Case Reports in Clinical Medicine
Vol.2 No.2(2013), Article ID:31749,4 pages DOI:10.4236/crcm.2013.22035
Successful coil embolization with a basic technique for ruptured posterior tibial artery in a patient with Ehlers-Danlos syndrome type IV: A case report
![]()
1Department of Diagnostic and Interventional Neuroradiology, Yamagata City Hospital Saiseikan, Yamagata, Japan; *Corresponding Author: naght@saiseikan.jp
2Department of Surgery, Yamagata City Hospital Saiseikan, Yamagata, Japan
3Department of Neurosurgery, Yamagata City Hospital Saiseikan, Yamagata, Japan
Copyright © 2013 Satoko Nezu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received 18 March 2013; revised 20 April 2013; accepted 4 May 2013
Keywords: Ehlers-Danlos Syndrome Type IV; Peripheral Arterial Rupture; Coil Embolization
ABSTRACT
The surgical management of vascular complication with Ehlers-Danlos Syndrome type IV (EDSIV) is extremely challenging because of its tissue or organ fragility including arteries. Less traumatic maneuvers and devices have been recommended to perform the endovascular treatment for the vascular lesion of EDS-IV, although the endovascular procedure is less invasive than surgical intervention. We report a 23-yearold man with EDS-IV suffered from left posterior tibial arterial rupture. We performed internal trapping of the ruptured segment using detachable coils with a standard technique via the contralateral femoral artery puncture. The patient was discharged without any complication associated with the endovascular procedure. Embolization by a basic technique, performed with greatest care, is a safe and useful treatment option which we radiologists should try for managing EDS-IV patients.
1. INTRODUCTION
Ehlers-Danlos syndromes (EDS) are a group of inherited connective tissue disorders characterized by skin hyperextensibility, joint hypermobility, and tissue fragility. This syndrome is classified into six major types [1]. EDS type IV (EDS-IV), known as vascular type, is characterized by thin translucent skin, fragility or rupture of arteries, intestines and uterus. Patients with EDS-IV also show characteristic facial features and often suffer from extensive bruising [2]. Vascular complications in EDS-IV, such as arterial rupture, aneurysms, and dissection, are life threatening and often difficult to manage surgically because of the connective tissue fragility [2-4]. We report a 23-year-old male patient with EDS-IV associated with a posterior tibial arterial rupture successfully treated by a standard endovascular coil embolization.
2. CASE REPORT
A 23-year-old man noticed sudden pain in his left calf while walking. He came to our hospital as an out-patient. He had undergone colostomy because of sigmoid-colonic perforation 7 months ago in our hospital. At the colostomy, surgeons were alarmed by his friable intestine and mesentery. From these fragile organs and his translucent skin, he was clinically diagnosed as EDS-IV and skin biopsy revealed decrease of type III collagen production.
His left lower leg was swollen and aching, but his vital signs were normal. Contrast-enhanced computed tomography (CT) scan showed a swollen left calf and faint extravasation from left fibular artery (Figures 1(a) and (b)). 3D-CT angiograms (3D-CTA) revealed irregular dilatation of the left posterior tibial artery (Figure 1(c)). Extravasation from the fibular artery was so faint that the surgeons chose a conservative therapy without admission initially, hesitating to perform surgical intervention.
The patient, unfortunately, hit his swollen leg after 4 days and required emergency admission. Contrastedenhanced CT scan on admission revealed a vivid extravasation of contrast media from dilated left posterior tibial artery (Figure 2). To avoid compartment syndrome due to continuous arterial bleeding, immediate hemostasis was considered. The surgeons, however, hesitated to
 (a)
(a)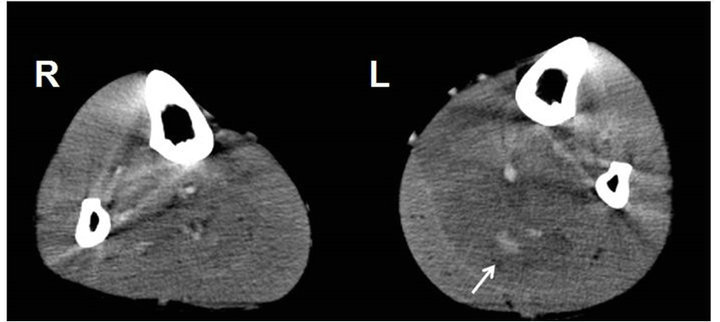 (b)
(b) (c)
(c)
Figure 1. (a) Arterial phase of contrast-enhanced computed tomography (CT) scan shows swelling of the left calf. The caliber of left posterior tibial artery is enlarged, comparing with the opposite side (arrows); (b) Venous phase of contrast-enhanced CT scan indicates a faint extravasation (arrow) from left fibular artery; (c) 3D-CT angiogram shows irregular dilatation of the left posterior tibial artery.
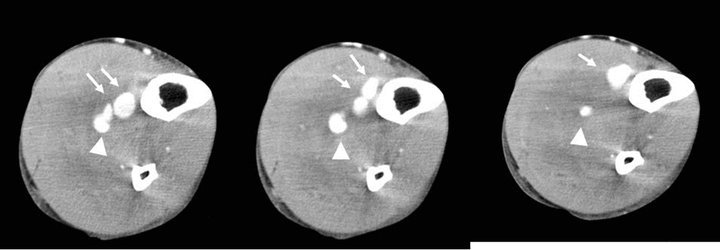
Figure 2. Contrast-enhanced CT scans on admission reveal vivid extravasation (arrows) from dilated left posterior tibial artery (arrowheads).
perform surgical intervention because they had experienced much difficulty during the patient’s prior surgery (colostomy). Therefore, emergent endovascular therapy was planned.
We punctured the right femoral artery with Seldinger’s method using 4Fr-11 cm sheath introducer (Supersheath, Medikit, Tokyo, Japan). We then inserted the 4Fr diagnostic catheter (Shepherd-hook type, Create Medic, Yokohama, Japan) into the left superficial femoral artery via the aortic bifurcation using 0.035-inch guide wire (Medikit, Tokyo, Japan).
Left superficial femoral arteriogram showed a fusiform aneurysm of the posterior tibial artery with a segmental wall irregularity distal to the aneurysm (Figure 3(a)). Late arterial phase of the arteriogram also revealed an extravasation from the aneurysm (Figure 3(b)). Because we could easily pass the catheter through the aneurysm and irregular segment using microcatheter system (Renegade-18, Boston Scientific Japan, Tokyo, Japan/0.016-inch Radifocus GT wire, Terumo, Tokyo, Japan), we planned an internal trapping of the abnormal segment by the distal-to-proximal fashion. We initially deployed three detachable coils (Orbit Galaxy 5.0 mm - 15 cm, 4.0 mm - 12 cm, 4.0 mm - 12 cm, Johnson and Johnson, Tokyo, Japan) at the distal end of the irregular segment. Then we added a detachable coil (Matrix2 8.0 mm - 30 cm, Boston Scientific Japan, Tokyo, Japan) within the aneurysm followed by three coils (Matrix2 5.0 mm - 15 cm, Orbit Galaxy 3.5 mm - 7.5 cm, 3.5 mm - 7.5 cm) deployed at just proximal to the aneurysm (Figure 4).
After the embolization, the lesion was completely divided from the arterial supply of the left lower leg (Figure 5). Distal left posterior tibial artery of normal appearance was well-supplied via muscular branches. In
 (a) (b)
(a) (b)
Figure 3. (a) Arterial phase of the left superficial femoral arteriogram (digital subtraction angiography) shows an irregular fusiform aneurysm (arrow) of the posterior tibial artery. Segmental wall irregularity is also shown distal to the aneurysm (arrowheads); (b) An extravasation (arrow) from the aneurysm was shown on the late arterial phase.

Figure 4. Left: Posterior tibial arteriogram during the endovascular procedure shows three detachable coils deployed at the distal end of irregular segment. Microcatheter tip is positioned within the proximal fusiform aneurysm. Right: Digital radiogram reveals a complete internal trapping by detachable coils. Rough coiling indicates the fusiform aneurysm (arrow).
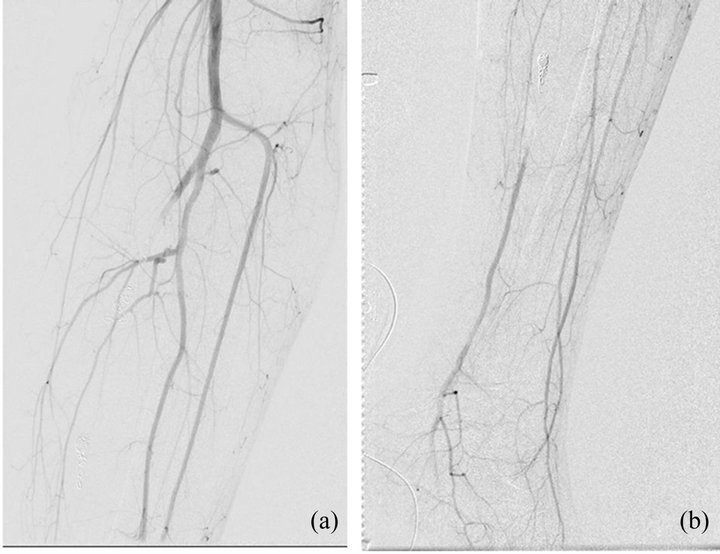
Figure 5. (a), (b) Left superficial femoral arteriograms show a complete disappearance of the abnormal segment including fusiform aneurysm. Distal posterior tibial artery is well-visualized by collaterals.
this patient, decompressing fasciotomy was unnecessary during the clinical course. Sixteen days after the embolization, the patient was discharged without any trouble at the puncture site or access route, or in the left lower leg.
3. DISCUSSION
Ehlers-Danlos Syndrome type IV is a very rare disorder with marked fragility of arteries and organs. It is an autosomal dominant inherited disorder resulting from mutations in the gene of type III collagen (COL3A1) [5, 6]. About 64% - 77% of the patients develop vascular complications, such as arterial rupture threatening their life [3,5]. It has been reported that the initial symptom appears by the age of 20 years in almost patients, and their median survival age is 48 years [5].
We had achieved successful coil embolization for ruptured posterior tibial artery (PTA) in the present case of EDS-IV. To the best of our knowledge, ruptured PTA or pseudoaneurysm of PTA due to EDS-IV has been reported in only 3 cases [7-9]. All cases were treated by endovascular procedure. In these reports, antegrade approach via the ipsilateral or contralateral femoral puncture was performed in two cases, and a retrograde approach using distal PTA puncture was performed in another case.
It has been recognized that the most important complication in endovascular procedures for EDS-IV is a puncture-site trouble, such as femoral arterial rupture, pseudoaneurysm formation, or large access-site hematoma [3,4]. To avoid these procedure-related complications, Brooke et al. recommended an open repair and sheath-insertion with “U” stitch [4]. Smaller access devices and less traumatic catheter and wires are also recommended [4,7]. Hagspiel et al. had performed a retrograde catheter-approach for the ruptured PTA from a distal PTA puncture [7].
In the present case, we choose an antegrade approach via the contralateral femoral puncture with usual technique and devices. Accustomed femoral puncture seemed to be safer than the unusual antegrade puncture of ipsilateral femoral artery. We also thought that our standard 4Fr sheath-introducer and diagnostic catheter system was less traumatic. Some people may say that the ipsilateral femoral approach should be preferable rather than the contralateral way, because of the risk of vascular trouble during catheterization through a long approach crossing over the aortic bifurcation. There is, however, no report mentioning the arterial dissection or rupture of approach route for endovascular treatment of EDS-IV. In our case, fortunately, contrast-enhanced CT scan had revealed no aorto-iliac lesions. Therefore, we intentionally performed contralateral femoral puncture with great care. Of course, we also used the greatest care while handling the catheters and guidewires.
Internal coil trapping, as in the present case, should be a basic strategy to manage a ruptured artery in EDS-IV patients [7-11]. Transcatheter injection of n-butyl cyanoacrylate (NBCA)-Lipiodol mixture may be an optional technique when the microcatheter could not access the distal normal segment crossing through the ruptured site [9].
4. CONCLUSION
Successful embolization for ruptured PTA of the EDS-IV patient was achieved by a standard internal coil trapping technique with paying great care in handling the endovascular devices. Although EDS-IV patients are known to have fragile arteries, endovascular treatment can be a suitable alternative management, which we radiologists should try without hesitation, for peripheral vascular lesions in EDS-IV patients.
REFERENCES
- Beighton, P., De Paepe, A., Steinmann, B., Tsipouras, P. and Wenstrup, R.J. (1997) Ehlers-Danlos syndromes: Revised nosology, villefranche. American Journal of Medical Genetics, 77, 31-37. doi:10.1002/(SICI)1096-8628(19980428)77:1<31::AID-AJMG8>3.0.CO;2-O
- Lum, Y.W., Brooke, B.S. and Black III, J.H. (2011) Contemporary management of vascular Ehlers-Danlos syndrome. Current Opinion in Cardiology, 26, 494-501. doi:10.1097/HCO.0b013e32834ad55a
- Oderich, G.S., Panneton, J.M., Bower, T.C., Lindor, N.M., Cherry, K.J., et al. (2005) The spectrum, management and clinical outcome of Ehlers-Danlos syndrome type IV: A 30-year experience. Journal of Vascular Surgery, 42, 98- 106. doi:10.1016/j.jvs.2005.03.053
- Brooke, B.S., Arnaoutakis, G., McDonnell, N.B. and Black III, J.H. (2010) Contemporary management of vascular complications associated with Ehlers-Danlos syndrome. Journal of Vascular Surgery, 51, 131-139. doi:10.1016/j.jvs.2009.08.019
- Pepin, M., Schwarze, U., Superti-Furga, A. and Byers, P.H. (2000) Clinical and genetic features of Ehlers-Danlos syndrome type IV, the vascular type. New England Journal of Medicine, 342, 673-668. doi:10.1056/NEJM200003093421001
- Superti-Furga, A., Steinmann, B. and Byers, P.H. (1989) Type III collagen deficiency. Lancet, 22, 903-904. doi:10.1016/S0140-6736(89)92899-7
- Hagspiel, K.D., Bonatti, H., Sabri, S., Arslan, B. and Harthun, N.L. (2011) Metachronous bilateral posterior tibial artery aneurysms in Ehlers-Danlos syndrome type IV. CardioVascular and Interventional Radiology, 34, 413- 418. doi:10.1007/s00270-010-9929-4
- Matsushima, K. and Takara, H. (2009) Endovascular treatment for a spontaneous rupture of the posterior tibial artery in a patient with Ehlers-Danlos syndrome type IV: Report of a case. Surgery Today, 39, 523-526. doi:10.1007/s00595-008-3881-9
- Uchiyama, D., Koganemaru, M., Abe, T., Akashi, H., Hayabuchi, N., et al. (2006) Successful transcatheter arterial embolization for spontaneous rupture of the posterior tibial artery in a patient with Ehlers-Danlos syndrome type IV. Journal of Vascular and Interventional Radiology, 17, 1716-1717. doi:10.1097/01.RVI.0000236585.57552.FF
- Iida, Y., Obitsu, Y., Komai, H. and Shigematsu, H. (2009) Successful coil embolization for rupture of the subclavian artery associated with Ehlers-Danlos syndrome type IV. Journal of Vascular Surgery, 50, 1191-1195. doi:10.1016/j.jvs.2009.05.064
- Sugawara, Y., Ban, K., Imai, K., Okada, K., Watari, M., et al. (2004) Successful coil embolization for spontaneous arterial rupture in association with Ehlers-Danlos syndrome type IV: Report of a case. Surgery Today, 34, 94- 96. doi:10.1007/s00595-003-2634-z

