International Journal of Otolaryngology and Head & Neck Surgery
Vol. 1 No. 3 (2012) , Article ID: 24814 , 4 pages DOI:10.4236/ijohns.2012.13021
Tympanometry, a Prognostic Indicator of Myringoplasty with Assessment of Eustachian Tube Function
Department of ENT, Govt Grant Medical College and JJ Group of Hospitals, Mumbai, India
Email: ssj19july@yahoo.co.in
Received October 1, 2012; revised October 31, 2012; accepted November 8, 2012
Keywords: Tympanometry; Myringoplasty; Eustachian Tube Function
ABSTRACT
Objective: To determine Eustachian tube function in tubotympanic type of chronic ear disease and to correlate Eustachian tube function with pathological change in middle ear mucosa. Materials and Methods: A prospective study of the cases of tubotympanic type of chronic suppurative otitis media was undertaken. Patients were subjected to clinical examination followed by audiometry tests and impedence audiometry to determine eustachian tube functions. Patients were then subjected to myringoplasty and eustachian tube function were then reassessed post operatively. Results: In our study, out of 30 cases who underwent myringoplasty, 21 cases had successful surgical outcome and 9 cases were failed. Out of 24 cases of good Eustachian tube function, 21 cases had successful surgical outcome intends of taking up graft, absence of otorrhea and improvement in hearing. In remaining 3 cases, there was recurrence of otorrhea with central perforation. All the 6 cases with poor Eustachian tube function had surgical failure. Conclusion: The prognosis of the middle ear reconstructive surgery has direct correlation with Eustachian tube functions and Eustachian tube function tests should be a routine investigation in all the cases planned for surgical reconstruction of the middle ear.
1. Introduction
Reconstructive ear surgery is one of the most common surgeries taken up by the otologist. The success of the surgery is indicated by improvement in hearing & non persistence of the symptoms. One of the important factors on which success of the surgery depends, is proper functioning of Eustachian tube.
The Eustachian tube, also auditory tube or pharyngotympanic tube, is a tube that links the nasopharynx to the middle ear. It is a part of the middle ear. In adult humans the Eustachian tube is approximately 35 mm (1.4 in) long. The Eustachian tube extends from the anterior wall of the middle ear to the lateral wall of the nasopharynx. It aerates the middle ear system and clears mucus from the middle ear into the nasopharynx. Opening and closing functions of the eustachian tube are physiologically and pathologically important. Normal opening of the eustachian tube equalizes atmospheric pressure in the middle ear; closing of the eustachian tube protects the middle ear from unwanted pressure fluctuations and loud sounds. Mucociliary clearance drains mucus away from the middle ear into the nasopharynx, thus preventing infection from ascending to the middle ear.
Adequate tubal function is a prerequisite for the success of the middle ear reconstructive surgeries hence assessment of Eustachian tube function is of paramount importance not only before undertaking any surgery for suppurative otitis media but also in establishing its etiological basis.
However, the assessment of Eustachian tube function has been implicated in tympanoplasty failure both primarily via middle ear pressure dynamic & secondarily via recurrent otitis media. Since, tubal function has been shown to improve with the age, the goal has been to devise a test, which could describe Eustachian tube function adequately & thereby predict success or failure of middle ear surgery.
2. Aims of the Study
1) Eustachian tube function in tubotympanic type of chronic ear disease.
2) To correlate Eustachian tube function with pathological change in middle ear mucosa.
3) An attempt was also made to ascertain whether Eustachian tube function had any bearing upon the outcome of myringoplasty.
3. Material and Methods
A prospective study of the cases of tubotympanic type of chronic suppurative otitis media with central perforation attending the ENT outpatient department and who are undergoing myringoplasty at our hospital was undertaken from 1st November 2010 to 30th November 2011.
A thorough history was taken for otorrhea and hearing loss. The discharging ear is thoroughly cleaned, the central perforation and attico antral disease excluded, a thorough clinical ENT examination was done and evidence of any ENT conditions were ruled out. Tuning fork tests were done with 256 Hz, 512 Hz, and 1024 Hz tuning forks. Tuning fork tests includes Rinne’s, weber’s and Absolute bone conduction tests.
The ear was then subjected to microscopic evaluation to assess the condition of the middle ear mucosa and based on these findings middle ear mucosa was classified into, dry, moist and boggy status. Subsequently all these patients were subjected to audiological investigation. A pure tone audiometry was done with ELKON-EDA-3N3 multi pure tone audiometer and the hearing status was assessed, patients having poor cochlear reserves was excluded from the study.
This was followed by Eustachian tube function evaluation by the AMPLAID 724 impedance audiometer. The opening pressure and the residual pressure of the test ears were measured. Accordingly they were grouped into subjects having good Eustachian tube function and poor Eustachian tube function. Patient having residual pressure of more than 50 dapa were grouped as poor Eustachian tube function and those having less than 50 dapa were grouped as good Eustachian tube function.
A myringoplasty was performed in all the patients. The operation was done under local anaesthesia and a postaural and a per meatal incision was taken accordingly. The temporalis fascia was chosen as graft material. The patients were then called after 3 week (i.e. postoperative 6 week) and 9 week (i.e. postoperative 12 week) Eustachian tube function by impedance audiometry was again repeated in all the patients. In patients with intact tympanic membrane a tympanometric assessment was made by measuring the middle ear pressure first and subsequently twice again after asking the patients to swallow in an attempt to make the Eustachian tube patent and functioning.
The patient in whom the graft failed to take up and the perforation persisted was subjected to Eustachian tube function for perforated tympanic membrane, the opening and the residual pressure of that was noted.
The same procedure was done and same data was collected after 12 weeks. The correlation between the Eustachian tube function and surgical outcome was then studied and evaluated.
4. Results and Observations
4.1. Eustachian Tube Functions by Impedance Audiometry
Impedance audiometry for Eustachian tube functions were done in all the cases.
Out of 30 cases, 24 cases (80%) had good Eustachian tube functions in which 9 cases (37.5%) were having bilateral chronic suppurative otitis media and remaining 15 cases (62.5%) had unilateral chronic otitis media (Table 1).
Out of 30 cases 6 cases (20%) had poor Eustachian tube functions in which 5 cases (83.33%) had bilateral chronic suppurative otitis media and 1 case (16.666%) had unilateral chronic suppurative otitis media (Table 1).
4.2. State of Middle Ear Mucosa
Out of 30 cases 20 cases (66.66%) had dry middle ear mucosa, 4 cases (13.33%) had boggy middle ear mucosa and 6 cases (20%) had moist middle ear mucosa.
Out of 24 cases of good Eustachian tube function 20 cases (87.5%) had dry middle ear mucosa, 2 cases (8.33%) had boggy middle ear mucosa and 2 cases (8.33%) had moist middle ear mucosa (Table 2).
Out of 6 cases with poor Eustachian functions, 2 cases (33.33%) had boggy middle mucosa and 4 cases (66.66%) had moist middle ear mucosa (Table 2).
4.3. Results of Eustachian Tube Function
In our study, range of opening pressure of all the 30 cases was 258 dapa to 450 dapa. The mean opening pressure was 345.966 dapa. The range of residual pressure of all the 30 cases was 2 apa to 165 dapa, the mean residual pressure was 39.26 dapa.
In all 24 cases having good Eustachian tube functions the range of opening pressure was 258 dapa to 373 dapa, the mean pressure was 328.5 dapa. The range of residual pressure was 2 dapa to 45 dapa. The mean residual pressure was 23.458 dapa.
In all 6 cases having poor Eustachian tube function, the range of opening pressure was 371 dapa to 450 dapa. The mean pressure was 415.833 dapa, range of residual pressure was 60 dapa to 165 dapa and the mean pressure was 102.5 dapa.
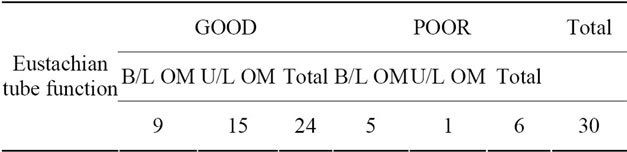
Table 1. Correlation between eustachian tube function and otitis media (OM—otitis media).
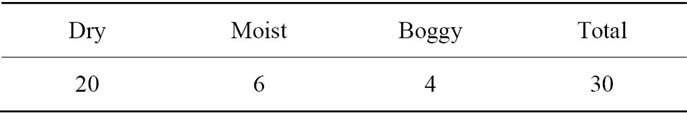
Table 2. Correlation between middle ear mucosa and eustachian tube function.
4.4. The Outcome of Myringoplasty
Out of 30 cases who underwent myringoplasty, 21 cases (70%) had successful surgical outcome and 9 cases (30%) were failed. Out of 24 cases of good Eustachian tube function, 21 cases (87.5%) had successful surgical outcome intends of taking up graft, absence of otorrhea and improvement in hearing (Figure 1). In remaining 3 cases (12.5%), there was recurrence of otorrhea with central perforation. All these 3 cases were having bilateral chronic suppurative otitis media.
All the 6 cases with poor Eustachian tube function had surgical failure, out of which, 5 cases (83.33%) were having bilateral chronic suppurative otitis media.
5. Discussion
A prevailing interest in pathophysiology of the Eustachian tube has been stimulated by the persistent incidence of middle ear effusion and chronic otitis media. The ongoing sophistication in current middle ear reconstructive surgery has added more dimensions to the study of the Eustachian tube and its effects in the course of reconstructive middle ear surgery.
The tubal dysfunction is one of the most important factors responsible for the failure of reconstructive middle ear surgery—Zollner, 1963 [1], wullstein, 1963 [2], Farrior, 1965 [3], Schuknecht, [4] and Kerr, 1967 [4]. Even recently Toss [5] and Biswas [6] 1999 have emphasized the importance of Eustachian tube function in the middle ear surgery. The Eustachian tube function has been implicated in tympanoplasty failure both primarily via middle ear pressure dynamics and secondarily via recurrent otitis media Scott et al. [7].
Adequate functioning of the Eustachian tube is also considered as one of the pre requisite of re-establishing a closed aerated tympanic cavity in tympanoplasty—Holmquist [8].
Compere, 1958 [9] and Roger, 1962 [10] assessed tubal function by observing the middle ear clearance of radio opaque fluid in to nasopharynx and Proud in 1963 [11] using fluroscent solution. Most surgeons now evaluate tubal function clinically by observing the valsalva response—M. M. Hassam et al. [12].
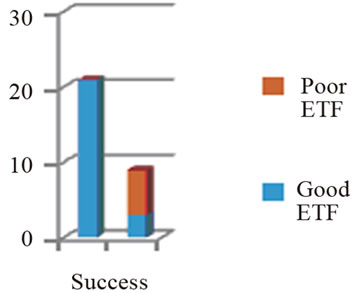
Figure 1. Correlation between surgical outcome and Eustachian tube function (ETF—eustachian tube function).
The 3 functions of Eustachian tube warrants separate testing procedure for individual functions. Eustachian tube function can also thus be evaluated by radiographic investigation like CTscan, tympanometry, sonotubometry-Virtanen et al. [13]. For maintaining normal function of the middle ear the physiological functioning and not anatomical patency of the Eustachian tube is required. A modern impedance audiometer offers us the facility of ascertaining the physiological function of the Eustachian tube not only tympanic membrane is intact but also in presence of perforation—A. Biswas.
In our study, we have used a modern impedance audiometry. Its advantages are that it can be used in perforated membrane, quick & non-invasive, patients compliance is not required, accurate and inexpensive. Comparing the data by Munjal et al. It is evident that the lower the opening pressure, higher the success rate of surgery. In our study cases having good Eustachian tube function, the mean opening pressure was 328.5 dapa and cases having poor Eustachian tube function the mean opening pressure was 415.8 dapa.
Good Eustachian tube function always carries better prognosis in surgical outcome of myringoplasty.
6. Conclusions
Impedance audiometer offers the best means of assessing Eustachian tube functions.
The Eustachian tube function can be measured in both intact as well as perforated membrane.
The prognosis of the middle ear reconstructive surgery has direct correlation with Eustachian tube functions. Good Eustachian tube functions are definite prerequisite for obtaining the good prognostic value and vice versa.
Bilateral disease does not carry a good prognosis in the operating ear in spite of the ear having good Eustachian tube functions.
The status of the middle ear mucosa has direct correlation with the outcome of the surgery.
A dry perforation carries good surgical prognosis as well as good Eustachian tube functions.
We feel that Eustachian tube function tests should be a routine investigation in all the cases planned for surgical reconstruction of the middle ear.
REFERENCES
- F. Zollner, “Therapy of the Eustachian Tube,” Archives of Otolaryngology, Vol. 78, 1963, p. 394.
- H. K. Wullstein, “A Simple Apparatus for the Assessment of Eustachian Tube Patency before Myringoplasty,” Archives of Otolaryngology, Vol. 78, 1963, p. 371.
- J. B. Farrior, “Total Tympanoplasty Type V: Eustachian Tube Patency in Tympanoplasty,” Archives of Otolaryngology, Vol. 81, No. 4, 1965, pp. 398-409. doi:10.1001/archotol.1965.00750050409015
- H. F. Schukencht and A. G. Kerr, “Pathology of the Eustachian Tube,” Archives of Otolaryngology, Vol. 86, No. 5, 1967, pp. 497-502. doi:10.1001/archotol.1967.00760050499007
- M. Tos, “Importance of the Eustachian Tube Function in Middle Ear Surgery,” Ear, Nose and Throat Journal, Vol. 77, No. 9, 1998, pp. 744-747.
- A. Biswas, “Eustachian Tube Function Test; a New Dimension in the Management of Chronic Suppurative Otitis Media,” Indian Journal of Otology and Head Neck Surgery, Vol. 51, No. 2, 1999, pp. 14-22.
- S. C. Manning, C. D. Bluestone, et al., “A Prognostic Value of Eustachian Tube Functions in Paediatric Tympanoplasty,” Laryngoscope, Vol. 97, No. 9, 1997, pp. 1012-1016.
- J. Holmquist, “Evaluation of Eustachian Tube Function,” Journal of Otology and Laryngology, Vol. 94, 1980, pp. 15-23.
- W. E. Compere Jr., “Tympanic Cavity Clearance Studies,” Transaction American Academy of Ophthalmology and Otolaryngology, Vol. 64, 1958, p. 444.
- R. L. Rogers, “The Evaluation of Eustachian Tubal Function by Fluorescent Dye Studies,” Laryngoscope, Vol. 72, No. 4, 1962, pp. 456-480. doi:10.1288/00005537-196204000-00003
- G. O. Proud, “Assessment of Eustachian Tube Functions in Patients with Ear Drum Perforation,” Annals of Otology, Rhinology and Laryngology, Vol. 72, 1963, p. 563.
- M. M. Hassam, “A Simple Assessment of Eustachian Tube Patency before Myringoplasty,” Journal of Laryngology and Otology, Vol. 93, No. 1, 1979, pp. 39-42. doi:10.1017/S0022215100086692
- H. Virtanen, “The Prognostic Value of Eustachian Tube Function Measurements in Tympanoplastic Surgery,” Acta Otolarynogologica, Vol. 90, 1980, pp. 317-323.
- M. Manish, et al., “Forced Response Test and Myringoplasty Results,” Indian Journal of Otology and Head and Neck Surgery, Vol. 51, No. 2, 1999, pp. 66-70.

