International Journal of Clinical Medicine
Vol. 3 No. 7 (2012) , Article ID: 26056 , 14 pages DOI:10.4236/ijcm.2012.37111
Team Effectiveness in Patient Health Management: An Overview of Reviews
![]()
1Faculty of Medicine, McGill University, Montreal, Canada; 2Lausanne University Hospital, Lausanne, Switzerland; 3CareNet Corporation, Montreal, Canada.
Email: amede.gogovor@mcgill.ca
Received September 17th, 2012; revised October 20th, 2012; accepted November 18th, 2012
Keywords: Team Care Effectiveness; Chronic Disease Management; Chronic Care Model; Overview of Reviews
ABSTRACT
Background: The desire to improve the quality of health care for an aging population with multiple chronic diseases is fostering a rapid growth in inter-professional team care, supported by health professionals, governments, businesses and public institutions. However, the weight of evidence measuring the impact of team care on patient and health system outcomes has not, heretofore, been clear. To address this deficiency, we evaluated published evidence for the clinical effectiveness of team care within a chronic disease management context in a systematic overview. Methods: A search strategy was built for Medline using medical subject headings and other relevant keywords. After testing for performance, the search strategy was adapted to other databases (Cinhal, Cochrane, Embase, PsychInfo) using their specific descriptors. The searches were limited to reviews published between 1996 and 2011, in English and French languages. The results were analyzed by the number of studies favouring team intervention, based on the direction of effect and statistical significance for all reported outcomes. Results: Sixteen systematic and 7 narrative reviews were included. Diseases most frequently targeted were depression, followed by heart failure, diabetes and mental disorders. Effectiveness outcome measures most commonly used were clinical endpoints, resource utilization (e.g., emergency room visits, hospital admissions), costs, quality of life and medication adherence. Briefly, while improved clinical and resource utilization endpoints were commonly reported as positive outcomes, mixed directional results were often found among costs, medication adherence, mortality and patient satisfaction outcomes. Conclusions: We conclude that, although suggestive of some specific benefits, the overall weight of evidence for team care efficacy remains equivocal. Further studies that examine the causal interactions between multidisciplinary team care and clinical and economic outcomes of disease management are needed to more accurately assess its net program efficacy and population effectiveness.
1. Introduction
To address the growing burden of managing chronic diseases in aging populations, with increasing demand for services over time and across various care settings, innovative models of care are needed. Integrated disease care delivery represents a creative response to the challenges of chronic illness. It applies multidisciplinary care and use of available community-based social networks and interventional resources to provide evidence-based care for entire populations [1,2].
A primary component of such disease management models is the use of multidisciplinary teams in the delivery of care, with the hypothesis that teams will enhance integration of care and improve provider, patient and managerial satisfaction, as well as improving administrative and clinical processes and patient outcomes [3-5].
Thus, the multidisciplinary team approach has been widely promoted as a means to provide effective and efficient care by integrating the skills of different health care professionals to contribute to a common purpose [6-8].
Benefits of team care and teamwork have been documented in several reports [4,9-13]. Principal perceived benefits for team members include enhanced job satisfaction, sense of being valued, respected and trusted, learning from others’ expertise, sharing of workload, and enhanced sense of well-being [4,9-11,13]. These feelgood perceptions among team members, sometimes referred to as the “romance of teams” phenomenon, probably contribute, in some degree, to the common belief that teams are a very effective health care work structure [3] and that the delivery of care by a coordinated team is a good thing [6,14-16].
However, in the context of chronic disease management, there have been, as yet, only limited measurements of the efficacy of team care on patient, or health system, outcomes [9,17].
The goal of this overview was to systematically examine all available evidence in an attempt to more reliably answer the question: “Does organised team care, versus individual, or non-organised or non-integrated care, achieve improved outcomes, or care processes, among patients with chronic illness in a disease management setting?”
2. Methods
2.1. Definitions
Studying the effectiveness of team care within a chronic disease management context requires definitions. There is a broad range of definitions for chronic disease management in the literature [18,19-24]. For this overview, an intervention conducted within a chronic disease management context was defined as an intervention that targeted a specific chronic disease that involved a care team in outpatient/primary care settings. Our working definition of teamwork was based on WHO’s definition: “Coordinated action carried out by two or more individuals jointly, concurrently or sequentially. It implies common agreed goals, clear awareness of, and respect for, others’ roles and functions” [25].
According to the Cochrane Collaboration’s definition [26], a systematic review was classified as state of the art if the five following criteria were met: clearly stated objectives, predefined eligibility criteria for studies, explicit and reproducible methodology, assessment of risk of bias, systematic presentation and synthesis. Based on the criteria of Cook et al., we considered a review to be narrative if there were no explicit methods for searching literature or for reporting study results. Such reviews have a broader perspective on a given topic, sources and selection of papers usually not specified, no appraisal of studies selected, synthesis often qualitative [27].
2.2. Data Sources
In collaboration with a librarian a search strategy was built for MEDLINE using medical subject headings and other relevant keywords. After testing for its performance, the search strategy was adapted to other databases using their specific requirements. Also, reference lists from all articles in our bibliography were searched for additional citations (Table 1). Searches were limited to reviews published between 1996 and 2011, and to English and French languages.
2.3. Study Selection
A first selection was based on titles and abstracts, was performed by two authors (AG, BB) in duplicate; irrelevant articles (i.e., obviously not a review, absence of chronic disease management context, not addressing the effectiveness of team care) were discarded at this stage. Remaining article abstracts were reviewed by two authors (AG, BB) and retained if all of the following inclusion criteria were met: 1) systematic or narrative review; 2) assessment of the effectiveness of team care, provided by at least two health professionals of different speciality and corresponding to different levels of integration (collaborative, coordinated, shared care, multidisciplinary, interdisciplinary, integrated) [28,29]; 3) chronic disease management context (full disease management context if combination of chronic disease, team, and outpatient or primary care or ambulatory setting); 4) where the impact on either a process or an outcome was measured and reported. All reported outcomes were extracted. Articles that characterized the role of individual team members only were excluded. Full papers were retrieved if one or both authors considered the abstract relevant against the four inclusion criteria. The investigators independently
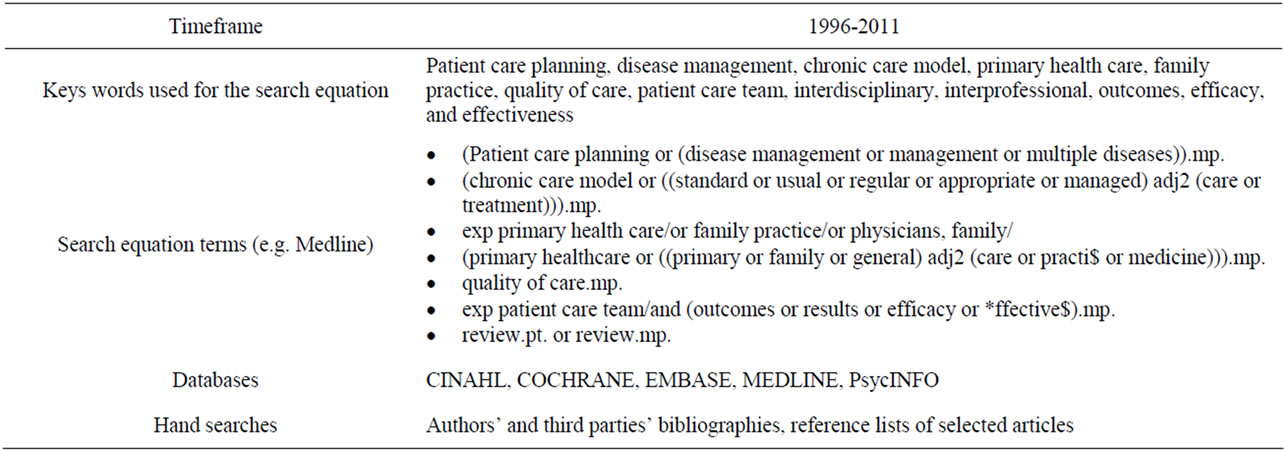
Table 1. Search strategy.
assessed full articles and discrepancies were resolved by consensual assessment.
2.4. Data Abstraction
A data abstraction form was developed and tested on several papers to ensure that it was consistent with the study objectives. The elements of the abstraction form included the type of review (systematic, narrative); the definition or model of team care and the list of healthcare professionals involved as described by the authors; the context of chronic disease management; the type of patients covered in the review; the chronic diseases targeted; the type of process and outcomes measures, the determinants of effectiveness of team care (where applicable), the conclusions of the authors of the reviews, and the category of effectiveness based on the conclusions of the authors of the reviews as follow: teamwork effective, teamwork possibly effective, teamwork possibly not effective, teamwork not effective, inconclusive. Data abstraction was performed on all eligible papers by two authors (AG, IPB). Any discrepancies were resolved by consensual assessment, and ultimately by discussion with another member of the research team.
2.5. Data Synthesis
2.5.1. Systematic Reviews
We analyzed the results by reporting for each review the number of studies favouring the intervention based on the direction of effect and statistical significance for all reported outcomes. The quality of the systematic reviews was assessed by two elements: the 5 criteria of the Cochrane Handbook of systematic reviews [26] and the AMSTAR, a measurement tool to assess systematic reviews. AMSTAR is an 11-items tool and the total score was computed as the sum of all items answered “yes”. The tool was found to have a good agreement, reliability and validity [30-32]. Data were then reported by level of quality: low (0 to 3, medium (4 to 7), and high (8 to 11) (Table 2).
2.5.2. Narrative Reviews
We conducted a separate synthesis of the findings from narrative reviews for they often lack explicit methods for searching literature or reporting results. In addition, there
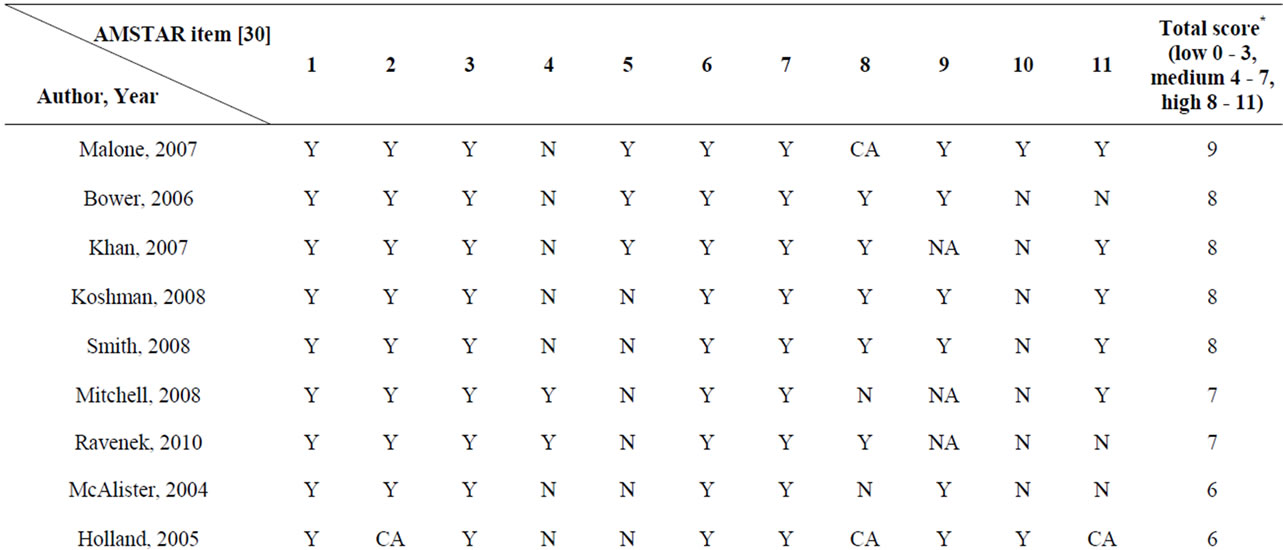
Table 2. AMSTAR assessment for included systematic reviews.
are no methods available as to how to assess the quality of narrative reviews.
3. Results
3.1. Characteristics of Included Review Papers
Sixteen systematic [33-48] and 7 narrative reviews were included in the overview [6,49-54] (see flow diagram in Figure 1). While eight systematic reviews included only randomized controlled trials, six included both randomized and non-randomized trials. Also out of the 16 systematic reviews, 8 included meta-analyses.
Diseases most frequently targeted were depression (6 reviews out of 23) followed by heart failure (4 reviews), diabetes (2 reviews) and mental disorders (2 reviews). Details about the included systematic and narrative reviews are provided in Table 3.
Systematic reviews with a meta-analysis were of better quality than systematic reviews without a meta-analysis, on the AMSTAR criteria (Table 2). The mean score for systematic reviews with meta-analyses was 7 (range 5 to 9, out of a maximum of 11) for a total of 173 primary articles (mean = 21.6) and 5.5 for non-meta-analysis systematic reviews (range 3 to 8) for a total of 135 primary articles (mean = 22.5). As expected, the quality of the systematic reviews that we classified as state of the art was very high (AMSTAR mean score = 7.2) compared to non-state of the art reviews (mean score = 4.3).
3.2. Evidence of Effectiveness
3.2.1. Systematic Reviews
Of the 16 systematic reviews reported in this study, 8 were meta-analyses. Effectiveness outcomes most commonly assessed were clinical endpoints, resource utilization (emergency room visit, hospital admission), costs, quality of life, medication adherence. While clinical and resource utilization were the most common positive outcomes, mixed results were more often found with costs, medication adherence, mortality, patient satisfaction. The overarching results are percent of the studies favouring the intervention (PSFI) and, pooled effect estimates (RR, OR, SMD) for reviews with meta-analysis. Individual results are summarized by level of quality and are reported in Table 4.
3.2.2. High Quality Reviews
In the review of Malone et al. (2007), reporting on mental illnesses, the percent of the studies favouring the intervention (PSFI) was 65% (11/17). The PSFI was 85% (53/62) for the review of Bower et al. (2006); for the measured outcomes depressive symptoms (OR = 0.24 CI 0.17 - 0.32) and antidepressants use (OR = 1.92 CI 1.54 - 2.39). The Khan et al. (2007) review on multiple sclerosis showed that 55% (12/22) of the studies favoured the intervention. In the review of Koshman et al. (2008), only 29% (5/17) of the studies that reported outcomes on collaborative care with heart failure team favoured the
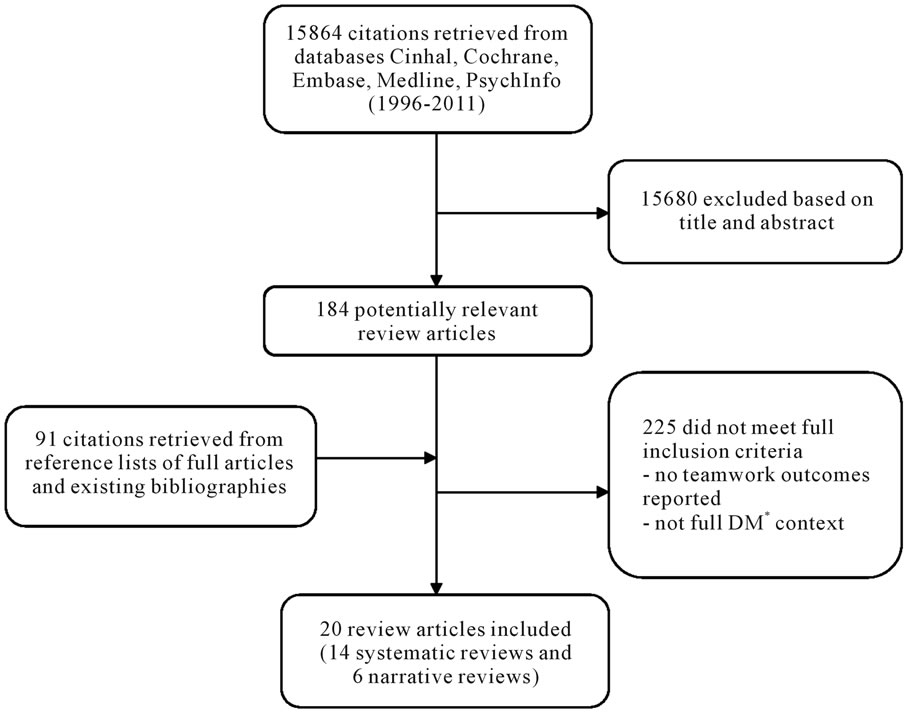
Figure 1. Flow chart of study selection. *DM = disease management (chronic disease + team + outpatient/primary care/ambulatory).
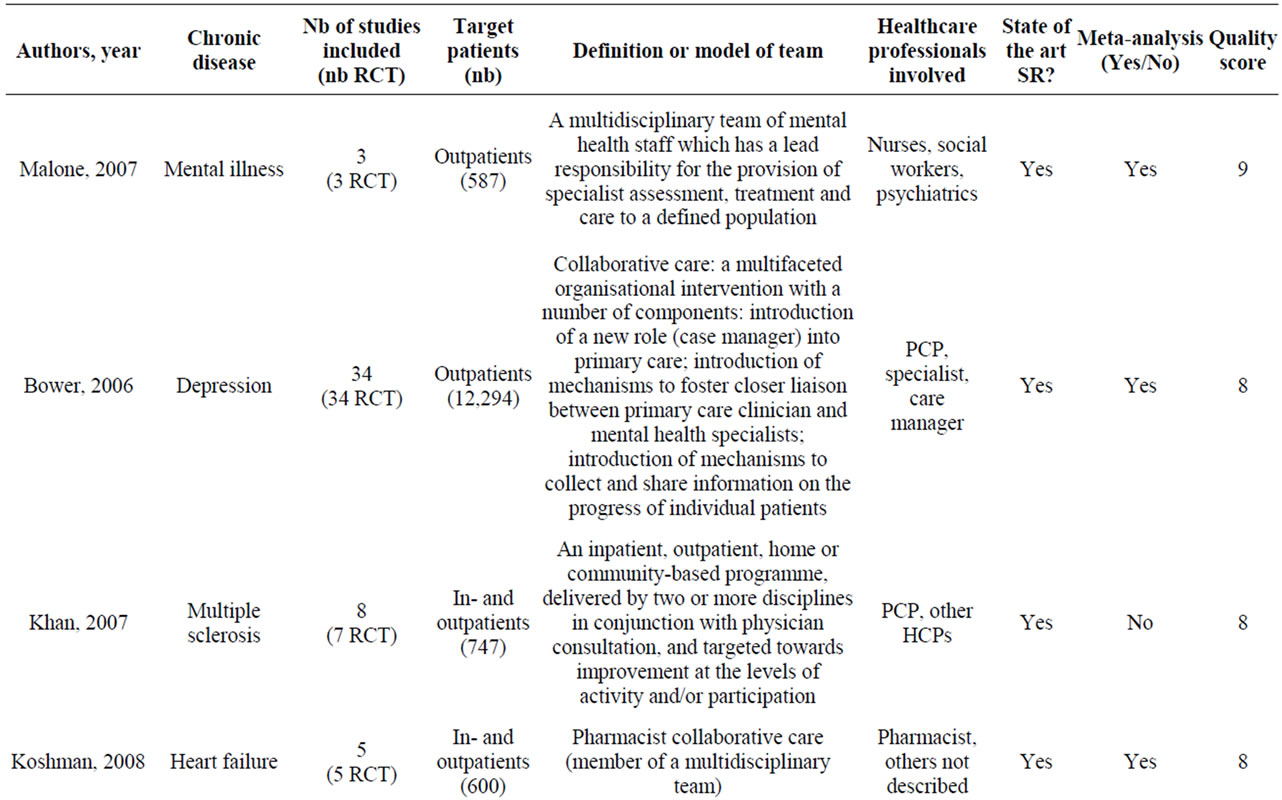

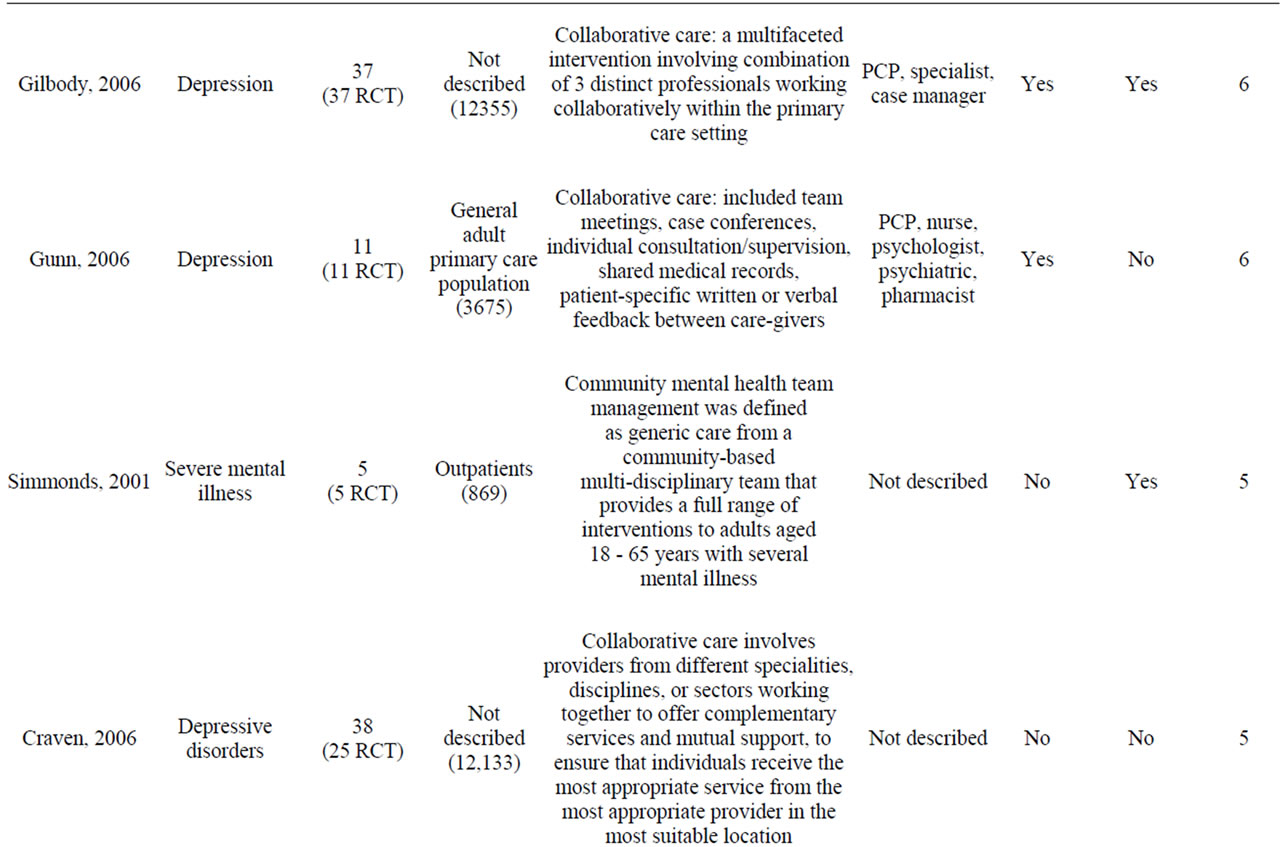
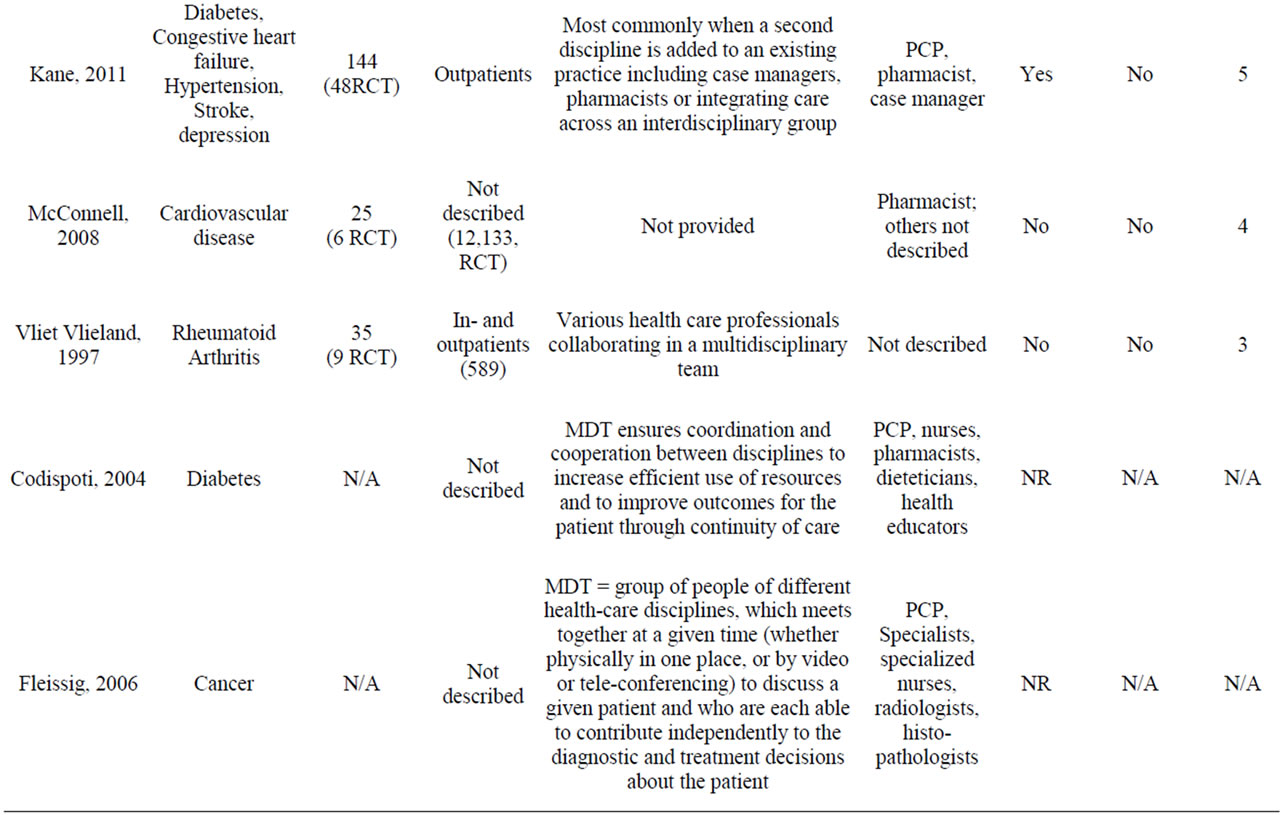
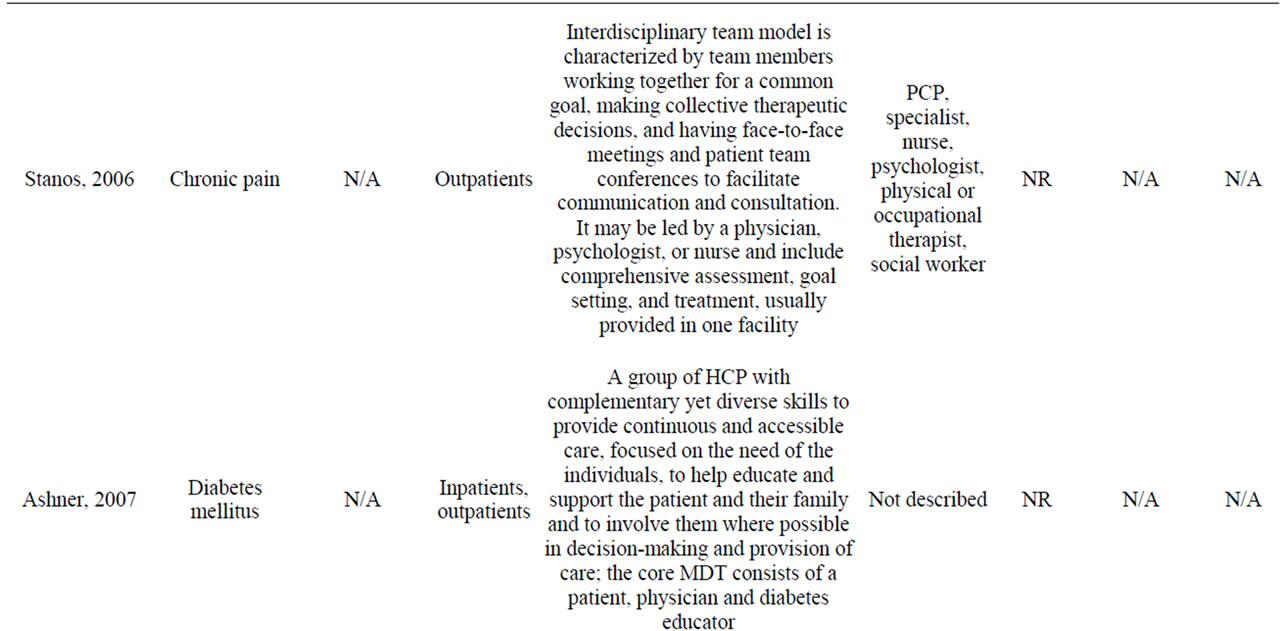

Table 3. Characteristics of reviews included.
intervention. However the pooled effect estimates were positive for all-cause hospitalization and heart failure. Smith et al. (2008) targeted various chronic diseases: 61% (25/41) of the studies favoured the intervention thus this review should be categorized as “teamwork possibly effective” instead of “teamwork not effective” based on the conclusion of the authors of the review.
3.2.3. Medium Quality Reviews
In the review of Mitchell et al. (2008) on stroke, classified as inconclusive, only 25% (2/8) of the studies favoured the intervention. The review of Ravenek et al. (2010) on chronic low back pain had a similar conclusion with only 21% (6/28). In the review of McAlister et al. (2004), there is evidence to support the conclusion that teamwork is effective for the following outcomes: all-cause mortality (RR = 0.75, CI 0.59 - 0.96), all-cause hospitalization (RR = 0.81, CI 0.71 - 0.91), heart failure hospitalizations (RR = 0.74, CI 0.63 - 0.87). However, only 49% (43/87) favoured the intervention when all outcomes were considered. Holland et al. (2005) reviewed heart failure RCT studies and 71% (34/48) of them favoured the intervention. The pooled effect estimate was significant for all-cause mortality (RR 0.79 CI 0.69 - 0.92), for all-cause hospital admissions (RR 0.87 CI 0.79 - 0.95), and for heart failure hospital admissions
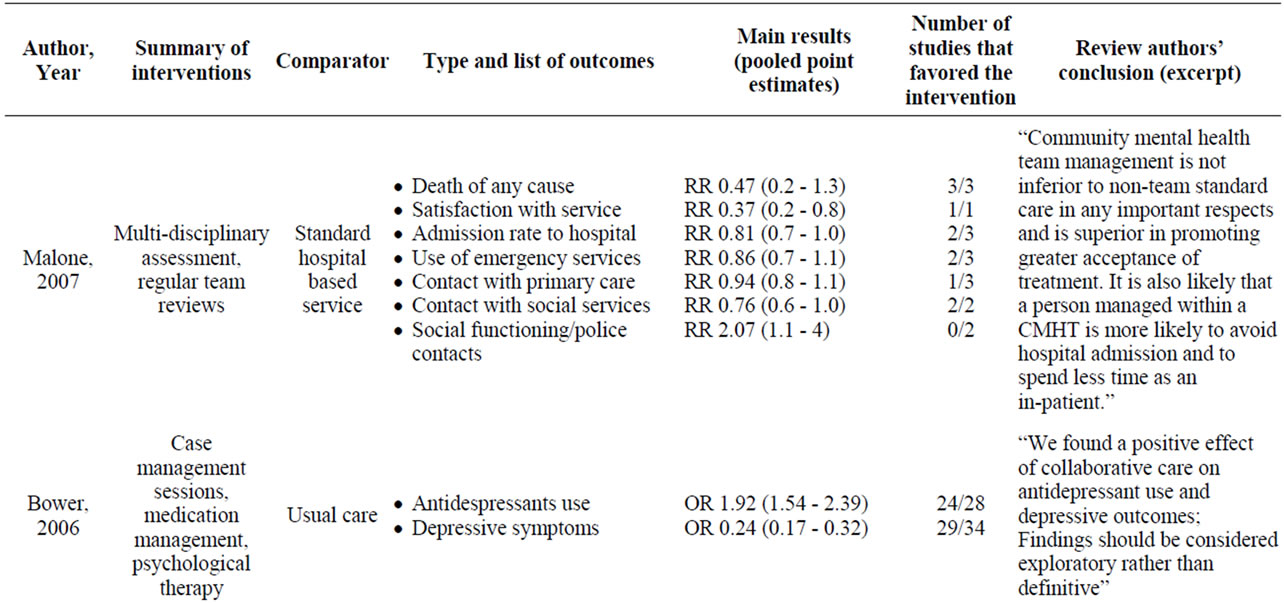
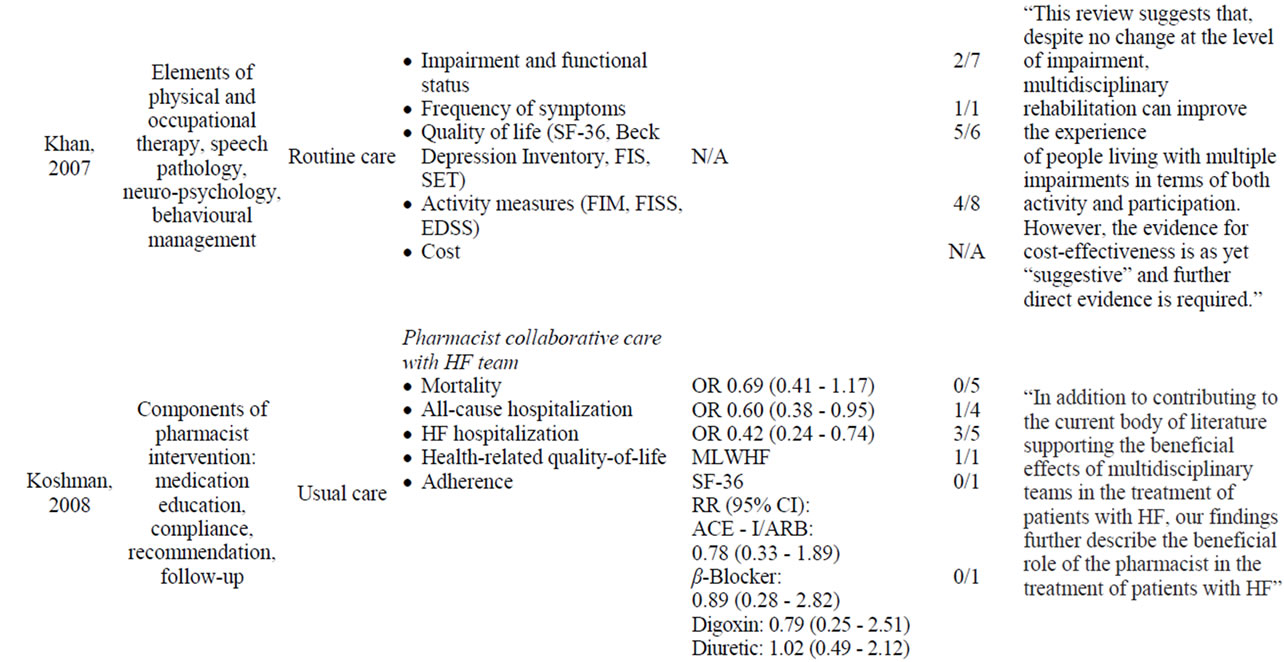
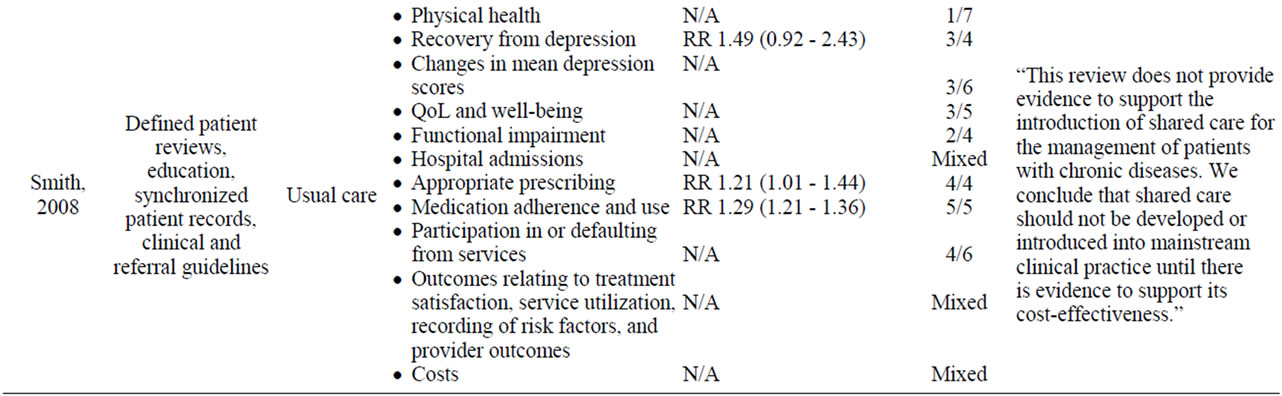
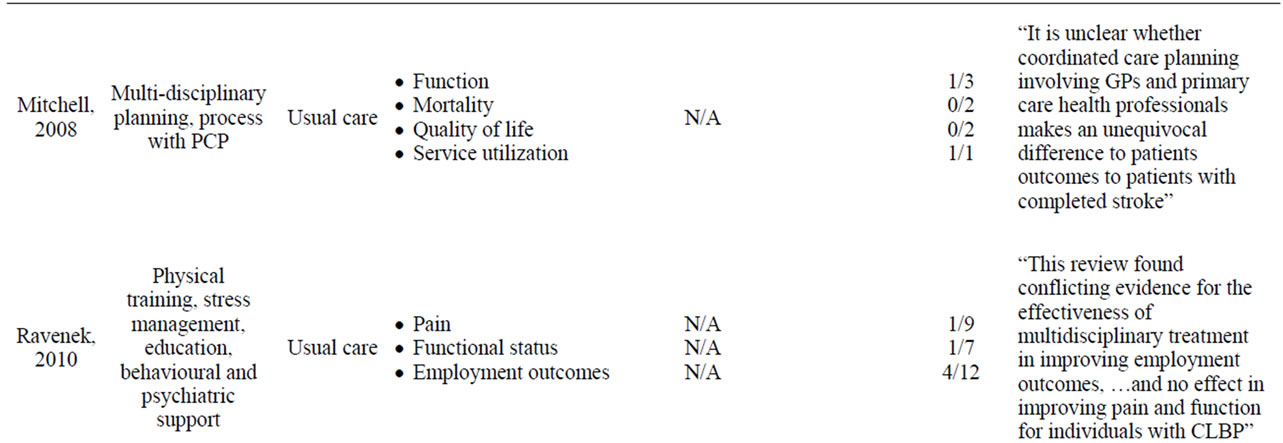
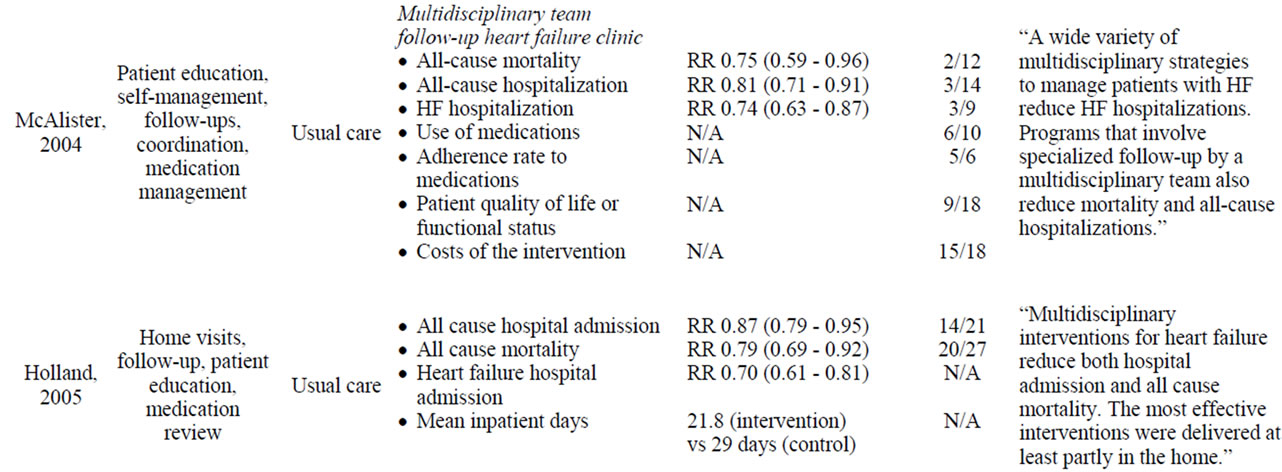
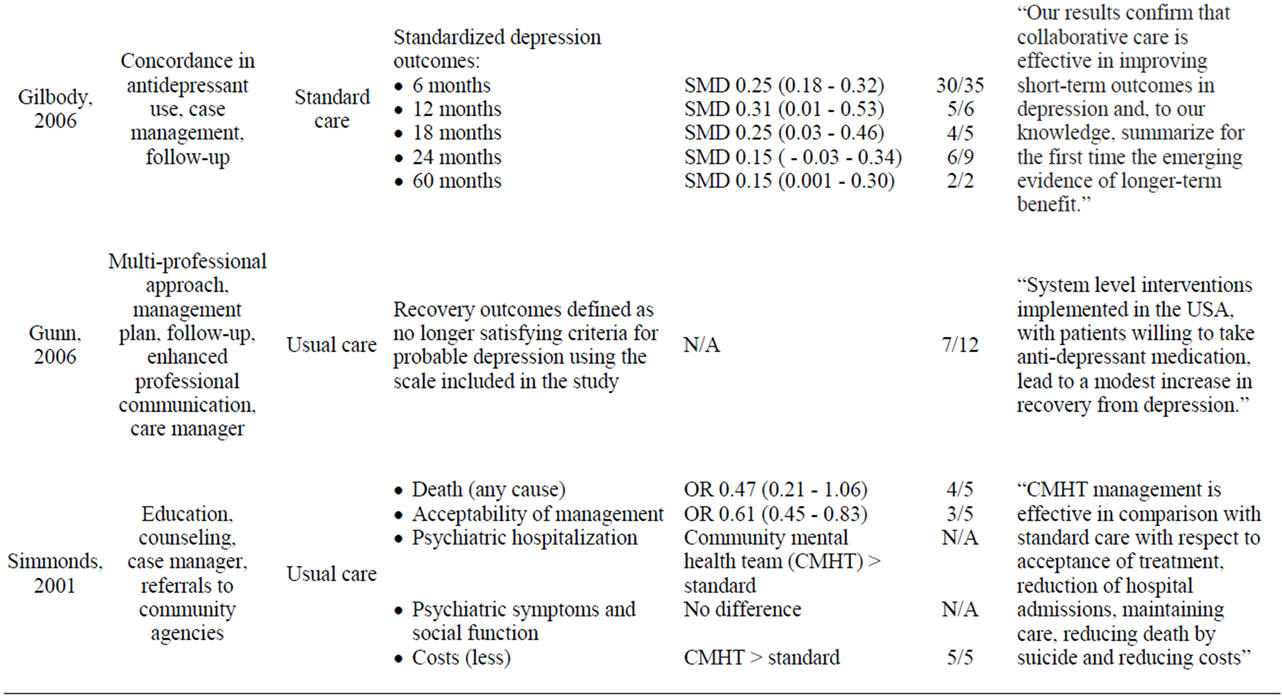
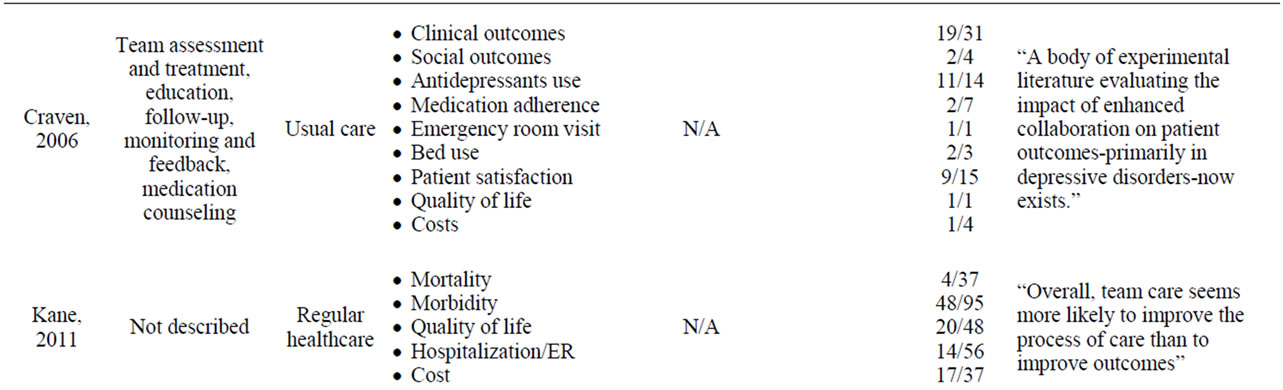
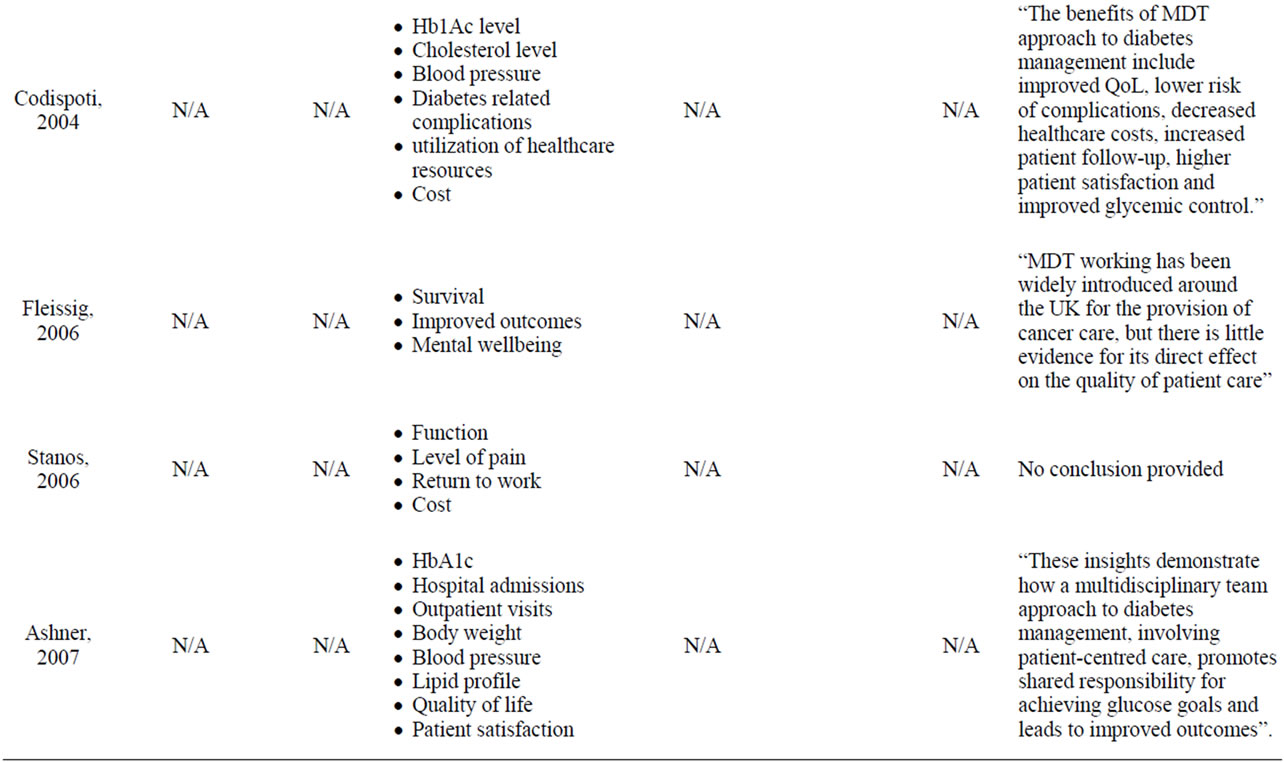

Table 4. Summary of results of the reviews.
(RR 0.70 CI 0.61 - 0.81), confirming the effectiveness of teamwork. In the review of Gilbody et al. (2006) on depression, the evidence retrieved confirmed the conclusion of teamwork effective with 83% (47/57) of the studies favouring the intervention; e.g. SMD was 0.25 CI 0.18 - 0.32 for depression outcomes at 6 months. The PSFI was 58% (7/12) for the review of Gunn et al. (2006) on depression that was classified as teamwork possibly effective. In Simmonds et al. (2001) on severe mental illnesses, 80% (12/15) of the studies favoured the intervention. The intervention was superior to standard care for death (all cause), acceptability of management, psychiatric hospitalization and costs outcomes. No difference was found for psychiatric symptoms and social function outcomes. In the review of Craven & Bland (2006) on depressive disorders that was classified as “teamwork possibly effective”, 60% (48/80) of the studies favoured the intervention. The review of Kane et al. (2011), reporting on multiple chronic disease, was inconclusive with 38% of positive results. The review of McConnell et al. (2008) on cardiovascular disease concluded that teamwork was effective which was confirmed by the 89% of the studies favoured the intervention.
3.2.4. Low Quality Reviews
In the review of Vliet Vlieland & Hazes (1997) on rheumatoid arthritis classified as inconclusive, 71% (5/7) of the studies’ favoured the intervention on clinical outcomes and no differences for resource utilization outcomes.
Seven narrative reviews were included in the overview. Based on the conclusion of the authors of the reviews, four concluded that teamwork was effective; one review found teamwork possibly effective; and, one was classified as inconclusive. The seventh review was disregarded because no conclusion was provided by the authors (Table 4).
4. Discussion
The findings of this overview do not provide unequivocal evidence that team care is universally effective in improving patient clinical care and outcomes. However, despite the limited number of reviews, the weight of cumulative results is suggestive of positive clinical and resource utilization impacts in the multidisciplinary management of several prevalent chronic diseases, namely: heart failure, depression and diabetes.
To our knowledge, no previous systematic overview has addressed the specific question of the efficacy/effectiveness of team care in chronic disease management. However, in a review of systematic reviews [55] of integrated care programs, with multidisciplinary patient care teams as a component in some of the included reviews, the investigators did report mixed results for costs and mortality outcomes; and, positive results for hospitalization, quality of life and patient satisfaction outcomes. Many unstructured reviews have also supported the benefits of health teams in terms of organisational, team members’ and patients’ perceived benefits [4].
Although the determinants of teamwork effectiveness were rarely assessed in the reviews analysed for this paper, the findings were in line with other previously reported results [8,15,56,57]. In particular, professional hierarchies, lack of leadership, poor communications and inter-team relations; and, incomplete knowledge of abilities and roles are the most frequently perceived factors to have negative impact on teams’ effectiveness [10,11].
Another important aspect of teamwork effectiveness and uptake is the model of remuneration or the provision of incentives. The model of reimbursement has been described in two reviews [43,51] as one of the barriers to collaborative care. Experiences in Australia and UK with new reimbursement models have been linked to team performance [15]. In Canada, health officials are increasingly advocating the benefits of interdisciplinary models and providing incentives to health professionals [58].
Finally, no conclusions could be drawn on the relationship between the level of efficiency of teamwork or the intensity of the interventions and effectiveness of patient outcomes.
Our study has several limitations. Many review papers that have examined the effectiveness of disease management programs for various chronic diseases were excluded because they did not report separate results for a multidisciplinary team care component. Thus, effects of team care could therefore not be assessed specifically. Also, in our overview, limited numbers of reviews precluded disease-specific comparisons. Another potential limitation is that vote counting, based on direction of effect and statistical significance, can disregard sample size (number of studies) and be, therefore misleading [59]. And, we did not include subjective outcome measurements for team effectiveness, which often relate to attitudinal aspects measured by team members, such as perceptions of their own team functioning [15,56]. Lastly, the methodological challenges of conducting an overview of reviews are worth noting. Only one quality assessment tool and two methodological papers are currently available for guidance [60]. Further methods need to be developed for this new form of knowledge synthesis, particularly analytical methods that take into consideration the doubling of individual studies between the reviews, the original conclusions of the component reviews, as well as the quality of evidence.
5. Conclusion
Our systematic overview add to the growing body of evidence suggesting health care teams can have beneficial impact on clinical and health resource endpoints. However, because of the limitations cited, the findings do not provide unqualified evidence of the effectiveness of team care in improving clinical outcomes in the context of chronic disease management. Further studies that examine the causal relations between multidisciplinary team care and clinical and economic outcomes of disease management programs are needed to more accurately assess its efficacy in terms of public health and cost efficiency.
REFERENCES
- J. Selby, D. Scanlon, J. Lafata, V. Villagra, J. Beich and P. Salber, “Determining the Value of Disease Management Programs,” Joint Commission Journal on Quality and Patient Safety, Vol. 29, No. 9, 2003, pp. 491-499.
- E. H. Wagner, “Chronic Disease Management: What Will It Take to Improve Care for Chronic Illness?” Effective Clinical Practice, Vol. 1, No. 1, 1998, pp. 2-4.
- N. J. Allen and T. D. Hecht, “The ‘Romance of Teams’: Toward an Understanding of Its Psychological Underpinnings and Implications,” Journal of Occupational & Organizational Psychology, Vol. 77, No. 439, 2004, pp. 439-461. doi:10.1348/0963179042596469
- S. M. Mickan, “Evaluating the Effectiveness of Health Care Teams,” Australian Health Review, Vol. 29, No. 2, 2005, pp. 211-217. doi:10.1071/AH050211
- R. F. Schofield and M. Amodeo, “Interdisciplinary Teams in Health Care and Human Services Settings: Are They Effective?” Health & Social Work, Vol. 24, No. 3, 1999, pp. 210-219. doi:10.1093/hsw/24.3.210
- Centers for Disease Control and Prevention, “Team Care: Comprehensive Lifetime Management for Diabetes,” US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Atlanta, 2001.
- C. Codispoti, M. R. Douglas, T. McCallister and A. Zuniga, “The Use of a Multidisciplinary Team Care Approach to Improve Glycemic Control and Quality of Life by the Prevention of Complications among Diabetic Patients,” The Journal of the Oklahoma State Medical Association, Vol. 97, No. 5, 2004, pp. 201-204.
- Institute of Medicine, “Crossing the Quality Chasm: A New Health System for the 21st Century,” National Academy Press, Washington DC, 2001.
- C. Borrill, “Team Working and Effectiveness in Health Care,” British Journal of Health Care, Vol. 6, No. 8, 2000, pp. 364-371.
- S. L. Dieleman, K. B. Farris, D. Feeny, J. A. Johnson, R. T. Tsuyuki and S. Brilliant, “Primary Health Care Teams: Team Members’ Perceptions of the Collaborative Process,” Journal of Interprofessional Care, Vol. 18, No. 1, 2004, pp. 75-78. doi:10.1080/13561820410001639370
- R. Lichtenstein, J. A. Alexander, J. F. McCarthy and R. Wells, “Status Differences in Cross-Functional Teams: Effects on Individual Member Participation, Job Satisfaction, and Intent to Quit,” Journal of Health and Social Behavior, Vol. 45, No. 3, 2004, pp. 322-335. doi:10.1177/002214650404500306
- A. Opie, “Effective Team Work in Health Care: A Review of Issues Discussed in Recent Research Literature,” Health Care Analysis, Vol. 5, No. 1, 1997, pp. 62-70. doi:10.1007/BF02678456
- C. Sevin, G. Moore, J. Shepherd, T. Jacobs and C. Hupke, “Transforming Care Teams to Provide the Best Possible Patient-Centered, Collaborative Care,” The Journal of Ambulatory Care Management, Vol. 32, No. 1, 2009, pp. 24-31.
- S. Ahmed, A. Gogovor, E. Berman, M. Miloff, B. Burnand, M. Krelenbaum and T. Montague, “Changing Healthcare: Stakeholder Perceptions of the Burden of Chronic Disease and the Value of Teams, Measurements and Communication,” Healthcare Quarterly, Vol. 12, No. 2, 2009, pp. e1-e13.
- I. Oandasan, R. G. Baker, K. Barker, C. Bosco, D. D’Amour, L. Jones, S. Kimpton, L. Lemieux-Charles, L. Nasmith, L. San Martin Rodriguez, J. Tepper and D. Way, “Teamwork in Health Care: Promoting Effective Teamwork in Health Care in Canada. Policy Synthesis and Recommendations,” Canadian Health Services Research Foundation, Ottawa, 2006.
- E. H. Wagner, “The Role of Patient Care Teams in Chronic Disease Management,” British Medical Journal, Vol. 320, No. 7234, 2000, pp. 569-572. doi:10.1136/bmj.320.7234.569
- H. Temkin-Greener, D. Gross, S. J. Kunitz and D. Mukamel, “Measuring Interdisciplinary Team Performance in a Long-Term Care Setting,” Medical Care, Vol. 42, No. 5, 2004, pp. 472-481. doi:10.1097/01.mlr.0000124306.28397.e2
- Care Continuum Alliance, “Definition of Disease Management,” 2011. http://www.carecontinuum.org/dm_definition.asp
- G. Ellrodt, D. Cook, J. Lee, M. Cho, D. Hunt and S. Weingarten, “Evidence-Based Disease Management,” Journal of the American Medical Association, Vol. 278, No. 20, 1997, pp. 1687-1692. doi:10.1001/jama.278.20.1687
- R. Epstein and L. Sherwood, “From Outcomes Research to Disease Management: A Guide for the Perplexed,” Annals of Internal Medicine, Vol. 124, 1996, pp. 832-837.
- D. Faxon, L. Schwamm, R. Pasternak, E. Peterson, B. McNeil, V. Bufalino, C. Yancy, L. Brass, D. Baker, R. Bonow, L. Smaha, D. Jones, S. J. Smith, G. Ellrodt, J. Allen, S. Schwartz, G. Fonarow, P. Duncan, K. Horton, R. Smith, S. Stranne and K. Shine, “Improving Quality of Care through Disease Management: Principles and Recommendations from the American Heart Association’s Expert Panel on Disease Management,” Stroke, Vol. 35, No. 6, 2004, pp. 1527-1530. doi:10.1161/01.STR.0000128373.90851.7B
- S. L. Norris, R. E. Engelgau, M. Michael, P. J. O’Connor and D. McCulloch, “Chronic Disease Management: A Definition and Systematic Approach to Component Interventions,” Disease Management Health Outcomes, Vol. 11, No. 8, 2003, pp. 477-488. doi:10.2165/00115677-200311080-00001
- D. A. Turnbull, H. Mensforth, J. J. Beilby, J. E. Marley, F. Qureshi and A. L. Tonkin, “An Empirical Model for the Development of Disease Management Programs in General Practice: A Case Study Using Hypertension,” Disease Management Health Outcomes, Vol. 10, No. 11, 2002, pp. 723-729. doi:10.2165/00115677-200210110-00006
- I. Peytremann-Bridevaux and B. Burnand, “Disease Management: A Proposal for a New Definition,” International Journal of Integrated Care, Vol. 9, 2009, p. e16.
- P. Kekki, “Teamwork in Primary Care,” World Health Organization, 1990.
- J. P. T. Higgins and S. Green, “Cochrane Handbook for Systematic Reviews of Interventions,” J. P. T. Higgins and S. Green, Eds., 2009. http://www.cochrane-handbook.org
- D. J. Cook, C. D. Mulrow and R. B. Haynes, “Systematic Reviews: Synthesis of Best Evidence for Clinical Decisions,” Annals of Internal Medicine, Vol. 126, No. 5, 1997, pp. 376-380.
- I. Gaboury, H. Boon, M. Verhoef, M. Bujold, L. M. Lapierre and D. Moher, “Practitioners’ Validation of Framework of Team-Oriented Practice Models in Integrative Health Care: A Mixed Methods Study,” BMC Health Services Research, Vol. 10, 2010, p. 289. doi:10.1186/1472-6963-10-289
- G. Johansson, K. Eklund and G. Gosman-Hedstrom, “Multidisciplinary Team, Working with Elderly Persons Living in the Community: A Systematic Literature Review,” Scandinavian Journal of Occupational, Vol. 17, 2010, pp. 101-116. doi:10.3109/11038120902978096
- B. J. Shea, J. M. Grimshaw, G. A. Wells, M. Boers, N. Andersson, C. Hamel, A. C. Porter, P. Tugwell, D. Moher and L. M. Bouter, “Development of AMSTAR: A Measurement Tool to Assess the Methodological Quality of Systematic Reviews,” BMC Medical Research Methodology, Vol. 7, 2007, p. 10. doi:10.1186/1471-2288-7-10
- B. J. Shea, L. M. Bouter, J. Peterson, M. Boers, N. Andersson, Z. Ortiz, T. Ramsay, A. Bai, V. K. Shukla and J. M. Grimshaw, “External Validation of a Measurement Tool to Assess Systematic Reviews (AMSTAR),” PLoS One, Vol. 2, No. 12, 2007, p. e1350. doi:10.1371/journal.pone.0001350
- B. J. Shea, C. Hamel, G. A. Wells, L. M. Bouter, E. Kristjansson, J. Grimshaw, D. A. Henry and M. Boers, “AMSTAR Is a Reliable and Valid Measurement Tool to Assess the Methodological Quality of Systematic Reviews,” Journal of Clinical Epidemiology, Vol. 62, No. 10, 2009, pp. 1013-1020. doi:10.1016/j.jclinepi.2008.10.009
- P. Bower, S. Gilbody, D. Richards, J. Fletcher and A. Sutton, “Collaborative Care for Depression in Primary Care. Making Sense of a Complex Intervention: Systematic Review and Meta-Regression,” British Journal of Psychiatry, Vol. 189, 2006, pp. 484-493. doi:10.1192/bjp.bp.106.023655
- M. A. Craven and R. Bland, “Better Practices in Collaborative Mental Health Care: An Analysis of the Evidence Base,” Canadian Journal of Psychiatry, Vol. 51, No. 6, 2006, pp. 7S-72S.
- S. Gilbody, P. Bower, J. Fletcher, D. Richards and A. J. Sutton, “Collaborative Care for Depression: A Cumulative Meta-Analysis and Review of Longer-Term Outcomes,” Archives of Internal Medicine, Vol. 166, No. 21, 2006, pp. 2314-2321. doi:10.1001/archinte.166.21.2314
- J. Gunn, J. Diggens, K. Hegarty and G. Blashki, “A Systematic Review of Complex System Interventions Designed to Increase Recovery from Depression in Primary Care,” BMC Health Services Research, Vol. 6, 2006, p. 88. doi:10.1186/1472-6963-6-88
- R. Holland, J. Battersby, I. Harvey, E. Lenaghan, J. Smith and L. Hay, “Systematic Review of Multidisciplinary Interventions in Heart Failure,” Heart, Vol. 91, No. 7, 2005, pp. 899-906. doi:10.1136/hrt.2004.048389
- R. L. Kane, T. A. Shamliyan and T. McCarthy, “Do Geriatric Healthcare Teams Work?” Aging Health, Vol. 7, 2011, pp. 865-876. doi:10.2217/ahe.11.68
- F. Khan, L. Turner-Stokes, L. Ng and T. Kilpatrick, “Multidisciplinary Rehabilitation for Adults with Multiple Sclerosis,” Cochrane Database of Systematic Reviews, No. 4, 2007, Article ID: CD006036.
- S. L. Koshman, T. L. Charrois, S. H. Simpson, F. A. McAlister and R. T. Tsuyuki, “Pharmacist Care of Patients with Heart Failure: A Systematic Review of Randomized Trials,” Archives of Internal Medicine, Vol. 168, No. 7, 2008, pp. 687-694. doi:10.1001/archinte.168.7.687
- D. Malone, G. Newron-Howes, S. Simmonds, S. Marriot and P. Tyrer, “Community Mental Health Teams (CMHTs) for People with Severe Mental Illnesses and Disordered Personality,” Cochrane Database of Systematic Reviews, No. 3, 2007, Article ID: CD000270.
- F. A. McAlister, S. Stewart, S. Ferrua and J. J. McMurray, “Multidisciplinary Strategies for the Management of Heart Failure Patients at High Risk for Admission: A Systematic Review of Randomized Trials,” Journal of the American College of Cardiology, Vol. 44, No. 4, 2004, pp. 810-819. doi:10.1016/j.jacc.2004.05.055
- K. J. McConnell, A. M. Denham and K. L. Olson, “Pharmacist-Led Interventions for the Management of Cardiovascular Disease: Opportunities and Obstacles,” Disease Management and Health Outcomes, Vol. 16, No. 3, 2008, pp. 131-144. doi:10.2165/00115677-200816030-00001
- G. K. Mitchell, R. M. Brown, L. Erikssen and J. J. Tieman, “Multidisciplinary Care Planning in the Primary Care Management of Completed Stroke: A Systematic Review,” BMC Family Practice, Vol. 9, 2008, p. 44. doi:10.1186/1471-2296-9-44
- M. J. Ravenek, I. D. Hughes, N. Ivanovich, K. Tyrer, C. Desrochers, L. Klinger and L. Shaw, “A Systematic Review of Multidisciplinary Outcomes in the Management of Chronic Low Back Pain,” Work, Vol. 35, No. 3, 2010, pp. 349-367.
- S. Simmonds, J. Coid, P. Joseph, S. Marriott and P. Tyrer, “Community Mental Health Team Management in Severe Mental Illness: A Systematic Review,” British Journal of Psychiatry, Vol. 178, 2001, pp. 497-502. doi:10.1192/bjp.178.6.497
- S. M. Smith, S. Allwright and T. O’Dowd, “Does Sharing Care Across the Primary-Specialty Interface Improve Outcomes in Chronic Disease? A Systematic Review,” American Journal of Managed Care, Vol. 14, No. 4, 2008, pp. 213-224.
- T. P. Vliet Vlieland and J. M. Hazes, “Efficacy of Multidisciplinary Team Care Programs in Rheumatoid Arthritis,” Seminars in Arthritis and Rheumatism, Vol. 27, No. 2, 1997, pp. 110-122. doi:10.1016/S0049-0172(97)80011-X
- P. Aschner, J. LaSalle and M. McGill, “The Team Approach to Diabetes Management: Partnering with Patients,” International Journal of Clinical Practice, No. 157, 2007, pp. 22-30. doi:10.1111/j.1742-1241.2007.01606.x
- A. Fleissig, V. Jenkins, S. Catt and L. Fallowfield, “Multidisciplinary Teams in Cancer Care: Are They Effective in the UK?” Lancet Oncology, Vol. 7, No. 11, 2006, pp. 935-943. doi:10.1016/S1470-2045(06)70940-8
- L. M. Kalisch, E. E. Roughead and A. L. Gilbert, “Improving Heart Failure Outcomes with PharmacistPhysician Collaboration: How Close Are We?” Future Cardiology, Vol. 6, 2010, pp. 255-268. doi:10.2217/fca.09.67
- W. J. Katon and M. Seelig, “Population-Based Care of Depression: Team Care Approaches to Improving Outcomes,” Journal of Occupational & Environmental Medicine, Vol. 50, No. 4, 2008, pp. 459-467. doi:10.1097/JOM.0b013e318168efb7
- S. Stanos and T. T. Houle, “Multidisciplinary and Interdisciplinary Management of Chronic Pain,” Physical Medicine & Rehabilitation Clinics of North America, Vol. 17, No. 2, 2006, pp. 435-450. doi:10.1016/j.pmr.2005.12.004
- S. Vannoy, D. Powers and J. Ã. Unützer, “Models of Care for Treating Late-Life Depression in Primary Care,” Aging Health, Vol. 3, No. 1, 2007, pp. 67-75. doi:10.2217/1745509X.3.1.67
- M. Ouwens, H. Wollersheim, R. Hermens, M. Hulscher and R. Grol, “Integrated Care Programmes for Chronically Ill Patients: A Review of Systematic Reviews,” International Journal for Quality in Health Care, Vol. 17, No. 2, 2005, pp. 141-146. doi:10.1093/intqhc/mzi016
- L. Lemieux-Charles and W. L. McGuire, “What Do We Know about Health Care Team Effectiveness? A Review of the Literature,” Medical Care Research and Review, Vol. 63, No. 3, 2006, pp. 263-300. doi:10.1177/1077558706287003
- B. C. Poulton and M. A. West, “The Determinants of Effectiveness in Primary Health Care Teams,” Journal of Interprofessional Care, Vol. 13, No. 1, 1999, pp. 7-18. doi:10.3109/13561829909025531
- S. Khan, C. McIntosh, C. Sanmartin, D. Watson and K. Leeb, “Primary Health Care Teams and Their Impact on Processes and Outcomes of Care,” Statistics Canada, 2008.
- C. Pope, N. Mays and J. Popay, “Synthesizing Qualitative and Quantitative Health Evidence: A Guide to Methods,” Open University Press, McGraw Hill Education, New York, 2007.
- V. Smith, D. Devane, C. M. Begley and M. Clarke, “Methodology in Conducting a Systematic Review of Systematic Reviews of Healthcare Interventions,” BMC Medical Research Methodology, Vol. 11, No. 1, 2011, p. 15. doi:10.1186/1471-2288-11-15

