Journal of Cancer Therapy
Vol. 4 No. 3 (2013) , Article ID: 31496 , 3 pages DOI:10.4236/jct.2013.43084
Combination Therapy of Multiple Micro Trauma Technology on Hepatocellular Carcinoma
Xinfeng Li1*, Guorong Lu2, Dexin Liu3, Gaoxiong Wang1, Shilin Li2, Wei Zhuang1
![]()
1Department of Hepatobiliary Surgery, Second Affiliated Hospital of Fujian Medical University, Quanzhou, China;
2Department of Ultrasound, Second Affiliated Hospital of Fujian Medical University, Quanzhou, China;
3Department of Radiology, Second Affiliated Hospital of Fujian Medical University, Quanzhou, China.
Email: *Surgone-0107@163.com
Copyright © 2013 Xinfeng Li et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received January 7th, 2013; revised February 10th, 2013; accepted February 18th, 2013
Keywords: Hepatocellular Carcinoma; Radiofrequency Ablation; Hepatic Artery; Chemoembolization
ABSTRACT
Objective: To compare efficacy of therapy scheme as Transhepatic Artery Chemoembolization (TACE) + Radiofrequency Ablation (RFA) + Introportal Vein Chemotherapy (PVC) + Percutaneous Ethanol Injection (PEI) therapy (quadruplet group) with TACE + RFA combinational therapy (diad group) in treating hepatocellular carcinoma (HCC). Methods: 25 cases in quadruplet group were treated by TACE for 3 weeks, then by RFA, after 2 months, by PVC + PEI; 23 cases in diad group were treated by TACE for 3 weeks and then by PEI. After completion of each treatment course in both groups, Alphafetoprotein (AFP) was tested 2 months later; abdomen colorful doppler, CT and AFP were retested 6 months later. Results: AFP was significantly decreased in 23 cases of quadruplet group and 20 cases of diad group among those with AFP positive results. 6 months later, examinations of CT, colorful Doppler and AFP in two groups showed: quadruplet group has significantly decreased (X2 = 6.81, P < 0.01) blood supply of cancer tissue and significantly diminished (X2 = 8.29, P < 0.01) tumor size, few cases with AFP elevation (X2 = 5.06, P < 0.05); lower 1 year relapse rate and two years mortality than that in diad group (X2 = 5.30, P < 0.05). Conclusion: TACE + RFA + PVC + PEI combinational therapy is a safe double intervention treatment for HCC scheme with less side effects, which is better than TACE + PEI scheme in killing remnant tumor and reducing relapse.
1. Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer in the world, and the third most common cause of cancer-related death [1]. Surgery gives the best chance of cure with complete extirpation of the tumour. However, this potentially curable method is possible only in a small proportion of patients, for the remaining, palliative treatment is indicated, which includes radiofrequency ablation (RFA), transcatheter arterial chemoembolization (TACE), immunotherapy, radiotherapy or molecular targeted therapy [2]. Due to the unique biological activity of hepatocellular carcinoma, despite all the treatment options when used as monotherapy, patients with HCC have a poor long term prognosis. In this setting, multimodal and combination therapies have emerged as alternative treatment modalities for HCC. TACE + PEI combinational therapy has achieved certain effect in improving quality of life and prolonging life span, however, the incomplete treatment is still the most important cause for relapse. From Oct 2005 to Aug 2010, the author has chosen TACE + RFA + PVC + PEIT combinational method to treat 25 HCC patients and compared its efficacy with TACE + PEI method in 23 HCC patients. The purpose of our study is therefore to assess the technical feasibility and local efficacy of TACE + RFA + PVC + PEI combinational therapy for HCC scheme with less side effects, which is better than TACE + PEI scheme in killing remnant tumor and reducing relapse.
2. Materials and Methods
2.1. Material
48 cases with HCC (35 males, 13 females), within the age range from 27 to 65 years old, with the mean age at 38.1 years; Cases in both groups were confirmed by pathology diagnosis with Doppler guided puncture; tumor size was between 4.0 cm × 3.8 cm × 3.5 cm and 10.1 cm × 9.1 cm × 8.7 cm; 40 cases with single nodes, 8 cases with 2 - 3 nodes, AFP positive in 23 cases in quadruplet group and 20 cases in diad group. Our prospective study was approved by our institutional review board and informed consent was obtained from all participating patients.
2.2. Methods
48 cases were allocated into two groups with 25 cases in TACE + RFA + PVC + PEI quadruplet group. After 3 weeks TACE treatment, RF-3000 radiofrequency treatment system (US Dalong Company) with electrode diameter 4.0 cm was used to design treatment plan according to the tumor size. In general, treatment was conducted from the deep tissue to the superficial tissue; treatment was given once more for each withdraw at 1.5 cm with no more than 15 times. Tumor was covered by microbubble under Doppler at the end of treatment. 2 months later, PMC plan (Fluorouracil 1000 mg, Mitomycin 8 mg and Carboplatin 300 mg) was conducted by PVC and PEI was conducted in the area with insufficient RFA treatment, which was separated to 3 to 5 points and the total volume less than 15 ml, with 3 - 5 ml each point. PEI was conducted in 23 cases of TACE+ PEI diad group following 3-week TACE treatment. The treatment area was separated to 3 to 5 points with 3 - 5 ml each point and total volume as 15 ml. The treatment was done for 5 times, once a week. Afterwards, there was a return visit for every 2 months. AFP retest was performed respectively at 2 months and 6 months after completion of each treatment course in 48 cases. CT and abdomen color Doppler were conducted 6 months later. Those relapsed cases (refers to AFP positive index elevation, enlarged tumor size, new lesion found and positive aspiration biopsy) were performed PEI for the second time with the same method and dose.
2.3. Statistical Analysis
Chi Square Test was used with P < 0.05 as of statistical significance
3. Results
3.1. Follow up
Patients in both groups were followed up for 2 years. AFP decreased in 23 cases of quadruplet group and 20 cases of diad group after corresponding treatment among those cases with AFP positive result. After 6-month treatment, AFP was elevated again in 6 cases of quadruplet group (26%) and in 12 cases of diad group (60%) (X2 = 5.055, P < 0.05). One year relapse rate was 32% (8 cases) in quadruplet group and 65.22% (15 cases) in diad group (X2 = 5.30, P < 0.05); two years mortality was 20% (5 cases) in quadruplet group and 47.8% (11 cases) in diad group.
Comparison of examination results of abdomen color Doppler and CT of two groups were showed in Table 1.
3.2. Complication
Fever and transient abdominalgia were common; 1 case with hemobilia in diad group, 2 cases in quadruplet group and 3 cases in diad group had arrest of bone marrow and recovered after treatment. There was no severe complication.
4. Discussion
Currently, most scholars still consider that surgical removal is the best choice for resectable HCC, nonresectable HCC can be treated by complex treatment. PFA is characterized by micro trauma, reliable local tumor killing and easy repeated application with better efficacy of multiple points puncture ablation [3-6]. Hence, TACE + RFA became an effective combinational therapy for HCC treatment [4-7]. The mechanism is based on that tumor cells have lower tolerance to heat than that of normal cells. The division of tumor cells stops at temperature up to 40˚C; tumor cells are killed or DNA is damaged at temperature with 41˚C - 42˚C. RFA technology works by producing middle and high radio frequency (460 kHz) through concentrated beam polar, provoking tissue and cell to undergo ions vibration with collision of ions producing heat up to 80˚C - 100˚C. This leads to coagulability necrosis of cancer tissue, clotting of vascular tissue around tumor to form response band, and prevention of metastasis of tumor and blood supply. The heat response of radio frequency can strengthen immunity of body [8] as well. Choi reported that the 3-yearsurvival-rate after multiple RFA treatment was 54% and vascular reconnection or allochthonic vascular formation may occur 1 month later after TACE treatment [9]. Therefore, RFA treatment should be conducted within 1 month. Combinational of these two methods is complementary to each other [7]. Treatment is not thoroughly complete in most cases due to that RFA under per cutem ultrasound guidance is affected by Doppler blind area, cancer embolus of portal vein branches and tumor location etc. (e.g. rumor near main vascular, gall bladder,
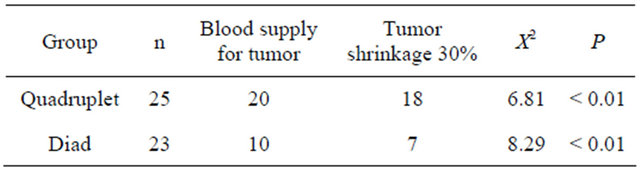
Table 1. Comparison of examination results of color Doppler and CT in two groups.
stomach and colon etc.). Li considered that portal vein blood supply was essential for the HCC growth and relapse after treatment [10]. It has been reported that HCC specimen of tumor node after vascular infusion demonstrated that, blood supply of 1/3 of cancer embolus was by liver hepatic artery, 1/2 was by portal vein, and others were by double blood supply [11]. Due to the slow blood flow speed of portal vein, only half of TACE dosing in chemotherapy is needed to reach topical high concentration to gain better tropical effect with less damage to the whole liver. Therefore, PEI conducted in areas (especially near cavum viscera) of insufficient treatment effect facilitate further killing remnant tumor. Of 48 cases treated by different combinational plans in this study, AFP decreased significantly 2 month later; color doppler and CT examination showed significant lower blood flow in tumor and obvious smaller tumor size in quadrilet group in comparison with that in diad group (P < 0.01) 6 months later; and elevation of AFP was higher in diad group than that in quadrilet group (P < 0.05); there are more remnant cancer tissue in diad group than in quadrilet group probably due to the influence of the tumor position (ultrasound blind area, near cavum viscera, near main vascular, absolute ethanol using volume and patient different pain extent sensed by patient); and one year relapse rate was higher in diad group than that in quadrilet group (P < 0.05). It demonstrates that septum exists in tumor growth and absolute ethanol can not resolve septums, which blocking diffusion of absolute ethanol. However, thermocoagulation of RFA can destroy tumor septums with superior cancer tissue damage than that by PEI. In addition, PVC + PEI can complement insufficiency of treatment, so multiple interventional therapies can further kill remnant cancer tissue. The 2-year-survival-rate of quadrilet group can reach 80%, higher than the 52.2% of diad group.
The author considers that TACE + RFA + PVC + PEI combinational therapy is a safe, reliable multi-interventional treatment plan with less side-effect. It has better effect in killing remnant cancer tissue and reducing relapse than TACE + PEIT plan.
5. Acknowledgements
This work was supported by Fujian Provincial Scientific Bureau Fund (JA03085).
REFERENCES
- J. Bruix and J. M. Llovet, “Prognostic Prediction and Treatment Strategy in Hepatocellular Carcinoma,” Hepatology, Vol. 35, No. 3, 2002, pp. 519-524. doi:10.1053/jhep.2002.32089
- G. Cabibbo, F. Latteri, M. Antonucci and A. Craxi, “Multimodal Approaches to the Treatment of Hepatocellular Carcinoma,” Nature Clinical Practice: Gastroenterology & Hepatology, Vol. 6, No. 3, 2009, pp. 159-169. doi:10.1038/ncpgasthep1357
- H. X. Xu, X. Y. Xie, M. D. Lu, et al., “Ultrasound-Guided Percutaneous Thermal Ablation for Treatment of Hepatocellular Carcinoma,” Chinese Journal of Hepatobiliary Surgery, Vol. 11, No. 12, 2005, pp. 809-811.
- H. X. Xu, X. Y. Xie, M. D. Lu, et al., “Ultrasound-Guided percutaneous Thermal Ablation of Hepatocellular Carcinoma Using Microwave and Radiofrequency Ablation,” Clinical Radiology, Vol. 59, No. 1, 2004, pp. 52-60. doi:10.1016/j.crad.2003.09.006
- X. L. Du, J. S. Wu, Q. S. Ma, et al., “Transcatheter Hepatic Artery Combolization Helps Radiofrequency Ablation of Hepatic Neoplasms,” Journal of the Fourth Military Medical University, Vol. 21, No. 11, 2000, pp. 1406- 1408.
- J.-Y. Wu, W. Yang, M. Cui, et al., “Efficacy and Feasibility of Radiofrequency Ablation for Decompensated Cirrhotic Patients with Hepatocellular Carcinoma,” Chinese Medical Journal, Vol. 123, No. 15, 2010, pp. 1967- 1972.
- X. F. Li, G. R. Lu, G. X. Wang, D. X. Lu and S. L. Li, “TACE in Combination with RF in Treatment of Advanced HCC,” Chinese Journal of Hepatobiliary Surgery, Vol. 9, 2003, pp. 23-25.
- X. Y. Yin, M. D. Lu, X. Y. Xie, et al., “Use of Percutaneous Thermal Ablation for Treatment of Reoperable Recurrent Hepatocellular Carcinoma after Liver Resection,” Chinese Journal of Hepatobiliary Surgery, Vol. 12, No. 4, 2006, pp. 243-245.
- D. Chio, H. K. Lim, M. J. Kim, et al., “Recurrent Hepatocellular Carcinoma: Percutanous Radiofrequency Ablation after Hepatectomy,” Radiology, Vol. 230, 2004, pp. 135-141. doi:10.1148/radiol.2301021182
- M. R. Li, G. D. Ye, H. D. Chen, et al., “Combined Superselective Transcatheter Arterial Chemoembolization and Selective Intraportal Venous Embolization for the Treatment of Inoperable Advanced Primary Liver Cancer,” Chinese Journal of General Surgery, Vol. 19, No. 1, 2004, pp. 12-14.
- H. Taniguchi, T. Daidoh and Y. Shioaki, “Blood Supply and Drug Delivery to Primary and Secondary Human Liver Cancers Studied with in Vivo Bromodeoixyuridine Labeling,” Cancer, Vol. 71, No. 1, 1993, pp. 50-55. doi:10.1002/1097-0142(19930101)71:1<50::AID-CNCR2820710109>3.0.CO;2-T
NOTES
*Corresponding author.

