Open Journal of Urology
Vol. 3 No. 2 (2013) , Article ID: 31403 , 6 pages DOI:10.4236/oju.2013.32018
Greenlight Photoselective Vaporisation of the Prostate in 133 High Surgical Risk Patients: A 5-Year Outcome Study
1Urology Service, Hospital Virgen de la Salud, Toledo, Spain
2LMR Group, Madrid, Spain
3Urology Service, Hospital Río Ortega, Valladolid, Spain
Email: naggoga@yahoo.es, martaromeromolina@hotmail.com, erubio2000@gmail.com, nachogomezgarcia@ymail.com, asampietro@ono.com, mafealfe@hotmail.com, agomez@imi.es
Copyright © 2013 Ignacio Gómez García et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received February 11, 2013; revised March 12, 2013; accepted March 22, 2013
Keywords: Greenlight; vaporisation; PVP; high risk; ASA
ABSTRACT
Greenlight photoselective vaporisation of the prostate (GPVP) is progressively becoming an established treatment in patients with LUTS because it is a minimally invasive technique that achieves efficient haemostasis, making it the ideal technique for patients at high surgical risk. Material and Methods: To study of 133 patients with an ASA surgical risk score of 3 or 4, undergoing GPVP, with an analysis of perioperative outcome, IPSS, Qmax, IIEF-5 and complications during a five-year follow-up. Results: At 5 years the mean annual improvement in IPSS was stable, and at 5 years there was a 15.2 point improvement versus the preoperative score (p < 0.05). The Qmax showed an improvement of 14.9 ml/sec and was maintained at five years after surgery (p < 0.05). No patients were transfused or suffered urinary incontinence. 2.25% suffered major complications and there were no deaths. 3.1% of patients suffered de novo urgency. In the 5-year follow-up, five patients had to be reoperated. The quality of sexual health assessed by IIEF-5 before the procedure was scored at 14 points; the 5-year follow-up covering the preoperative period and all revisions did not show any worsening in the IIEF-5 score (p > 0.05). Conclusions: Due to its physical characteristics, in our opinion GPVP is now the treatment of choice in patients at high surgical risk. In our series, the risk of major/minor complications and transfusions was much lower than the same risks in conventional techniques. The objective results (Qmax and quality of life questionnaire) are equivalent to conventional techniques and persist over a 5-year follow-up.
1. Introduction
Benign prostatic hyperplasia (BPH) occurs in over of half of all men aged over 60 years. Between 15% and 30% report LUTS (lower urinary tract symptoms) and 10% to 40% of them may require conventional surgery. The high incidence of per operative complications, associated morbidity and mortality and the need for blood transfusion in about 4% of patients, often led to high surgical risk patients having to live with a permanent indwelling catheter. The introduction and development of minimally invasive techniques (MIT) in the surgical treatment of BPH mean that high risk patients can now be treated, because of the low incidence of per operative complications, minimal blood loss, fast recovery and results that are very similar to conventional techniques.
2. Material and Methods
Between May 2006 and May 2011 we performed GPVP with 80 or 120 W laser on 615 patients diagnosed with BPH. Patients with a surgical risk of 3 and 4 according to the American Society of Anaesthesiologists (ASA) classification were included in the study. Patients with less than one year of follow-up were not included.
We performed a descriptive statistical study of the data set using SPSS v.15, evaluating side effects, complications, IPSS, IIEF-5, maximum flow, pre-operatively and at one week, one month, three months, six months, one year, two years, three years and five years.
Also performed statistical analysis with Student’s T test (95% confidence interval), analyzing in IPSS, Qmax and IIFE-5, improvement per year compared to baseline.
3. Results
The analysed group consisted of 133 patients, 89.4% (119) with lower urinary tract symptoms secondary to BPH, and 10.6% (14) with LUTS secondary to prostate carcinoma that was biologically and biochemically stable.
Mean age was 77.8 years (57 - 84). 78.4% (105) had an ASA 3 classification and 21.6% (28) were classified as ASA 4. 93.3% (126) were on antiplatelet or anticoagulant therapy. 63 patients (47.36%) had an indwelling catheter. Of the 70 non-catheterised patients, 75.71% (53) received combination treatment with an alpha-blocker and 5-ARI, 21.4% (15) received alpha-blocker treatment alone, and 2.4% received other treatments.
The preoperative assessment in all patients included: creatinine, routine blood test, PSA, urine culture, urological ultrasound, uroflowmetry, IPSS and IIEF-5. 17 (12.78%) urodynamic studies were performed in patients with severe urgency-frequency symptoms.
The mean PSA value, was 3.35 ng/ml with a range of 0.7 - 8.23 ng/ml. 38.6% (46) of patients underwent ultrasound guided biopsy, finding no evidence of malignancy in any patients. On ultrasound, mean prostate volume was 96.6cc, median 89cc (range 42cc - 157cc). Uroflowmetry alone was performed in all non-catheterised patients, finding a mean Qmax of 6.1 and a range of 3.8 to 11.6 ml/sec. Quality of life was assessed using the IPSS questionnaire, resulting in a mean score of 25.2 and a range of 17 to 31 points. The mean IIEF-5 score was 14 with a range of 7 to 25. The urodynamic study showed overactive bladder associated with lower urinary tract obstruction in 15 of the 17 patients studied.
An 80W PV Greenlight laser generator was used in 76 patients and a 120 W HPS Greenlight laser was used in 57 patients. Mean operating time was 107 minutes (range 36 to 140 minutes). Mean power used was 327,000 joules (range 116,000 to 600,000 joules).
Postoperatively all patients were catheterised with a three-way Ch 22 catheter and continuous bladder irrigation was performed with normal saline. Mean hospital stay was 27.9 hours excluding complications. Mean time of catheterisation was 36.7 hours in 122 patients. The catheter was kept in situ for 48 hours in 11 patients with a prostate volume of over 120cc. No patients required a blood transfusion. 2.25% had major post-operative complications: there was one case of pulmonary thromboembolism, one severe hyponatraemia secondary to reabsorption syndrome, and one case of pancreatitis. 4.5% of patients suffered AUR in the first 24 hours requiring catheterisation. All patients achieved spontaneous micturition after catheter removal.
At the week one check-up, all 133 patients were reviewed. 34.5% of patients reported urgency. 50.7% reported dysuria and 9.02% had mild initial haematuria. None reported incontinence.
All patients were reviewed after one month, finding urgency in 15.78%, dysuria in 12.7% and initial haematuria persisted in 1.5%. With regard to the IPSS, the mean score was 13.6, mean Qmax was 19.3 ml/sec and the IIEF-5 score was assessed as 15.9.
121 patients attended the post-operative visit at three months. Urgency persisted in 9% of patients, who were prescribed anticholinergics, 4.5% had dysuria and none reported initial haematuria. IPSS score improved with a mean of 12 points versus baseline. Mean Qmax was 24.3 ml/sec and the mean IIEF-5 score was 15.4.
At the six-month review, 114 patients were evaluated, finding urgency still present in 4.5% despite the anticholinergic treatment and 1.5% still had dysuria. The mean score for IPSS was 8, the mean Qmax was 26.2ml/sec and the mean IIEF-5 score was 16.2.
Twelve months after surgery, 95 patients attended for review. 3.1% reported urgency partly controlled with anticholinergics, 2.1% had dysuria, IPSS score was 8.6 points (70% improvement versus baseline), Qmax was 24.1 ml/sec (a fourfold improvement from baseline) and IIEF-5 was 14.2 points. One patient had to be reoperated because he had no improvement in his symptoms. One patient developed navicular fossa stenosis and underwent a dilatation protocol.
Two years after surgery, 81 patients were still under review. 1.23% still had urgency, IPSS score 9.1, mean Qmax was 23.7 and the mean IIEF-5 score was 14.7. Two patients were reoperated due to prostatic sclerosis. One patient was biopsied and diagnosed with prostate adenocarcinoma, Gleason score 8. He was treated with external radiotherapy and androgen blockade with goserelin and bicalutamide.
67 patients were followed-up at three years. There were almost no changes in IPSS (mean 8.8), Qmax (23.4 ml/sec) or IIEF-5(17.3 points). 1.4% suffered urgency. Three patients were biopsied, one for the first time and two underwent second biopsies due to increased PSA levels with a diagnosis of adenocarcinoma of the prostate. One patient was referred for radiotherapy and the other two were prescribed partial androgen blockade with leuprorelin.
48 patients were followed-up at 48 months. Mean IPSS was 9.3, mean Qmax was 21.9 ml/sec and IIEF-5 was 13.9.
60 months after surgery, 39 patients were still being followed up. Mean improvements for IPSS (9.2), Qmax (21.2 ml/sec) and IIEF-5 (14.1) remained stable. At 5 years one patient had to undergo vaporisation again for urinary retention (Figure 1).
There was a 13.2 point mean improvement in IPSS during the first three months, improving to 16.6 points at six months. From six months to 5 years the mean annual improvement in IPSS was stable and at 5 years there was a 16 point (64%) improvement versus the preoperative score. Qmax showed a three-month improvement of 18 ml/sec versus baseline, and an improvement of 15.1 ml/sec was maintained at five years after surgery, representing a 250% improvement.
No patients were transfused or suffered urinary incontinence. 2.25% suffered major complications and there were no deaths. 3.1% of patients suffered de novo urgency, which continued at 12 months after surgery, 1.2% at 24 months and 1.4% at three years. During the 5-year follow-up, 5 patients had to be reoperated (2 prostatic sclerosis, 1 urethral stricture and 2 patients with worsened IPSS), which represents a cumulative incidence of 3.75% of patients. The patient with navicualar fossa stenosis underwent a meatotomy and a balloon dilatation protocol (Table 1).
There was statistically significant improvement (p < 0.05) compared to baseline, the post-operatively and at all subsequent visits (5-year follow-up) in both IPSS and Qmax; while there was no statistically significant differences between baseline IIFE-5 and in the 5-year followup (Table 2).
4. Discussion
Traditionally, techniques for treating patients with LUTS have varied according to prostate volume. Prostatectomy and TURP are currently the gold standard. The wellknown associated comorbidity of these procedures has led to the introduction of MIT for BPH treatment, with the aim of reducing perioperative complications and minimising side effects while maintaining the same effectiveness as the conventional procedures. TURP is the
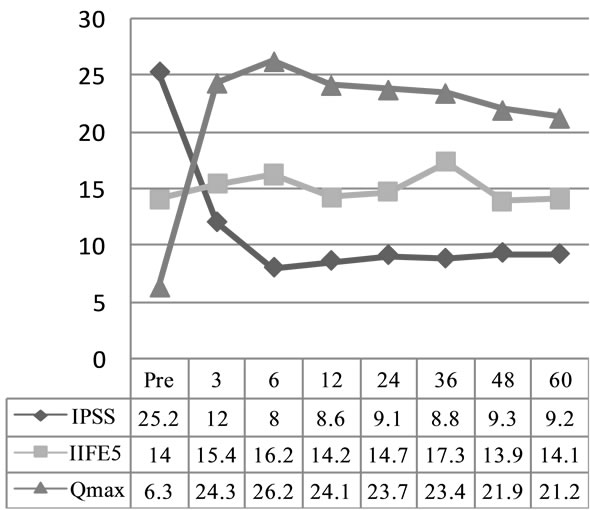
Figure 1. Evolution of IPSS, Qmax and IIFE-5.
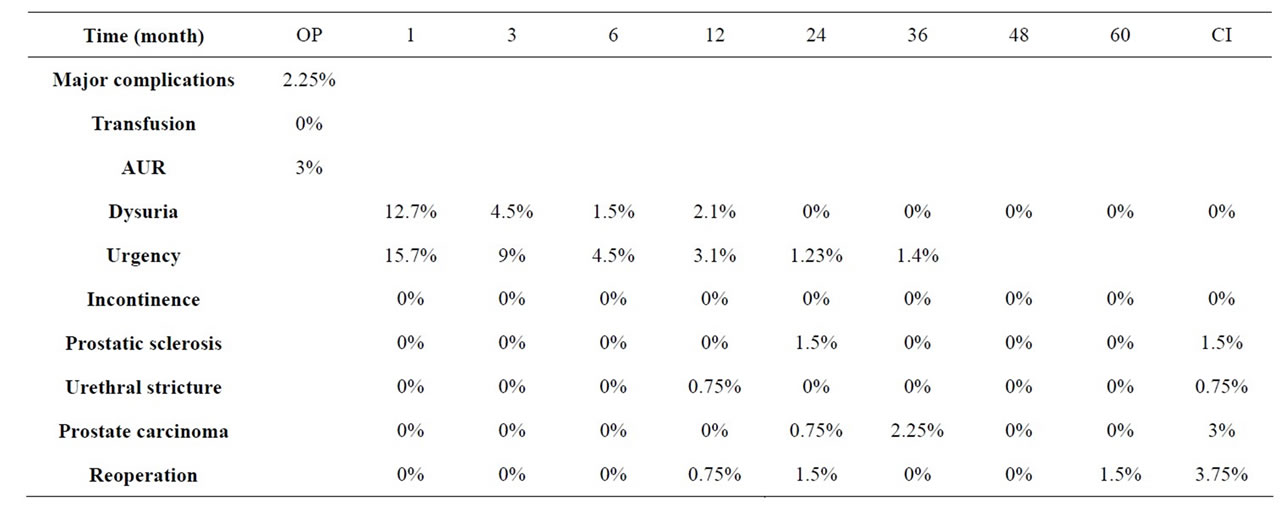
Table 1. Complications OP: surgery; CI: cumulative incidence; AUR: acute urinary retention.
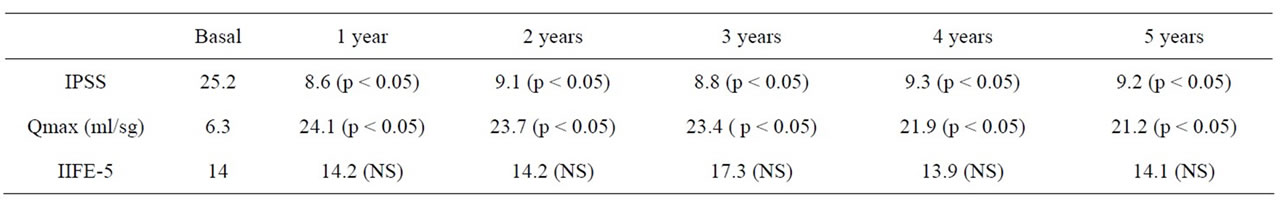
Table 2. Statistical analysis with T test compared each year with basal.
second most common surgery in the Western world but its frequency has fallen in the US from 350,000 procedures in 1986 to 200,000 in 1998, due to the greater efficacy of alpha-blocker treatment or in combination with 5-ARI [1]. The situation for BPH treatment today is that the number of TURPs performed is falling, and the indication for MIT is rising [2]. The TRIUMPH study has shown that the rate of surgery has fallen by 4.9%, probably as a result of a good use of alpha-blocker and combination therapy. This fact shows that surgery is increasingly indicated in elderly patients, with greater comorbidity and larger prostate volume [3,4].
The KTP laser (80 W) and the HPS and XPS lasers (120 - 180 W), on stimulation, the crystal emits a light beam with a 532 nm; this wavelength is absorbed by tissues with high oxyhaemoglobin content, such as the prostate [5]. GPVP is a technique with little blood loss, making it ideal in high-risk patients with significant comorbidity, and for patients who are on anticoagulant therapy.
Many studies report that the incidence of complications from TURP may stand at over 20% [1,6,7]. The risk of blood transfusion in risk-free TURP patients is about 2.5%. This percentage increases to 9% - 33% in high-risk patients according to the European Guidelines [2,5,8-11], with a 10% - 27% likelihood of readmission. Different publications have analysed the incidence of TURP complications and found frank intraoperative haematuria in up to 10.8% of cases [4], complications in 15% - 20%, reabsorption syndrome in 5%, reoperation required within the first 10 years in 10% - 15% [12], erectile dysfunction in about 13% in a multicentre study conducted by the AUA [13], mortality in up to 0.8%, morbidity ranging from 7% to 14% depending on the series [7], retrograde ejaculation in 75% [13], post-TURP syndrome in about 5%, perforation in 10%, reoperations in 12% [14]. Since TURP does not provide sufficient safety in BPH treatment in high-risk patients, several studies advocate and conclude that GPVP and HoLEP should be the techniques of choice for the treatment of prostatic symptoms in patients at high surgical risk [5,15].
The evolution of GPVP lasers using 80, 120 and 180 W systems has brought about improved effectiveness, safety, and the possibility of treating larger volume prostates [16,17], with clinical results similar to TURP, but with additional advantages, especially in patients with a high surgical and anaesthetic risk [11,18-20].
We performed a review of the literature and found four non-randomised studies comparing TURP and PVP [14]. In three of them the two techniques showed equal improvement in Qmax and IPSS, without statistically significant differences between them, although the TURP patients had significantly more adverse effects and PVP patients enjoyed better perioperative safety [21-24]. In another non-randomised study with a 12-month followup, Ruszat et al. [25] found no statistically significant differences between the two techniques with regard to PRV and IPSS, although there was more improvement in Qmax in the TURP group. They also found that hospital stay was shorter and complications were lower in the PVP group, although there were no differences between stenosis, reoperation or prostatic sclerosis. Cleynenbreugel et al. [11] reviewed some prospective studies comparing TURP and PVP and did not find any significant differences in terms of improved Qmax or IPSS, but PVP showed less morbidity and greater perioperative safety.
Bachmann et al., in a series involving 108 patients, reported that the procedure had minimal bleeding with improvement in Qmax and PRV of 75.4% and 186% respectively [22]. Shandu et al. studied 24 patients who underwent GPVP. IPSS improved 49% and Qmax improved 123% at one year [10]. Other studies have demonstrated the effectiveness and improvement in LUTS with a low rate of complications [17,20,21,26]. It has been shown that surgery with 120 W systems is effective in prostates with volumes of above 60cc, and no significant differences have been found in the IPSS, residual volume and maximum flow [20,27-29].
Ruszat et al. reported on 116 patients who underwent PVP and were on antiplatelet and/or anticoagulant therapy [2,9,26], no blood transfusions were required, and 2-year results were equivalent to the control group. However, patients in the antiplatelet/anticoagulant therapy group were found to have worse intraoperative haemostatic control. The only difference was that vaporised patients who were not on anticoagulants required a shorter catheterisation time, and this finding was confirmed by other authors [2,9,26]. Other long-term studies have demonstrated the durability of GPVP in the treatment of BPH at three and five years [14,16,18].
In a 5-year study in patients with GPVP, Hai et al. [14] concluded that the improvement in Qmax and AUASS is maintained 5 years after treatment, with fewer complications than HoLEP, TURP and OP and that GPVP can be performed in high-risk patients and in prostates of all sizes. In 2009, Reich et al. reported on the one-year results of 66 patients with a surgical risk classification of ASA 3 or higher. No blood transfusions were needed, 11% were recatheterised, there was a 222% improvement in Qmax, a mean reduction in IPSS of 14 points versus baseline and a 1.5% incidence of reoperation [26,27]. In 2008, Choi et al. suggested that GPVP should be the first line treatment in patients with a high anaesthetic risk [27].
Few studies have assessed erectile function following GPVP. Bruyere et al. [29] reported a fall in IIEF-5 score 2 years after photovaporisation in previously healthy patients, and Paick et al. [30] reported an improvement in IIEF-5 and preserved erectile function as before, after photovaporisation. Kavoussi et al. also reported an improved IIEF-5 score following surgery [30]. Hamman concluded that erectile function was not affected after PVP and that IIEF-5 score remained stable [30]. Spaliviero et al. [13] did not find worsening of erectile function 12 months after PVP with HPS. In the literature there has only been one case report of ED 6 months after surgery, and the authors thought that it was not attributable to the surgery [19]. The incidence of retrograde ejaculation after PVP is between 28% and 36%, which is lower than in TURP where the figure can be as high as 75% [3, 13,29,30].
GPVP Complications are lower than in patients with TURP; dysuria is 6% - 30% in the first month, recatheterisation is 1% - 5%, mild and transient haematuria 1% - 5%, transient dysuria 7% - 30%, urine infection 0% - 6%, prostatic sclerosis 1% - 2%, retrograde ejaculation 28% - 36%, blood transfusion, erectile dysfunction and incontinence <0.5%, urethral stenosis 0% - 4%, reoperation 0% - 7% at 5 years [20,29,30].
In 2007, Sountoulides et al. [15] concluded that laser prostatectomy was starting to compete with TURP as the gold standard treatment for BPH. In a study on 67 patients, Omer et al. concluded that the high-power KTP laser represented a new challenge to the gold standard status of TURP. At present, high-power GPVP and HoLEP are the most widely-accepted techniques that have major potential for replacing TURP and OP [4].
5. Conclusion
There was a 64% improvement in IPSS at 5 years, which was almost sustained from 3 months after surgery onwards. Qmax at 5 years versus baseline showed a 250% improvement that was maintained from the post-operative period to the 5-year follow-up. The mean preoperative IIEF-5 score was 14, attributable to patients' multiple pathologies. At 5 years, the score remained unchanged from the preoperative (p < 0.01). There were fewer complications than with conventional techniques: no patients suffered urinary incontinence or erectile dysfunction or required a blood transfusion. 2.25% suffered major complications, 1.4% still had de novo urgency at 3 years, and after 5 years of follow-up 3.75% had been reoperated. Our study confirms, like other authors, that GPVP should be the technique of choice in surgical treatment for patients with LUTS and high anesthetic risk.
REFERENCES
- C. Capitán Manjon, J. M. de la Morena, E. de la Peña, et al., “Papel Actual de la Fotovaporización Prostática con Láser Greenlight HPS. Aspectos téCnicos y Revisión de la Literatura,” Actas Urológicas Españolas, Vol. 33, No. 7, 2009, pp. 771-777. doi:10.1016/S0210-4806(09)74230-5
- X. Yu, S. P. Elliott, T. J. Wilt, et al., “Practice Patterns in Benign Prostatic Hyperplasia Surgical Therapy: The Dramatic Increase in Minimally Invasive Technologies,” The Journal of Urology, Vol. 180, No. 1, 2008, pp. 241-245. doi:10.1016/j.juro.2008.03.039
- G. Alivizatos and A. Skolarikos, “Greenlight in Benign Prostatic Hyperplasia: Turning Green into Gold,” Current Opinion in Urology, Vol. 18, 2008, pp. 46-49. doi:10.1097/MOU.0b013e3282f0d63b
- P. Sountoulides, O. Kaufmann, D. Kikidakis, et al., “Vaporización Fotoselectiva de la Próstata (VFP) vs Enucleacion de la Próstata Con Laser Holmio (HoLEP): Resultados Actuales y Estrategias,” Archivos Españoles de Urología, Vol. 63, No. 2, 2010, pp. 89-101. doi:10.4321/S0004-06142010000200001
- W. J. Fu, B. F. Hong, X. X. Wang, et al., “Evaluation of Greenlight Photoselective Vaporization of the Prostate for the Treatment of High Risk Patients with Benign Prostatic Hyperplasia,” Asian Journal of Andrology, Vol. 8, 2006, pp. 367-371. doi:10.1111/j.1745-7262.2006.00134.x
- A. E. Te, T. R. Malloy, B. S. Stein, et al., “Photoselective Vaporization of the Prostate for the Treatment of Benign Prostatic Hyperplasia: 12 Months Results from the First United States Multicenter Prospective Trial,” The Journal of Urology, Vol. 172, No. 4, 2004, pp. 1404-1408. doi:10.1097/01.ju.0000139541.68542.f6
- O. F. Karatas, E. Alkan, K. Horansali, et al., “Photoselctive Vaporization of the Prostate in Men with a History of Chronic Oral Anti-Coagulation,” BJU International, Vol. 36, No. 2, 2010, pp. 190-197. doi:10.1590/S1677-55382010000200009
- E. López Alcina, J. U. Juan Escudero, M. Fabuel Deltoro, et al., “Fotovaporización Prostática (FVP) Mediante Lá- ser Verde. Ventajas Quirúrgicas en Pacientes de Riesgo,” Archivos Españoles de Urología, Vol. 61, No. 9, 2008, pp. 1029-1034. doi:10.4321/S0004-06142008000900012
- N. J. Parr, C. S. Loh and A. D. Desmond, “Transurethral Resection of the Prostate and Bladder Tumour without Withdrawal of Warfarin Therapy,” British Journal of Urology, Vol. 64, No. 6, 1989, pp. 623-625. doi:10.1111/j.1464-410X.1989.tb05322.x
- J. S. Sandhu, C. Ng, B. A. Vanderbrink, et al., “HighPower Potassium-Titanyl-Phosphate Photoselective Laser Vaporization of Prostate for Treatment for Treatment of Benign Prostatic Hyperplasia in Men with Large Prostates,” Urology, Vol. 64, No. 6, 2004, pp. 1155-1159. doi:10.1016/j.urology.2004.07.018
- B. V. Cleynenbreugel, S. J. Srirangam and H. Van Poppel, “High Performance System Greenlight Laser: Indications and Outcomes,” Current Opinion in Urology, Vol. 19, 2009, pp. 33-37. doi:10.1097/MOU.0b013e328317cab3
- H. Son, S. H. Song, J. S. Paick, “Current Laser Treatments for Benign Prostatic Hyperplasia,” Korean Journal of Urology, Vol. 51, No. 11, 2010, pp. 737-744. doi:10.4111/kju.2010.51.11.737
- M. Spaliviero, K. Strom, X. Gu, et al., “Does Green Light HPS Laser Photoselective Vaporization Prostatectomy Affect Sexual Function?” Journal of Endourology, Vol. 24, No. 12, 2010, pp. 2051-2057. doi:10.1089/end.2010.0296
- M. A. Hai, “Photoselective Vaporization of Prostate: Five Years Outcomes of Entire Clinic Patient Population,” Urology, Vol. 73, No. 4, 2009, pp. 807-810. doi:10.1016/j.urology.2008.08.502
- P. Sountoulides and P. Tsakiris, “The Evolution of KTP Laser Vaporization of the Prostate,” Yonsei Medical Journal, Vol. 49, No. 2, 2008, pp. 189-199. doi:10.3349/ymj.2008.49.2.189
- M. Spaliviero, M. Araki, D. J. Culkin, et al., “Incidence, Management, and Prevention of Perioperative Complications of Greenlight HPS Laser Photoselective Vaporization Prostatectomy: Experience in the First 70 Patients,” Journal of Endourology,, Vol. 23, No. 3, 2009, pp. 495- 502. doi:10.1089/end.2008.0299
- H. Son, Y. K. Ro, S. H. Min, et al., “Modified Vaporization-Resection for Photoselective Vaporization of the Prostate Using a Greenlight High-Performance System 120-W Laser: the Seoul Technique,” Urology, Vol. 77, No. 2, 2011, pp. 427-432. doi:10.1016/j.urology.2010.06.034
- R. Ruszat, S. Wyler, T. Forster, et al., “Safety and Effectiveness of Photoselective Vaporization of the Prostate (PVP) in Patients on Ongoing Oral Anticoagulation,” European Urology, Vol. 51, No. 4, 2007, pp. 1031-1038. doi:10.1016/j.eururo.2006.08.006
- H. Woo, O. Reich, A. Bachmann, et al., “Outcome of Greenlight HPS 120-W Laser Therapy in Specific Patients Populations: Those in Retention, on Anticoagulants and with Larges Prostates (≥80 ml),” European Urology Supplements, Vol. 7, No. 4, 2008, pp. 378-383. doi:10.1016/j.eursup.2008.01.016
- A. E. Te, T. R. Malloy, B. S. Stein, et al., “Impact of Prostate-Specific Antigen Level and Prostate Volume as Predictors of Efficacy in Photoselective Vaporization Prostatectomy: Analysis and Results of Ongoing Prospective Multicentre Study at 3 Years,” BJU International, Vol. 97, No. 6, 2006, pp. 1229. doi:10.1111/j.1464-410X.2006.06197.x
- A. E. Te, “The Next Generation in Laser Treatments and the Role of the Greenlight High-Perfomance System Laser,” Reviews in Urology, Vol. 8, Suppl. 3, 2006, pp. S24- S30.
- A. Bachmann, R. Ruszat, S. Wyler, et al., “Photoselective Vaporization of the Prostate. The Basel Experience after 108 Procedures,” European Urology, Vol. 47, No. 6, 2005, pp. 798-804. doi:10.1016/j.eururo.2005.02.003
- D. M. Bouchier-Hayes, P. Anderson, S. Van Appledorn, et al., “KTP Laser versus Transurethral Resection: Early Results of a Randomized Trial,” Journal of Endourology, Vol. 20, No. 8, 2006, pp. 580-585. doi:10.1089/end.2006.20.580
- A. Bachmann, L. Schurch, R. Ruszat, et al., “Photoselective Vaporization (PVP) versus Transurethral Resection of Prostate (TURP): A Prospective Bi-Centre Study of Perioperative Morbidity and Early Functional Outcome,” European Urology, Vol. 48, No. 6, 2005, pp. 956-972. doi:10.1016/j.eururo.2005.07.001
- R. Ruszat, S. Wyler, M. Seitz, et al., “Comparison of Potassium-Titanyl-Phosphate Laser Vaporization of the Prostate and Transurethral Resection of the Prostate: Update of a Prospective Non-Randomized Two-Centre Study,” BJU International, Vol. 102, No. 10, 2008, pp. 1432-1438.
- O. Reich, A. Bachmann, M. Siebels, et al., “High Power (80 W) Potassium-Titanyl-Phosphate Laser Vaporization of the Prostate in 66 High Risk Patients,” The Journal of Urology, Vol. 173, No. 1, 2005, pp. 158-160. doi:10.1097/01.ju.0000146631.14200.d4
- B. Choi, S. Tabatabaei, A. Bachmann, et al., “Greenlight HPS 120 W Laser for BHP: Comparative Complications and Technical Recommendations,” European Urology, Vol. 7, 2008, pp. 384-388. doi:10.1016/j.eursup.2008.01.013
- X. Yu, S. P. Elliot, T. J. Wilt, et al., “Practice Patterns in Benign Prostatic Hyperplasia Surgical Therapy: The Dramatic Increase in Minimally Invasive Technologies,” The Journal of Urology, Vol. 180, No. 1, 2008, pp. 241-245. doi:10.1016/j.juro.2008.03.039
- F. Bruyere, A. Puichaud, H. Pereira, et al., “Influence of Photoselective Vaporization of the Prostate on Sexual Function: Results of a Prospective Analysis of 149 Patients with Long-Term Follow-Up,” European Urology, Vol. 58, No. 2, 2010, pp. 2007-2011. doi:10.1016/j.eururo.2010.04.027
- M. S. Wosnitzer and M. P. Rutman, “KTP/LBO Laser Vaporization of the Prostate,” Urologic Clinics of North America, Vol. 36, No. 4, 2009, pp. 471-483. doi:10.1016/j.ucl.2009.08.004

