presence of micro-organisms. It was revealed that of the 50 mobile phones, 30 (60%) were contaminated with micro-organisms. It is similar to studies conducted by Killic I. H. et al. and Datta P. et al. who found contamination of mobile phones 61.3% and 72% respectively. [1,2] While studies conducted by Karabay et al., Ulger F. et al., Tambekar D. H. et al. found higher rate of mobile contamination than our study i.e. 90.98%, 94.5%, 95% respectively [4-6].
Among 348 contaminated mobile swabs, 30 (06%) were of doctors, 37 (7.40%) were of interns, 128 (25.60%) were of M.B.B.S. students attending clinics and 153 (30.60%) were of nurses. On applying appropriate statistical test (Chi-square test) p value was that means this difference was significant.
In this study, only one type of organism was found in 326 mobile phone swabs. While two types of organisms were reported in 22 mobile swabs and no organisms were found in 152 mobile swabs. Study done by Chawala et al. reported that in health care workers, the majority of mobile phones showed polymicrobial growth i.e. 40% mobile phones showed two types of organism, 27.5% showed the presence of three or more types of organisms and only 25% were monomicrobial [7].
Isolation of Coagulase negative Staphylococci was predominant in our study (Table 3) i.e. 58.92% which is comparable with study of Karabay O et al., Killic I. H. et al. and Ulger F. et al. who found Coagulase negative Staphylococci isolation 68.4%, 60% and 58.96% respectively [1,4,5]. Study by Datta P. et al. found less isolation of coagulase negative Staphylocci i.e. 13.19% and reported Staphylococcus aureus (36%) as the dominant pathogen [2]. Similarly study conducted by Tambekar D. H. et al. found Staphylococcus aureus as the major pathogen (20%) [6].
In our study Pseudomonas aeruginosa (Table 3) isolation was less i.e. 3.24% which is comparable to studies conducted by Pandey A. et al. and Karabay O. et al., Chawala et al. who reported the isolation of Pseudomonas species from mobile phones 3.6%, 2.7% and 2.5% respectively[4,7,8].
In our study isolation of Escherichia coli & Klebsiella pneumoniae was (Table 3) 0.81% each. Higher rate of isolation i.e. Escherichia coli (08%) & Klebsiella pneumoniae (10 %) has been reported by Tagoe et al. [9].
Fungal growth in our study was found to be (Table 3) 12.43% while study by Ulger & Killic reported fungal growth in 7.49% and 1.54% respectively [1,5].
In this study among 50 resident doctors, 25 were female resident doctors and 25 were male resident doctors. Out of 25 male resident doctors, mobile phones of 19 (76%) male doctors were contaminated and out of 25 female resident doctors, 11 (44%) mobile phones were contaminated. On applying appropriate statistical test i.e. Chi-square test, p value was 0.0032 that means this difference was significant. It suggested that proportion of contamination of mobile phones of male resident doctors was more than contamination of mobile phones of female resident doctors.
Study by Tambekar et al. reported that 96% swabs from male and 93% from female doctor’s mobile phones were contaminated. And out of 90 isolated pathogens, 62 (72%) pathogens were found on male doctor’s mobile phones while 25 (28%) on female doctor’s mobile phones. This study suggested that contamination of male doctor’s mobile phones was more than female doctor’s mobile phones, it might be due to the reason that females keep their mobiles in purses and use less frequently during their duties. On the other hand, male doctors keep their mobiles in their pockets and use frequently anywhere, any time whenever it is needed and thus contaminated and played an important role in transmission of pathogens [6].
5. CONCLUSIONS
This study emphasizes that mobile phones act as a carriers & may play an important role in spreading of nosocomial infection.
Doctors are often exposed to pathogenic micro-organisms during hospital work & they may carry these micro-organisms on their mobile phones and act as a source of infection to others.
Restricting mobiles in health care set up is a debatable issue as use of mobile is unavoidable in emergencies. Hence regular surveillance and development of effective preventive strategies such as regular decontamination of mobile phones with alcohol disinfectant to reduce the burden and use of antimicrobial additive materials are required. We could easily avoid spreading bacterial infections by using regular cleaning agents and rearranging our environment. In conclusion, it can be said that hand hygiene is greatly overlooked and under-emphasized in health care settings as many preach but few follow it.
![]()
![]()
REFERENCES
- Killic, I.H., Ozaslan, M., Karagoz, I.D., Zer, Y. and Davatoglu, V. (2009) The microbial contamination of mobile phones used by healthcare staff. Pakistan Journal of Biological Sciences, 12, 882-884.
- Datta, P., Rani, H., Chander, J. and Gupta V. (2009) Bacterial contamination of mobile phones of health care workers. Indian Journal of Medical Microbiology, 27, 279-281. doi:10.4103/0255-0857.53222
- Collee, J.G., Miles, R.S. and Wan, B. (1996) Tests for the identification of bacteria. In: Collee, J.G., Fraser, A.G., Marmion, B.P. and Simmons, A., Eds., Mackie and MacCartney Practical Medical Microbiology, 14th Edition, Churchill Livingstone, Edinburg, 131-150.
- Karabay, O., Kocoglu, E. and Tahtaci, M. (2007) The role of mobile phones in the spread of bacteria associated with nosocomial infections. Journal of Infection in Developing Countries, 1, 72-73.
- Ulger, F., Esen, S., Dilek, A., Yanik, K., Gunaydin, M. and Leblebicioglu, H. (2009) Are we aware how contaminated our mobile phones with nosocomial pathogens? Annals of Clinical Microbiology and Antimicrobials, 8, 1476-1487.
- Tambekar, D.H., Gulhane, P.B., Dahikar, S.G. and Dudhane, M.N. (2008) Nosocomial hazards of doctor’s mobile phones in hospitals. Journal of Medical Sciences, 8, 73-76. doi:10.3923/jms.2008.73.76
- Chawla, K., Mukhopadhayay, C., Gurung, B., Bhate, P. and Bairy, I. (2009) Bacterial “cell” phones: Do cell phones carry potential pathogens? Online Journal of Health and Allied Sciences, 8, 8.
- Pandey, A., Asthana, A.K., Tiwari, R., Kumar, L., Das, A. and Madan, M. (2010) Physician accessories: Doctor, what you carry is every patient’s worry? Indian Journal of Medical Microbiology, 53, 711-713.
- Tagoe, D.N., Gyande, U.K. and Ansah, E.O. (2011) Bacterial contamination of mobile phones: When your mobile phone could transmit more than just a call. WebmedCentral Microbiology, 2, WMC002294.

