Journal of Cancer Therapy
Vol.5 No.4(2014), Article ID:45120,7 pages DOI:10.4236/jct.2014.54046
Chondrosarcoma of the Hand: A Literature Review
Daniele Stomeo1, Antonio Tulli2, Antonio Ziranu1, Federica Mariotti1, Giulio Maccauro1*
1Orthopedic Oncologic Unit, Department of Geriatrics, Neuroscience and Orthopedics, Catholic University, Rome, Italy
2Hand Surgery Unit, Department of Geriatrics, Neuroscience and Orthopedics, Catholic University, Rome, Italy
Email: *giuliomac@tiscali.it
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 27 February 2014; revised 25 March 2014; accepted 2 April 2014
ABSTRACT
Chondrosarcoma (CS) is a malignant neoplasm of mesenchymal origin characterized by the formation of cartilaginous matrix by neoplastic cells. It is very variable in presentation, clinical, genetic and anatomo-pathological features. CS is more often found in the pelvis and the proximal long bones (femur, humerus). Localization to the small bones of the hand is very rare and it represents a diagnostic and therapeutic challenge. CSs are malignancies resistant to both radiation and chemotherapy [1]. Surgical treatment is the only mean available. As opposed to CSs located elsewhere, CS of the hand is characterized by local recurrence and very low metastatic potential. In order to definitely set a diagnosis of chondrosarcoma in this region, comparison of histological and radiological findings is paramount. The principle goal of surgery shall be minimizing functional impairment. This provides the rationale for performing curettage, local adjuvant therapy and bone grafting in low-grade lesions.
Keywords:Chondrosarcoma, Chondrogenic Tumour, Hand, Finger, Digit, Treatment, Surgery, VEGF

1. Introduction
Chondrosarcoma (CS in the text) is a malignant tumour of mesenchymal origin characterized by the formation of cartilaginous matrix by neoplastic cells. It is very variable in presentation, clinical, genetic and anatomopathological features. It can be both primary and secondary. Several subtypes have been described. CS usually presents in the conventional or typical form, i.e., primary and central.
In order to establish correct subtypes and grading, histological findings should always be correlated to imaging [2] [3] .
CS is more often found in the pelvis and the proximal long bones (femur, humerus). Localization to the small bones of the hand is very rare and it represents a diagnostic and therapeutic challenge. Most tumours of the hands, such as enchondroma, are of benign origin. In this region CSs are the most frequent malignant bone neoplasms, and 50% of the described lesions are located in the phalanges [4] [5] . As opposed to CSs located elsewhere, CS of the hand is characterized by local recurrence and very low metastatic potential [4] [6] . On these bases, a new conservative approach, followed by careful post-operative follow-up, has been proposed [4] . The aim of this study was to review the literature on the hand chondrosarcoma with the aim of giving the current therapeutic management.
2. Epidemiology
Chondrosarcoma is the third most common primary malignancy of the bone after multiple myeloma and osteosarcoma; it accounts for 20% of bone primary sarcomas; it affects men more frequently than women (M:F = 2:1). It is morecommon among older adults. When found in children, prognosis is usually poorer [7] . In our review of literature we found a slight female preponderance in case reports and series regarding CS of the hand, whilst the mean age at presentation was similar to that of CS located elsewhere.
90% of CSs are described as conventional CS (i.e. primary and central); about 90% of these are low to intermediate grade (Grade 1 or 2 according to WHO classification) [8] .
CS is more often found in the pelvis and the proximal long bones (femur, humerus). Very rare is the localization to the small bones of the hands. Nigrisoli et al. [9] and Unni et al. [10] separately reported a total of 1401 cases of CS, among these only 1.25% affected the hands.
Despite this, CS is the most common primary malignant bone neoplasm in the hand [11] , and 50% of the described lesions are found in the phalanges [4] [5] .
3. Materials and Methods
The following electronic databases have been searched: The Cochrane Central Library (CENTRAL), MEDLINE/ Pubmed (from 1958 to February 2014), and EMBASE/Ovid. The search strategies for the different electronic databases (using a combination of controlled vocabulary and text word terms) were: Chondrosarcoma OR Chondrosarcomas OR CHS OR CS OR Chondrogenic sarcoma OR Chondrogenic Sarcomas OR Cartilage neoplasms OR Cartilage Sarcoma OR Cartilage Sarcomas; Hand OR Finger OR Metacarpal OR Digit OR Phalanx OR small bones.
We found 81 case reports and review articles, 15 of which were excluded because they were not written in English, Italian, Spanish or French. Our bibliography only includes the articles we found most useful.
4. Anatomopathology
Cs shows 5 histological distinctive features: 1) Production of malignant cartilage, 2) Medullary cavity infiltration, 3) Osseous trabeculae entrapment, 4) Haversian systems infiltration, 5) Normal bone destruction. In spite of these, it is very difficult to distinguish enchondroma from chondrosarcoma, since the former shows several of these features, especially when located in the hands.
According to the localization in the bone segment, CS can be described as “central” when it originates form the medullary cavity, “peripheral” and “periosteal or iuxtacortical” when it grows from the bone surface. The first is nearly always primary and is the most common type of CS; the second is more rare and generally derives from degeneration of pre-existing tumours such as osteochondromas [12] .
CSs usually present in the conventional or typical form, i.e. primary and central. CS variants are rare: Dedifferentiated CS, deriving from the transformation of a low-grade CS into a high-grade CS, generally acquires histological features of other mesenchymal sarcomas and forms areas of non-collagen-producing cells; Mesenchymal CS, a very aggressive variant characterized by highly cellular solid areas, populated by primitive mesenchymal cells; Clear cell CS, a low-grade lesion in which the clear cell appearance is due to the consistent amount of intracellular glycogen; Myxoid CS, characterized by myxoid matrix, slow-growing and high incidence of local recurrence.
Chondrosarcomas are a challenge to the pathologist, since benign and low-grade malignant chondrogenic lesions often show overlapping features.
Due to the ambiguous behaviour of CSs, the World Health Organization (WHO) proposed a grading system divided in 4 grades (borderline, low, intermediate and high grade) based on the work of Evans et al. [13] . The authors consider 7 variables that have been shown to correlate with patients’ prognosis: 1) Cellularity, 2) Size of nuclei, 3) Nuclear hyperchromasia, 4) Bior Tri-Nucleation, 5) Nuclear and cellular polymorphisms, 6) Mitoses, 7) Presence of Myxoid matrix.
Grade 0.5—Borderline: cannot be differentiated histologically from an enchondroma, but shows a more aggressive radiological aspect.
Grade 1—Low: with respect to enchondroma it shows slightly higher cellularity, hyperchromasia and increased size of nuclei. No polymorphisms, no myxoid matrix, rare mitoses.
Grade 2—Intermediate: higher cellularity, size of nuclei, hyperchromasia, polymorphisms, bi-nucleations and number of mitoses, focally present myxoid matrix.
Grade 3—High: as the previous, with diffused myxoid matrix and increased number of mitoses [2] (Figure 1).
Recent studies have investigated the use of VEGF as a marker capable to help the pathologist in distinguishing between lowand high-grade lesions. Other markers, such as PDGF, TGF b 2, Ki-67, or p53 have been correlated to tumour aggressiveness but not to tumour grading.
It is known that switchingtoneo-angiogenesisis amain factor in malignant tumour growth, and this has been observed for chondrogenic tumours as well [14] Radial growthover 3mm3 requires neovascularisation [15] . Falcone et al. demonstrated the presence of a correlation between VEGF expression and tumour grading: VEGF was found predominantly in high-grade malignancies. This new evidences could help to correctly identify lowand high-grade lesions and lead the therapeutic approach.
5. Clinical Presentation and Diagnosis
The main symptom is progressive swelling, generallyassociated with pain [16] (Figure 2(a)). Many patients have symptoms for several years before being visited by a surgeon. Because of the relative indolence and frequent misdiagnosis of these tumours, Gohla et al. [17] reported that the length of time between the first symptoms and the first surgery ranged from 2 months to 30 years.
The main differential diagnosis is enchondroma; other possibilities are: ganglion, bursa, gout, rheumatoid arthritis, cyst, onychomatricoma and chondromyxoid fibroma (very rare in the hands) [16] . From a clinical point of view enchondroma could be easily distinguished from CS because the former rarely causes pain or swelling, except in case of fractures.

Figure 1. High-grade chondrosarcoma of the III digit, infiltrating the II digit and the soft tissues of the right hand. Cartilaginous (black arrow), myxoid (arrowhead) and necrotic (white arrow) areas can be seen.
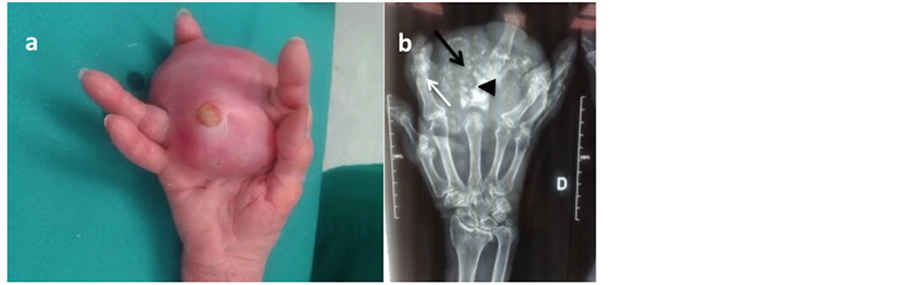
Figure 2. (a) High-grade chondrosarcoma of the III digi. At the clinical examination (Figure N a.) it presented as a huge. ulcerated soft tissue mass; it was 7 cm in diameter, fixed to superficial and deep llayers and painful. (b) At the preoperative roentgenograms the cortex of the proximal phlanx of the III digit was disrupted (arrowhead); several calcificaltions were present in the soft-tissue mass (black arrow), and some areas of osteolysis could be seen in the II digit (white arrow).
Even though we know that there is an increased risk of developing CS in multiple enchondromatosis, this seldom occurs in the hands [18] . We found reports including CSs arising in patients with Ollier’s disease [3] and Maffucci’s Syndrome [19] affecting the hands: the former being multiple enchondromatosis generally with unilateral predominance, the lattermultiple enchondromatosis associated with multiple haemangiomas.
Careful attention must be paid to patients with chondrogenic lesions which are painful or active after growth plates closure.
6. Radiological Diagnosis
Conventional radiograms provide very useful information about morphology, intra-lesional calcifications (popcorn-like pattern, arch-ring pattern), cortical erosion and periosteal reaction, when present [20] [21] (Figure 2(b)). Bone scan didn’t prove itself necessary, even though it may detect calcifications, periosteal reaction or pathologic fractures when they are not demonstrated by other techniques. MRI imaging is of fundamental importance since, in contrast to CT imaging, it allows detection of the borders between pathologic and normal bone, intramedullary extension, extra-osseous extension within soft-tissues or nearby articulations, dislocation of neuro-vascular bundles [22] [23] , CT scan is otherwise the best technique to detect cortical erosion [24] .
In the series of the Mayo Clinic, reporting 111 chondrosarcomas of small tubular bones, endosteal erosion, cortical destruction and expansion were present in 90% of cases, associated soft-tissue mass was observed in 80% of cases; the lesions were generally poorly marginated (79%); periosteal reaction and cortical thickening were rare (14% and 11% of cases respectively) [25] . Similar findings were reported by Cawte T. G. et al. [26] .
7. Discussion
Chondrosarcoma of the hands, although rare, represents the most frequent malignancy in this site. It shares many histological and radiological features with enchondroma, the most frequent benign tumour of the hand, thus differential diagnosis is often difficult. Indeed, it is well accepted that enchondromas, especially when affecting small bones, show hypercellularity, some myxoid changes, pleomorphisms and bi-nucleated cells, all of them being features used in the diagnosis of CSs.
In order to definitely set a diagnosis of chondrosarcoma in this region, comparison of histological and radiological findings is paramount. In the series reported by Ogose A. et al. [25] 14 lesions had none of the histologic features used to differentiate between CS and enchondroma, but they were diagnosed as CSs grade 1 because of their aggressive appearance in radiographs. On the contrary, 2 lesions were compatible with enchondroma on radiograms, but were diagnosed as CS grade 1 because of their histological aspect.
Even though radiology alone does not suffice for diagnosis, cortical destruction, soft-tissue mass and permeative pattern of growth seem to identify correctly CSs [27] .
Biopsy represents another crucial problem, since little specimens (above all FNAB samples) have low sensibility in distinguishing between enchondroma and chondrosarcoma [25] [28] [29] .
In conclusion a diagnosis of CS is justified even when histology is not supportive, if clinical and radiographical behaviour is suggestive.
Pain also could be misleading and cannot be used to surely differentiate benign from malignant chondrogenic lesions; Takigawa et al. [30] reported that 15.8% of patients with enchondroma of the hands developed pain.
CSs are malignancies resistant to both radiation and chemotherapy [1] . Surgical treatment is the only mean available. Different approaches are used depending on tumour grade [31] . For this reason it is important to correctly establish the grading of the malignancy. Recent studies have investigated the use of VEGF as a marker capable to help the pathologist in distinguishing between lowand high-grade lesions. Other markers have been correlated to tumour aggressiveness but not to grading. According to these data, Falcone et al. [32] formulated an algorithm for chondrosarcoma treatment. They propose intralesional excision with local adjuvants in VEGFnegative cases and wide excision in cases with VEGF positivity. In tumors with PDGF, TGF b 2, Ki-67, or p53 expression, more aggressive chemotherapeutic agents should be considered.
In recent years several clinical studies have stressed the peculiar pathologic behaviour of CSs of the hand in comparison to chondrosarcomas located elsewhere [4] [5] [33] .
Bovée et al. [5] reported a series of 35 patients affected by phalangeal CS; only 10 of the 28 patients examined at follow-up developed local recurrence, and none had metastases. He also reviewed the literature for digital CS and among 84 patients described until 1999 only 2 reported metastases. The authors conclude that phalangeal CS is locally aggressive but has very low metastatic potential.
Following these observations Mankin et al. [6] postulated that CS of the hand could be a different and more benign pathology compared to its appendicular skeleton counterparts.
Mittermayer et al. [4] reviewed a series of 13 Grade 1 CSs of the hand; the patients were divided into 2 groups and followed up for a mean of 99.8 months; group 1 (8 cases) underwent curettage and reconstruction with cancellous bone; group 2 (5 cases) underwent wide resection. No case of recurrence was observed in the second group, and only 1 patient had recurrence after 18 months. No one developed metastases. On this basis the authorssuggest intralesional resection by curettage and bone grafting as the preferential treatment for hand CSs.
Conservative surgery with curettage and bone grafting has been proposed to be effective on recurrence treatment by Exner et al. [34] , with no augmented risk for metastases.
8. Conclusion
Chondrosarcoma located in the hands is a diagnostic and therapeutic challenge. Distinction between benign and malignant lesions is not always easy; the same could be said about lowand high-grade lesions. Bovée et al. [5] demonstrated that the WHO grading system is not useful for diagnostic purpose in phalangeal chondrosarcomas. Indeed, these neoplasms are believed to have a more benign behaviour compared to CSs located elsewhere: they are locally aggressive, but show poor tendency to metastasize. The principle goal of surgery shall be minimizing functional impairment. This provides the rationale for performing curettage, local adjuvant therapy and bone grafting in low-grade lesions. This treatment has proven itself useful even in the management of local recurrence. High-grade lesions should be treated with radical resection.
References
- Eriksson, A.I., Schiller, A. and Mankin, H.J. (1980) The Management of Chondrosarcoma of Bone. Clinical Orthopaedics and Related Research, 153, 44-66.
- Bertoni, F., Bacchini, P. and Hogendoorn, P.C.W. (2002) Chondrosarcoma. In: Fletcher, C.D.M., Unni, K.K. and Mertens, F., Eds., World Health Organisation Classification of Tumours. Pathology and Genetics of Tumours of Soft Tissue and Bone. IARC Press, Lyon, 247-251.
- Miyawaki, T., Kinoshita, Y. and Iizuka, T. (1997) A Case of Ollier’s Disease of the Hand. Annals of Plastic Surgery, 38, 77-80. http://dx.doi.org/10.1097/00000637-199701000-00015
- Mittermayer, F., Dominkus, M., Krepler, P., Schwameis, E., Sluga, M., Toma, C., Lang, S., Grampp, S. and Kotz, R. (2004) Chondrosarcoma of the Hand: Is a Wide Surgical Resection Necessary? Clinical Orthopaedics and Related Research, 424, 211-215. http://dx.doi.org/10.1097/01.blo.0000129164.91760.95
- Bovee, J.V., Van der Heul, R.O., Taminiau, A.H. and Hogendoorn, P.C. (1999) Chondrosarcoma of the Phalanx: A Locally Aggressive Lesion with Minimal Metastatic Potential: A Report of 35 Cases and a Review of the Literature. Cancer, 86, 1724-1732. http://dx.doi.org/10.1002/(SICI)1097-0142(19991101)86:9<1724::AID-CNCR14>3.0.CO;2-I
- Mankin, H.J. (1999) Chondrosarcomas of Digits: Are They Really Malignant? Cancer, 86, 1635-1637. http://dx.doi.org/10.1002/(SICI)1097-0142(19991101)86:9<1635::AID-CNCR3>3.0.CO;2-#
- Aprin, H., Riseborough, E.J. and Hall, J.E. (1982) Chondrosarcoma in Children and Adolescents. Clinical Orthopaedics and Related Research, 166, 226-232.
- Shmookler, B., Bickels, J., Jelinek, J., Sugarbaker, P. and Malawer, M. (2001) Bone and Soft-Tissue Sarcomas: Epidemiology, Radiology, Pathology and Fundamentals of Surgical Treatment. Musculoskeletal Cancer Surgery. Springer, The Netherlands, 3-35.
- Nigrisoli, M., Ferraro, A., De Cristofaro, R. and Picci, P. (1990) Chondrosarcoma of the Hand and Foot. La Chirurgia degli Organi di Movimento, 75, 315-323.
- Unni, K.K. (1996) Chondrosarcoma (Primary, Secondary, Dedifferentiated, and Clear Cell). In: Dahlin’s Bone Tumors. General Aspects and Data on 11,087 Cases. 5th Edition, Lippincott-Raven, Philadelphia, 71-108.
- Tos, P., Artiaco, S., Linari, A. and Battiston, B. (2009) Chondrosarcoma in the Distal Phalanx of Index Finger: Clinical Report and Literature Review. Chirurgie de la Main, 28, 265-269. http://dx.doi.org/10.1016/j.main.2009.02.002
- Greenspan, A., Jundt, G. and Remagen, W. (2007) Cartilage (Chondrogenic) Lesions. In: Differential Diagnosis in Orthopaedic Oncology. Lippincott Williams & Wilkins, Philadelphia.
- Evans, H.L., Ayala, A.G. and Romsdahl, M.M. (1977) Prognostic Factors in Chondrosarcoma of Bone: A Clinicopathologic Analysis with Emphasis on Histologic Grading. Cancer, 40, 818-831. http://dx.doi.org/10.1002/1097-0142(197708)40:2<818::AID-CNCR2820400234>3.0.CO;2-B
- Ricciardella, M.L., Rossi, E.D., Fadda, G., Graci, C., Spinelli, M.S., Falcone, G., Rosa, M.A. and Maccauro, G. (2011) Angiogenesis in Hand Chondroma: An Immunohistochemical Study. International Journal of Immunopathology and Pharmacology, 24, 143-147.
- Folkman, J. (1990) What Is the Evidence That Tumors Are Angiogenesis Dependent? Journal of the National Cancer Institute, 82, 4-6. http://dx.doi.org/10.1093/jnci/82.1.4
- Roberts, P.H. and Price, C.H. (1977) Chondrosarcoma of the Bones of the Hand. Journal of Bone & Joint Surgery, 59, 213-221.
- Gohla, T., Van Schoonhoven, J., Prommersberger, K.J. and Lanz, U. (2004) Chondrosarcomas of the Hand. Handchir Mikrochir Plast Chir, 36, 328-332. http://dx.doi.org/10.1055/s-2004-821242
- Goto, T., Motoi, T., Komiya, K., Motoi, N., Okuma. T., Okazaki, H., Takatori, Y., Tange, T. and Nakamura, K. (2003) Chondrosarcoma of the Hand Secondary to Multiple Enchondromatosis; Report of Two Cases. Archives of Orthopaedic and Trauma Surgery, 123, 42-47.
- Ramirez-Bollas, J., Padilla-Rosciano, A., Romero-Y, H.A., Lavin-Lozano, A.J., Medina-Castro, J.M., Dubon-Garcia, E. and Turcios-Cadenas, E.R. (2005) Maffucci’s Syndrome. Case Reports and Literature Review. Cir Cir, 73, 217-221.
- Aisen, A.M., Martel, W., Braunstein, E.M., McMillin, K.I., Phillips, W.A. and Kling, T.F. (1986) MRI and CT Evaluation of Primary Bone and Soft-Tissue Tumors. American Journal of Roentgenology, 146, 749-756. http://dx.doi.org/10.2214/ajr.146.4.749
- Feldman, F., Van Heertum, R., Saxena, C. and Parisien, M. (2005) 18FDG-PET Applications for Cartilage Neoplasms. Skeletal Radiology, 34, 367-374. http://dx.doi.org/10.1007/s00256-005-0894-y
- Bohndorf, K., Reiser, M., Lochner, B., Feaux de Lacroix, W. and Steinbrich, W. (1986) Magnetic Resonance Imaging of Primary Tumours and Tumour-Like Lesions of Bone. Skeletal Radiology, 15, 511-517. http://dx.doi.org/10.1007/BF00361046
- Hudson, T.M., Hamlin, D.J., Enneking, W.F. and Pettersson, H. (1985) Magnetic Resonance Imaging of Bone and Soft Tissue Tumors: Early Experience in 31 Patients Compared with Computed Tomography. Skeletal Radiology, 13, 134- 146. http://dx.doi.org/10.1007/BF00352084
- Pettersson, H., Gillespy, T., Hamlin, D.J., Enneking, W.F., Springfield, D.S., Andrew, E.R., Spanier, S. and Slone, R. (1987) Primary Musculoskeletal Tumors: Examination with MR Imaging Compared with Conventional Modalities. Radiology, 164, 237-241.
- Ogose, A., Unni, K.K., Swee, R.G., May, G.K., Rowland, C.M. and Sim, F.H. (1997) Chondrosarcoma of Small Bones of the Hands and Feet. Cancer, 80, 50-59. http://dx.doi.org/10.1002/(SICI)1097-0142(19970701)80:1<50::AID-CNCR7>3.0.CO;2-J
- Cawte, T.G., Steiner, G.C., Beltran, J. and Dorfman, H.D. (1982) Chondrosarcoma of the Short Tubular Bones of the Hands and Feet. Skeletal Radiology, 27, 625-632. http://dx.doi.org/10.1007/s002560050448
- Floyd, W.E. and Troum, S. (1995) Benign Cartilaginous Lesions of the Upper Extremity. Hand Clinics, 11, 119-132.
- Rinas, A.C., Ward, W.G. and Kilpatrick, S.E. (2005) Potential Sampling Error in Fine Needle Aspiration Biopsy of Dedifferentiated Chondrosarcoma: A Report of 4 Cases. Acta Cytologica, 49, 554-559. http://dx.doi.org/10.1159/000326205
- Jennings, R., Riley, N., Rose, B., Rossi, R., Skinner, J.A., Cannon, S.R., Briggs, T.W., Pollock, R. and Saifuddin, A. (2010) An Evaluation of the Diagnostic Accuracy of the Grade of Preoperative Biopsy Compared to Surgical Excision in Chondrosarcoma of the Long Bones. International Journal of Surgical Oncology, 2010, Article ID: 270195.
- Takigawa, K. (1971) Chondroma of the Bones of the Hand. A Review of 110 Cases. Journal of Bone and Joint Surgery, American Volume, 53, 1591-1600.
- Gitelis, S., Bertoni, F., Picci, P. and Campanacci, M. (1981) Chondrosarcoma of Bone. The Experience at the Istituto Ortopedico Rizzoli. Journal of Bone and Joint Surgery, American Volume, 63, 1248-1257.
- Falcone, G., Rossi, E.D., Maccauro, G., de Santis, V., Rosa, M.A., Capelli, A. and Fadda, G. (2006) Diagnostic Relevance of the Immunohistochemical Detection of Growth Factors in Benign and Malignant Cartilaginous Tumors. Applied Immunohistochemistry & Molecular Morphology, 14, 334-340. http://dx.doi.org/10.1097/00129039-200609000-00013
- Hatori, M., Watanabe, M., Kotake, H. and Kokubun, S. (2006) Chondrosarcoma of the Ring Finger: A Case Report and Review of the Literature. The Tohoku Journal of Experimental Medicine, 208, 275-281. http://dx.doi.org/10.1620/tjem.208.275
- Exner, G.U., Dumont, C.E., Malinin, T.I. and von Hochstetter, A.R. (2003) Recurrent Aggressive Chondrosarcoma of the Middle Phalanx of the Index Finger: Excision and Reconstruction with an Osteocartilaginous Allograft. Archives of Orthopaedic and Trauma Surgery, 123, 425-428. http://dx.doi.org/10.1007/s00402-003-0531-y
NOTES

*Corresponding author.

