Open Journal of Psychiatry
Vol.4 No.3(2014), Article ID:47957,12 pages
DOI:10.4236/ojpsych.2014.43030
The Cost-Effectiveness of Short-Term Psychodynamic Psychotherapy and Solution-Focused Therapy in the Treatment of Depressive and Anxiety Disorders during a Three-Year Follow-Up
Timo Maljanen1, Tommi Härkänen2, Esa Virtala2, Olavi Lindfors2, Päivi Tillman1, Paul Knekt2,3
1Social Insurance Institution, Helsinki, Finland
2National Institute for Health and Welfare, Helsinki, Finland
3Biomedicum Helsinki, Helsinki, Finland
Email: timo.maljanen@kela.fi
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 10 May 2014; revised 12 June 2014; accepted 16 July 2014
ABSTRACT
Background: Various psychotherapies are used extensively in treating different mental disorders, but still relatively little is known about the long-term health and cost effects of different therapies. The aim of this study is to compare the cost-effectiveness of short-term psychodynamic psychotherapy (SPP) and solution-focused therapy (SFT) in the treatment of depressive and anxiety disorders during a three-year follow-up. Methods: A total of 198 outpatients suffering from mood or anxiety disorder were randomized to SPP or SFT. Symptoms were assessed using the Beck Depression Inventory, the Hamilton Depression Rating Scale, the Symptom Check List Anxiety Scale, the Hamilton Anxiety Rating Scale, and the Symptom Check List Global Severity Index. Both direct and indirect costs due to mental health problems were measured. Results: The symptoms of depression and anxiety were reduced statistically significantly according to all 5 psychiatric outcome measures during the first 7 months, after which only minor changes were observed. The differences between the two groups were small and not statistically significant. The direct costs were about equal in both groups but the indirect costs were somewhat higher in the SPP group, although not statistically significantly. The costs of auxiliary treatments were much higher than the cost of SPP or SFT. Conclusions: With regard to cost-effectiveness, there is little difference between SPP and SFT.
Keywords:Depression, Anxiety, Psychotherapy, Cost Analysis

1. Introduction
Numerous studies have demonstrated that short-term psychotherapies are effective in the treatment of mood and anxiety disorders, and in meta-analyses no significant differences in the effectiveness of different types of shortterm psychotherapies have been observed [1] [2] . However, as mood and anxiety disorders are frequently recurrent, the results of these studies must be interpreted with some caution, for the follow-up periods have in most studies been relatively short. Besides that, more attention should have been paid to monitoring the use of auxiliary psychiatric treatments, which may have a crucial effect both on symptoms and costs, especially in the long run [3] . The effects of auxiliary treatments are usually taken into account in economic evaluations, but although the need for economic evaluations of psychotherapies has been recognized for years, the number of such evaluations has remained modest, and especially studies with longer follow-up periods are rare. In addition to the paucity of existing research, cost-effectiveness comparisons are complicated by the fact that there is remarkable heterogeneity in the study designs due to differences in control treatments, patient inclusion criteria and outcome measures, for example. Before any firm conclusions about the cost-effectiveness of different therapies can be made, more information is needed about the costs and effects of different therapies. The aim of this study is to enlarge our knowledge in this respect by producing a comprehensive view of the various direct and indirect costs arising when patients have been treated either with short-term psychodynamic psychotherapy (SPP) or solution-focused therapy (SFT), as well as to assess changes in symptoms utilizing several health outcome indicators during a 3-year follow-up period. The cost-effectiveness of short-term therapies has been evaluated in a handful of studies [4] [5] , but to our knowledge this is the first cost-effectiveness study where these two therapies are compared over a follow-up period covering several years.
2. Population and Methods
This cost-effectiveness study is a part of the Helsinki Psychotherapy Study [6] . The study follows the Helsinki Declaration and was approved by Helsinki University Central Hospital’s ethics council. Patients gave written informed consent at the beginning of the study. The study population and methods used in the study are summarized only briefly here as they have been described in detail elsewhere [3] [6] -[8] .
2.1. Patients and Settings
A total of 459 eligible and willing outpatients from the Helsinki region were referred for the Helsinki Psychotherapy Study from 1994 to 2000. Eligible patients were 20 - 45 years of age and had a longstanding (>1 year) disorder causing work dysfunction. The patients had to meet DSM-IV criteria [9] for anxiety or mood disorders. For the criteria of exclusion, see Knekt et al. [6] . Of the eligible patients, 133 refused to participate, and the remaining 326 patients were randomly assigned to short-term psychodynamic psychotherapy (SPP) (101 patients), solution-focused therapy (SFT) (97 patients), and long-term psychodynamic psychotherapy (LPP) (128 patients). The LPP group was not included in this study because the three-year follow-up was deemed to be too short to cover the long-run effects of LPP, i.e., how symptoms and costs develop after the end of therapy. After assignment to treatment groups 3 SPP patients and 4 SFT patients refused to participate. Of the patients starting the assigned therapy, 21 (10 assigned to SPP and 11 to SFT) discontinued the treatment prematurely.
2.2. Treatments
2.2.1. Therapies
SPP is a brief, focal, transference based therapeutic approach which helps patients by exploring and working through specific intrapsychic and interpersonal conflicts. It is based on approaches described by Malan [10] and Sifneos [11] . SPP was scheduled for 20 treatment sessions, each lasting about 45 minutes with a frequency of one session per week. The SPP sessions were carried out, on average, over a period of 5.7 months (SD = 1.3).
SFT is a brief, resource oriented, goal focused therapeutic approach which helps clients change by constructing solutions [12] . It is based on an approach developed by de Shazer et al. [13] . The frequency of SFT sessions was flexible, usually one 60 to 90 minute session every two or three weeks for a maximum of up to 12 sessions over no more than 8 months. The mean duration of SFT was 7.5 months (SD = 3.0).
2.2.2. Therapists
SPP was provided by 12 therapists and SFT by 6 therapists. All therapists had received standard training in their respective forms of therapy. The mean number of years of experience in the therapy provided was 9 for both therapy forms. SPP was conducted in accordance with clinical practice, where the therapists might modify their interventions according to the patient’s needs within the respective framework. None of the SPP therapists had received any training in SFT and vice versa. SFT was manualized and adherence monitoring was performed.
2.3. Assessment
2.3.1. Effectiveness
Effectiveness was measured by changes in psychiatric symptoms. Symptoms of depression were assessed with the Beck Depression Inventory (BDI) [14] and the Hamilton Depression Rating Scale (HDRS) [15] . Symptoms of anxiety were assessed with the Symptom Check List Anxiety Scale (SCL-90-ANX) [16] and the Hamilton Anxiety Rating Scale (HARS) [17] . Overall psychological distress was measured using the Symptom Check List Global Severity Index (SCL-90-GSI) [16] . Assessments based on self-administered questionnaires (BDI, SCL- 90-ANX and SCL-90-GSI) were carried out at baseline and at 3, 7, 9, 12, 18, 24, and 36 months after baseline, while assessments based on interviews (HDRS and HARS) were performed at baseline and at follow-up points of 7, 12 and 36 months.
2.3.2. Costs
Altogether four different total cost components were estimated in this study. The most important of the four were the direct costs due to the treatment of mental disorders, which included costs accruing from 1) protocolbased and additional SPP and SFT sessions, 2) other psychotherapy sessions, 3) outpatient visits due to mental disorders, 4) psychotropic medication (prescription-only medicines), 5) inpatient care due to mental disorders, and 6) travel costs due to therapy visits. The indirect costs caused by mental disorders included 1) the value of lost productivity due to absenteeism from work because of psychiatric problems or 2) therapy visits, 3) the value of household work neglected because of psychiatric problems, 4) the value of leisure time lost due to therapy visits, and 5) the value of unpaid help received because of mental disorders. Direct costs due to non-mental disorders consisted of the cost of treatments (outpatient visits, inpatient care, and prescription-only medicines) for somatic disorders. Indirect costs due to non-mental disorders consisted of the value of lost productivity due to absenteeism from work and the value of household work neglected because of somatic problems.
Part of the cost data was readily available in monetary terms from patient registers covering all patients. Most of the cost items were estimated by multiplying the amount of services used by the corresponding unit costs. Information about the amounts of different services used was obtained either from patient level registers or from the patients themselves in five inquiries, which covered 0 - 7, 8 - 12, 13 - 18, 19 - 24 and 25 - 36 months’ periods from the start of the therapy. All costs were included in the analysis in full regardless of the payer. All costs were converted to the 2010 price level by using official price indices. The costs were discounted by using a three percent yearly discount rate. Details of estimation of costs are described in Maljanen et al. [8] .
2.3.3. Potential Confounding Factors
At baseline, demographic characteristics (age, sex, marital status, and education) and previous psychiatric treatments (medication, psychotherapy and hospitalization) were assessed by questionnaire, and suitability for psychotherapy [18] , as well as factors related to psychiatric history (age at onset of first psychiatric disorder, childhood separation experiences), by interview.
2.4. Statistical Methods
2.4.1. Effectiveness
The effectiveness of the two therapies was studied in a design with repeated measurements of the outcome variables as “intention-to-treat” (ITT) analyses [6] [19] . The primary analyses were based on the assumption of ignorable dropouts, and in secondary analyses missing values were replaced by multiple imputation (MI) [20] [21] . The statistical analyses were based on linear mixed models, model-adjusted means and mean differences calculated using predictive margins [22] [23] . See Maljanen et al. for details [8] .
The regression model for the effectiveness outcome assessed by repeated measurements included the main effects of time, treatment group, difference between theoretical and realized date of measurement, and first order interaction of time and treatment group [6] . Adjustment for the potential confounders was not found necessary.
2.4.2. Costs
The analyses of costs were based on comparisons of the arithmetic means of different cumulative cost items. Our earlier study [8] as well as many other studies have shown that due to the extremely high costs of some patients the distributions of cost variables are very skewed, and therefore the statistical analyses were performed using a non-parametric bootstrap approach [24] . In the cost analyses some of the missing values of cost variables were imputed using single-value imputation [8] . Potential confounding factors were not found in case of the cost outcomes, and thus the treatment group was the sole covariate in the model.
2.4.3. Cost-Effectiveness
The cost-effectiveness of the therapies was compared with the incremental cost-effectiveness
ratio (ICER) [25] , which is the difference in
the mean costs of the two therapies divided by the difference of their mean effectiveness,
i.e.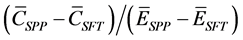 , where
, where
 stands for the mean costs and
stands for the mean costs and
 for the mean effectiveness of SPP, and
for the mean effectiveness of SPP, and
 and
and
 respectively for SFT.
respectively for SFT.
The effectiveness of the therapies was estimated by calculating the changes taken place in BDI, HDRS, SCL- 90-ANX, HARS and SCL-90-GSI during the three-year follow-up period. The calculation was based on the area under the curve (AUC), a frequently used tool in clinical trials with repeated measurements, which is the mean value of the clinical indicator during the follow-up period [26] . Changes in symptoms over the whole three-year follow-up period were estimated by subtracting the AUC value of each psychiatric measure from the baseline value of that measure. These estimates of the overall symptom changes are marked with the symbol B-AUC. The confidence intervals of differences in average costs and the ICERs were calculated using the bootstrap method [24] [27] . Both effectiveness and costs were discounted by using a three percent yearly discount rate.
The principles used in calculating ICERs were the same as those used in our earlier study with a one-year follow-up period [8] . As these methods have been described in detail in an earlier article, only the main points are taken up here.
In the cost-effectiveness analyses, missing data were handled with MI. The effect of missing data was assessed using multi-dimensional sensitivity analyses [28] . The proportion of missing AUC values, and hence also that of missing B-AUC values, was larger (23% - 42%) than the proportion of missing health outcome values of the single measurement points, because a missing value at any of the measurement points of a patient causes a missing value in the AUC value of such a patient.
The results of the cost-effectiveness analyses are presented using cost-effectiveness planes with bootstrap iterations. Depending on how the iteration points are spread out across the four quadrants one is able to draw conclusions about the uncertainty associated with the cost-effectiveness results.
2.4.4. Sensitivity Analysis
In the sensitivity analyses different methods of handling the problem of missing observations were utilized [29] . Due to the uncertainties associated with different imputation methods, analyses based solely on non-missing observations were also performed. Also unit costs whose values were uncertain were changed to test the robustness of the results of the basic analyses.
All statistical analyses were performed using SAS software version 9.2 [30] .
3. Results
3.1. Baseline Characteristics
The majority of the patients were females in their thirties who were employed or students and suffering from mood disorders (Table 1). Relatively few had received psychiatric treatment despite the fact that more than half
aMean (SD).
had experienced recurrent episodes of major depression and a relatively early onset of psychiatric disorder. There were no statistically significant differences between the treatment groups with respect to demographic characteristics or the patients’ baseline clinical status.
3.2. Effectiveness
During the period when the patients were receiving study therapy, i.e., during the first 7 months of the follow-up, the scores of the two outcome measures assessing the symptoms of depression (BDI and HDRS) as well as the scores of the two outcome measures assessing the symptoms of anxiety (SCL-90-ANX and HARS) declined statistically significantly in both therapy groups (Table 2). A very similar development was observed in the overall psychological distress measured by SCL-90-GSI (data not shown). From there to the end of the three-year follow-up period the mean scores of all symptom indicators remained quite stable in both groups. There were no statistically significant differences between the therapy groups at any point of the follow-up for any of the outcome measures. Hence also the differences in the overall symptom changes (B-AUC values) were small and not statistically significant.
3.3. Costs
After the single-value imputation of missing cost values, the share of non-missing observations varied, depending on the service used, from 75% (cost of psychiatric outpatient care in the SFT group) to 100% (costs of study therapy visits and psychotropic medication in both groups). Complete cost data, i.e., information about all cost items at every measurement point, were obtained from 79 SPP patients (78%) and from 72 SFT patients (74%). The mean total direct costs of patients with complete cost data were 4867 euros in the SPP group, being only marginally higher (by 29 euros, or 0.6%) than the costs in the SFT group (Table 3). If the total direct costs are
Table 2 . Mean health outcome scores (s.e.) and mean score differences (95% confidence interval) between treatment groups by follow-up: ITT, Model 1.
aBasic model. bBasic model adjusted for the baseline level of the outcome measure considered. cAccording to 500 bootstrap iterations. *A statistically significant improvement from previous measurement point.
calculated by summing up the mean costs of the different cost items shown in Table 3 the difference between the two groups turns out to be somewhat greater, with the total costs of the SPP group increasing to 5795 euros and the costs of the SFT group to 5306 euros. This difference was due to the fact that the patients in the SPP group used various auxiliary health care services more than or at least as much as the patients in the SFT group. During the three-year follow-up period the costs of all auxiliary health care services were in both groups much higher than the costs of study therapy: 247% and 98% higher, respectively, in the SPP and SFT groups. An overwhelming majority of patients in both groups, 83% in the SPP group and 82% in the SFT group, received some auxiliary treatments for their symptoms during the three-year follow-up period.
The largest cost item in both groups was auxiliary psychotherapy, which accounted for nearly 50% of all di
Table 3. Direct costs (euros) and resource use (in cursive and in parentheses) due to mental disorders in short-term psychodynamic psychotherapy and solution-focused therapy group during the three-year follow-up period: Analysis based on nonmissing observations of the single-value imputation data [n = number of patients with data at every measurement point].
aAccording to 500 bootstrap iterations. bHealth centre, occupational health care, mental health clinic, hospital outpatient clinic, private physician, etc. cInformation about the number of psychotherapy visits resulting in travel costs is not available. dTotal direct costs or the difference in total direct costs do not equal the sum of individual cost items because due to the varying number of missing observations the mean calculations of total costs and different cost items are partly based on different sets of patient data.
rect costs in both groups. The relatively high cost of other psychotherapy was explained by the fact that in both therapy groups there were some patients who had had numerous psychotherapy sessions not included in the study protocol.
In both groups the mean direct costs were highest at the beginning of the three-year follow-up period when patients were receiving study therapy. In the first year of the follow-up the mean costs of patients in the SFT group were higher than the mean costs of the SPP group because SFT itself cost more than SPP. During the first year the costs showed a steep declining trend in both groups, the reason being that the number of patients receiving study therapy continued to diminish. In the last two years of the follow-up the mean costs showed a growing trend in both therapy groups and, unlike in the first year, the costs of the SPP group were consistently higher (Figure 1).
The mean indirect costs due to mental disorders were, like the direct costs, higher in the SPP group (Table 4). The reasons for this cost difference of 4128 euros was that both the value of lost productivity due to absenteeism from work because of sickness and the value of unpaid help received because of mental health problems were clearly higher in the SPP group. The share of these two cost items of all indirect costs was about 80% in the SPP group and 70% in the SFT group. Also the value of lost leisure time due to therapy visits and the value of neglected household work were considerable. No statistically significant differences between the two groups were observed in any cost item. It is worth noticing that the indirect costs were in both groups higher than the direct costs.
During the three-year follow-up, mean direct costs due to non-mental disorders were about the same in both groups: 1838 euros in the SPP group and 1570 euros in the SFT group. This difference was not statistically significant. In both therapy groups nearly 80% of these costs were caused by outpatient visits to physicians. Also the mean indirect costs due to non-mental disorders were similar in the two therapy groups: 3957 euros in the SPP group and 4066 euros in the SFT group. In both groups the indirect costs were mainly due to lost productivity.
Figure 1. The mean monthly direct costs (euros) due to mental disorders in short-term psychodynamic psychotherapy and solution-focused therapy group during the three-year follow-up period.
Table 4. Indirect costs (euros) due to mental disorders in short-term psychodynamic psychotherapy and solution-focused therapy group during the three-year follow-up period: Analysis based on non-missing observations of the single-value imputation data [n = number of patients with data at every measurement point].
aAccording to 500 bootstrap iterations. bTotal indirect costs or the difference in total indirect costs do not equal the sum of individual cost items because due to the varying number of missing observations the mean calculations of total costs and different cost items are partly based on different sets of patient data.
3.4. Cost-Effectiveness
According to all five health outcome indicators the effectiveness of SPP seemed to be slightly better than that of SFT. The differences were, however, very small and as a result of this there is a lot of uncertainty in the ICERs. Due to this considerable uncertainty no point estimates or confidence intervals for this ratio were calculated. Instead, uncertainty associated with our results was analysed by running 500 ICER bootstrap iterations for each of the four health outcome measures assessing symptoms of depression or anxiety and direct costs (Figure 2). Because the cost outcome of these four analyses was the same, the locations of the iteration points with respect to the horizontal line were the same in all four Figures 2(a)-(d) excluding the variation caused by bootstrap iterations and imputation of missing values. Regardless of the outcome measure studied the iteration points are concentrated heavily around the origin and spread quite evenly among all four quadrants. Thus this cost-effective-

Figure 2. The incremental cost-effectiveness planes with 500 bootstrap iterations comparing short-term psychodynamic psychotherapy and solution-focused therapy: direct costs due to mental disorders as cost variable and BDI, HDRS, SCL-90-ANX and HARS as effectiveness variable.
ness analysis confirms our earlier findings that the differences between SPP and SFT are small both in terms of effectiveness and costs.
3.5. Sensitivity Analysis
In the sensitivity analyses we tested different imputation methods and changed the unit cost of those resources whose unit costs were known to be uncertain. The results for effectiveness, measured by all five health outcome measures, remained very similar to the basic results regardless of the imputation methods: during the first seven months the symptoms declined rapidly, but after that there were only small changes in the mean scores and no statistically significant differences between the two therapy groups at any measurement point. This stability of results is explained by the fact that the proportion of missing observations was reasonably small for all effectiveness measures.
With the economic outcome measures, the sensitivity analyses changed the results of the basic analysis more, but, again, the fundamental result remained the same: both direct and indirect costs due to mental disorders were greater in the group having received SPP. The sensitivity analyses changed the basic results mainly in the respect that the aggregate level of costs changed but the relationship between the two groups did not. This observation applies also to the costs arising from non-mental disorders. Independent of unit costs used or imputation method applied the differences in direct and indirect costs due to non-mental disorders were small between the two groups.
4. Discussion
Our study showed that symptoms of depression and anxiety were reduced substantially and by about the same amount in both therapy groups. The results thus confirm earlier findings indicating that both SPP and SFT are effective therapeutic approaches in the treatment of mental disorders [4] [31] . Differences in the direct health care costs due to mental disorders also were relatively small and not statistically significant either. As differences in the effectiveness means were very small the ICERs were extremely unstable and therefore no point estimates or confidence intervals for this ratio were estimated. Cost-effectiveness analysis in combination with the bootstrap method could, however, be used to handle the uncertainty associated with our results. The 500 bootstrap cost-effectiveness iterations made for each of the five health outcome measures supported the finding that SPP and SFT are quite similar with regard to their cost-effectiveness as the iteration points are situated quite evenly around the origin.
During the three-year follow-up period the mean total direct health care costs due to mental disorders were only marginally higher in the SPP group than in the SFT group. This difference was, however, not statistically significant, because the costs of individual patients varied considerably in both therapy groups. This difference in the total costs was due to fact that patients in the SPP group used auxiliary mental health care services more or at least as much as patients in the SFT group. Among the different cost items the greatest differences were, however, observed in the costs of study therapy, which were 482 euros (37%) higher in the SFT group, and this difference was also statistically significant. The reason for the observed difference in the cost of therapy sessions was that the price of one SFT visit was fixed at 188 euros (at 2010 prices) whereas the average price of one SPP visit was 71 euros. The higher price of an SFT visit was explained by the fact that the durations of SFT sessions were longer (1 - 1.5 hours vs. 45 minutes) and SFT therapists could consult with other SFT therapists if they considered it necessary. Both SPP and SFT therapists worked in the private sector, and so the price of a visit can be used as a proxy for the cost of one visit. Thus, although the realized number of study therapy visits by patients in the SPP group was, as planned in the protocol, nearly twice as high (18.0 vs. 9.4) as the number of visits by patients in the SFT group, the therapy costs were still clearly smaller in the SPP group.
An important finding in our study was that in the three-year follow-up period a great majority of patients in both therapy groups needed other treatments besides SPP or SFT for their symptoms. Studies with relatively short follow-up periods, too, have indicated that many patients need other treatments in addition to brief therapy [5] [32] . This study, with a follow-up period of three years, highlights very clearly that the need for additional treatments may be substantial especially in the long run, for the costs of all auxiliary treatments were observed to be much higher than the costs of SPP or SFT. Most of the cost of auxiliary treatments in both groups was due to the costs arising from the use of other psychotherapies received after the end of SPP or SFT. This indicates that in the long run short-term psychotherapies are quite seldom sufficient treatments for persons suffering from mood or anxiety disorders.
The total indirect costs due to mental disorders were in the SPP group as much as 4128 euros (65%) higher than the indirect costs of the SFT group. This great difference was due to the fact that the value of productivity lost and the value of informal help received because of mental disorders were much greater in the SPP group. Indirect costs were in both therapy groups clearly higher than direct costs. The mean indirect costs were, however, even more than the direct costs affected by the very high costs accrued by some individual patients. In the SPP group there were three patients with extremely high indirect costs which were due to productivity loss and informal help. If these patients had been excluded from the analysis, the mean indirect costs of the two therapy groups would have been quite similar.
The mean annual direct costs due to non-mental disorders during the three-year follow-up period were estimated to be 613 euros in the SPP group and 523 euros in the SFT group. This is much less than the corresponding average amount in the general Finnish population of same age (approximately 1100 euros in 2006) [33] . Although one must be very careful when comparing figures from different types of data (as was the case here), the differences in the above figures are so great that our finding does not seem to support the frequently expressed view that persons with depressive or anxiety disorders also have many other health problems and that their health care costs due to non-mental disorders are higher than those of persons without such disorders [34] . Possible explanations for our low estimates may be that the patients had relatively high educational attainment and that patients with severe organic diseases were excluded from our study. One further explanation could be that the reference figures [33] were partly based on registers where a certain share of mental health care expenditures, for instance, might be reported as somatic health care expenditures.
There are certain methodological considerations about our study that need to be addressed as well. First, compared to most clinical psychotherapy studies the sample size of our study (n = 198) can be regarded as relatively large, as sample sizes below 100 are very common [4] [31] . Second, in our study psychiatric symptoms were assessed using five different psychiatric measures which all yielded very similar results. This consistency of results together with the frequently repeated measurements increases the reliability of our results.
Third, the follow-up period of our study, three years, is considerably longer than what is usually the case with psychotherapy studies because in most studies the follow-up period is one year or less. Especially with mental health problems, which are often long-lasting and where relapses are frequent, a one-year follow-up period may be too short to capture the health or economic effects of the treatments compared.
In this study we tried to collect cost information about all the medication used in the treatment of mood and anxiety disorders. Some of the estimates on the direct costs of SPP and SFT can be regarded as highly reliable because part of the cost data was obtained directly from registers containing patient-level information about every patient. Part of the cost data was, however, based on information received from patients and with these cost items there is some uncertainty because of missing observations. In the sensitivity analyses different methods of handling missing observations were used and regardless of the way the missing observations were handled our results remained rather robust.
The missing observations were, however, a bigger problem in the case of indirect costs, as the estimation of indirect costs depended completely on information given by the patients. An additional weakness related to the estimation of indirect costs was that the estimation was partly based on questions to which it may have been difficult to give exact answers (e.g., for how long the respondent has been unable to study due to mental disorders or how much informal help the respondent has received). Also, considerable uncertainty attaches to the methods of valuing different indirect cost items, and there is no unanimity about how the valuation ought to be carried out. Regardless of these problems, the estimation of indirect costs is, however, considered to augment our understanding of the costs related to the treatment of depressive and anxiety disorders, especially because relatively few cost-effectiveness studies in the field of mental health have attempted to estimate indirect cost [35] .
To our knowledge, this is the first economic long-term evaluation study comparing the costs and effects of SPP and SFT. According to our results, symptoms of depression and anxiety were reduced to a very similar extent in both therapy groups and there were no significant differences in costs between the two groups. Thus our results suggest that these two therapies are comparable in terms of cost-effectiveness, and this observation was confirmed by bootstrap iterations. More research with extensive data both about the effects and costs of the therapies compared, a sufficiently long follow-up period and rigorous economic evaluation are needed before any definite conclusions about the cost-effectiveness of these therapies, or short-term therapies in general, can be made.
Finding out the most cost-effective treatments for mood and anxiety disorders can be regarded as exceptionally important for the prevalence of these disorders is high, they cause considerable human suffering and lead to remarkable disability resulting in notable indirect costs, and there are various treatment options with probably very different health and cost effects. Thus the benefits to be gained by identifying the most cost-effective treatments for these disorders may be substantial and clearly surpass those obtainable with most other disorders.
Acknowledgements
The Helsinki Psychotherapy Study Group [7] was responsible for collection of the data. Financial support for the study received from: The Academy of Finland (Grant No. 138876) and the Social Insurance Institution of Finland.
References
- Cuijpers, P., van Straten, A., Andersson, G. and van Oppen, P. (2008) Psychotherapy for Depression in Adults: A Meta-Analysis of Comparative Outcome Studies. Journal of Consulting and Clinical Psychology, 76, 909-922. http://dx.doi.org/10.1037/a0013075
- Cape, J., Whittington, C., Buszewicz, M., Wallace, P. and Underwood, L. (2010) Brief Psychological Therapies for Anxiety and Depression in Primary Care: Meta-Analysis and Meta-Regression. BMC Medicine, 8, 38. http://dx.doi.org/10.1186/1741-7015-8-38
-
Knekt, P., Lindfors, O., Renlund, C., Sares-Jaske, L., Laaksonen, M.A. and Virtala,
E. (2011) Use of Auxiliary Psychiatric Treatment during a 5-Year Follow-Up among
Patients Receiving Shortor Long-Term Psychotherapy. Journal of Affective Disorders,
135, 221-230.
http://dx.doi.org/10.1016/j.jad.2011.07.024 - Abbass, A.A., Hancock, J.T., Henderson, J. and Kisely, S.R. (2006) Short-Term Psychodynamic Psychotherapies for Common Mental Disorders. Cochrane Database of Systematic Reviews, Issue 4.
- Bosmans, J., Schreuders, B., van Marwijk, H., Smit, J., van Oppen,
P. and van Tulder, M. (2012) Cost-Effectiveness of Problem-Solving Treatment in
Comparison with Usual Care for Primary Care Patients with Mental Health Problems:
ARandomized Trial. BMC Family Practice, 13, 98.
http://dx.doi.org/10.1186/1471-2296-13-98 - Knekt, P., Lindfors, O., Harkanen, T., Valikoski, M., Virtala, E., Laaksonen, M.A., Marttunen, M., Kaipainen, M., Renlund, C. and the Helsinki Psychotherapy Study Group (2008) Randomized Trial on the Effectiveness of Longand Short-Term Psychodynamic Psychotherapy and Solution-Focused Therapy on Psychiatric Symptoms during a 3-Year Follow-Up. Psychological Medicine, 38, 689-703. http://dx.doi.org/10.1017/S003329170700164X
- Knekt, P. and Lindfors, O. (2004) A Randomized Trial of the Effect of Four Forms of Psychotherapy on Depressive and Anxiety Disorders: Design, Methods, and Results on the Effectiveness of Short-Term Psychodynamic Psychotherapy and Solution-Focused Therapy during a One-Year Follow-Up. Social Insurance Institution, Helsinki, 15-112. http://www.ktl.fi/tto/hps/pdf/effectiveness.pdf.
- Maljanen, T., Paltta, P., Harkanen, T., Virtala, E., Lindfors, O., Laaksonen, M.A., Knekt, P. and the Helsinki Psychotherapy Study Group (2012) The Cost-Effectiveness of Short-Term Psychodynamic Psychotherapy and Solution-Focused Therapy in the Treatment of Depressive and Anxiety Disorders during a One-Year Follow-Up. Journal of Mental Health Policy and Economics, 15, 13-23.
- American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. American Psychiatric Association, Washington DC.
- Malan, D.H. (1976) The Frontier of Brief Psychotherapy: An Example of the Convergence of Research and Clinical Practice. Plenum Medical Books, New York. http://dx.doi.org/10.1007/978-1-4684-2220-7
- Sifneos, P.E. (1978) Short-Term Anxiety Provoking Psychotherapy. In: Davanloo, H., Ed., Short-Term Dynamic Psychotherapy, Spectrum, New York, 35-42.
- Johnson, L.D.
and Miller, S.D. (1994) Modification of Depression Risk Factors: A Solution-Focused
Approach. Psychotherapy: Theory, Research, Practice, Training, 31, 244-253.
http://dx.doi.org/10.1037/h0090220 -
deShazer, S., Berg, I.K., Lipchik, E., Nunnally, E., Molnar, A., Gingerich, W. and
Weiner-Davies, M. (1986) Brief Therapy: Focused Solution Development. Family Process,
25, 207-221.
http://dx.doi.org/10.1111/j.1545-5300.1986.00207.x -
Beck, A.T., Ward, C.H., Mendelson, M., Mock, J. and Erbaugh, J. (1961) An Inventory
for Measuring Depression. Archives of General Psychiatry, 4, 561-571.
http://dx.doi.org/10.1001/archpsyc.1961.01710120031004 - Hamilton, M. (1960) A Rating Scale for Depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56-61. http://dx.doi.org/10.1136/jnnp.23.1.56
- Derogatis, L.R., Lipman, R.S. and Covi, L. (1973) SCL-90: An Outpatient Psychiatric Rating Scale—Preliminary Report. Psychopharmacology Bulletin, 9, 13-28.
- Hamilton, M. (1959) The Assessment of Anxiety States by Rating. British Journal of Medical Psychology, 32, 50-55. http://dx.doi.org/10.1111/j.2044-8341.1959.tb00467.x
- Laaksonen, M.A., Lindfors, O., Knekt, P. and Aalberg, V. (2012) Suitability for Psychotherapy Scale (SPS) and Its Reliability, Validity and Prediction. British Journal of Clinical Psychology, 51, 351-375. http://dx.doi.org/10.1111/j.2044-8260.2012.02033.x
- Harkanen, T., Knekt, P., Virtala, E. and Lindfors, O. (2005) A Case Study in Comparing Therapies Involving Informative Drop-Out, Non-Ignorable Non-Compliance and Repeated Measurements. Statistics in Medicine, 24, 3773-3787. http://dx.doi.org/10.1002/sim.2409
- Rubin, D.B. (1987) Multiple Imputation for Nonresponse in Surveys. John Wiley, New York. http://dx.doi.org/10.1002/9780470316696
- Schafer, J.L. (1999) Multiple Imputation: A Primer. Statistical Methods in Medical Research, 8, 3-15. http://dx.doi.org/10.1191/096228099671525676
- Lee, J. (1981) Covariance Adjustment of Rates Based on the Multiple Logistic Regression Model. Journal of Chronic Diseases, 34, 415-426.http://dx.doi.org/10.1016/0021-9681(81)90040-0
- Graubard, B.I. and Korn, E.L. (1999) Predictive Margins with Survey Data. Biometrics, 55, 652-659. http://dx.doi.org/10.1111/j.0006-341X.1999.00652.x
-
Efron, B. (1982) TheJackknife, the Bootstrap and Other Resampling Plans. CBMS-NSF
Regional Conference Series in Applied Mathematics, Monograph 38, SIAM.
http://dx.doi.org/10.1137/1.9781611970319 - Drummond, M., Sculpher, M., Torrance, G., O’Brien, B. and Stoddart, G.L. (2005) Methods for the Economic Evaluation of Health Care Programmes. 3rd Edition, Oxford University Press, Oxford.
- Pruessner, J., Kirschbaum, C., Meinlschmid, G. and
Hellhammer, D. (2003) Two Formulas for Computation of the Area under the Curve Represent
Measures of Total Hormone Concentration versus Time-Dependent Change. Psychoneuroendocrinology,
28, 916-931.
http://dx.doi.org/10.1016/S0306-4530(02)00108-7 - Briggs, A.H. (2001) Handling Uncertainty in Economic Evaluation and Presenting the Results. In: Drummond, M. and McGuire, A., Eds., Economic Evaluation in Health Care. Merging Theory with Practice, Oxford University Press, Oxford, 172-214.
- Manning, W.G., Fryback, D.G. and Weinstein, M.C. (1996) Reflecting Uncertainty in Cost-Effectiveness Analysis. In: Gold, M.R., Siegel, J.E., Russell, L.B. and Weinstein, M.C., Eds., Cost-Effectiveness in Health and Medicine, Oxford University Press, Oxford, 247-275.
- Armitage, P. (2001) Theory and Practice in Medical Statistics. Statistics in Medicine, 20, 2537-2548. http://dx.doi.org/10.1002/sim.727
- SAS Institute Inc. (2008) SAS/STAT® 9.2 User’s Guide. SAS Institute Inc., Cary.
- Gingerich, W.J. and Eisengart, S. (2000) Solution-Focused Brief Therapy: A Review of the Outcome Research. Family Process, 39, 477-498. http://dx.doi.org/10.1111/j.1545-5300.2000.39408.x
-
Guthrie, E., Moorey, J., Margison, F., Barker, H., Palmer, S., McGrath, G., Tomenson,
B. and Creed, F. (1999) CostEffectiveness of Brief Psychodynamic-Interpersonal Therapy
in High Utilizers of Psychiatric Services. Archives of General Psychiatry, 56, 519-526.
http://dx.doi.org/10.1001/archpsyc.56.6.519 - Hujanen, T., Peltola, M., Hakkinen, U. and Pekurinen, M. (2008) Men’s and Women’s Health Care Expenditures by Age Groups in 2006 [in Finnish]. Stakesintyopapereita 37/2008, Stakes, Helsinki.
- Simon, G., Ormel, J., VonKorff, M. and Barlow, W. (1995) Health Care Costs Associated with Depressive and Anxiety Disorders in Primary Care. American Journal of Psychiatry, 152, 352-357.
- Konnopka, A., Leichsenring, F., Leibing, E. and Konig, H. (2009) Cost-of-Illness Studies and Cost-Effectiveness Analyses in Anxiety Disorders: A Systematic Review. Journal of Affective Disorders, 114, 14-31. http://dx.doi.org/10.1016/j.jad.2008.07.014


