Health
Vol.5 No.3A(2013), Article ID:29525,7 pages DOI:10.4236/health.2013.53A068
Schizophrenia knowledge and attitudes toward help-seeking among Japanese fathers and mothers of high school students
![]()
1School of Health Sciences, Faculty of Medicine, Tohoku University, Miyagi, Japan; *Corresponding Author: hatsumi@med.tohoku.ac.jp
2Department of Psychiatry, Niigata University Graduate School of Medical and Dental Sciences, Niigata, Japan
3Division of Medical Education, Comprehensive Medical Education Center, School of Medicine, Faculty of Medicine, Niigata University, Niigata, Japan
4Department of Medical Informatics and Statistics, Niigata University Graduate School of Medicine, Niigata, Japan
Received 14 January 2013; revised 14 February 2013; accepted 26 February 2013
Keywords: Schizophrenia; Attitude; Help-Seeking; Fathers; Mothers
ABSTRACT
The prodromal symptoms of schizophrenia are nonspecific and include social withdrawal, sleeplessness, decreased desire, and loss of concentration. Schizophrenia outcomes might be improved if greater therapeutic effort was focused on people with prodromal symptoms. To hasten help-seeking for schizophrenia, we developed a schizophrenia education program for families of patients. Help-seeking and schizophrenia attitudes and knowledge were analyzed among Japanese parents (666 fathers and 613 mothers) of high school students by using the Social Distance Scale-Japanese version, the Link Devaluation-Discrimination Measure and our own questions on help-seeking and schizophrenia knowledge. Statistical analysis included cross-tabulation, the χ2 test, and multiple regression analysis. Most (97.5%) fathers were aged 40 - 59 years; most (78.3%) mothers were aged 40 - 49 years. There was a significant difference between fathers and mothers in basic knowledge of schizophrenia (P < 0.001); however, fathers and mothers did not significantly differ in their attitudes toward schizophrenia (P > 0.05). When asked what treatment they would seek for a child with sleeplessness or social withdrawal, fathers and mothers significantly differed in seeking help medical care at a department of psychosomatic medicine (P < 0.05) and in seeking help from the nurse at their child’s school (P < 0.001). Fathers and mothers also differed in relation to the decision not to seek help (P < 0.001). Multiple regression analysis revealed that basic knowledge significantly differed between fathers and mothers (P = 0.001). In an analysis of parental response to a child with sleepiness and social withdrawal, multiple regression analysis revealed that fathers and mothers significantly differed in the likelihood of seeking help at a department of psychosomatic medicine and from a school nurse and in the likelihood of not seeking help (P < 0.05, P = 0.001 and P = 0.001, respectively). In conclusion, helpseeking behavior differed between Japanese fathers and mothers. These findings should assist in developing schizophrenia education programs that aim to hasten intervention.
1. INTRODUCTION
Early intervention in schizophrenia is now a major focus in mental health care worldwide [1-3]. Duration of psychosis (DUP) is a critical variable, and the importance of intervention within 5 years of the onset of psychosis is now acknowledged [4]. Recent research indicates that longer DUP is directly associated with worsening of functional outcomes, symptoms, quality of life and response to antipsychotic medications [5]. Structural magnetic resonance imaging (MRI) studies showed abnormalities in hippocampus, temporal lobe and prefrontal cortex, as well as gray matter changes that are associated with clinical deterioration, including functional and cognitive declines and increased symptom severity [5]. Studies of treatment delays tend to focus on individual or illness-related factors and family or socio-demographic factors [6]. Some but not all studies found that denial of illness and lack of insight account for long DUP [6].
Most studies show that social withdrawal from friends and family leads to longer delays and that fear of being stigmatized may make people reluctant to seek help [6].
The signs of schizophrenia may be not be easy to recognize, particularly because the prodromal symptoms are nonspecific. However, many schizophrenia patients do have a prodromal phase, which may begin as early as age 10 years. Psychotic disorders such as schizophrenia typically begin with a prodromal period that precedes the onset of full-blown psychotic symptoms [7]. These prodromal symptoms are nonspecific and include social withdrawal, sleeplessness, decreased desire, and loss of concentration [5,8]. Intervention during the onset phase may prevent or delay the transition to psychosis and assist in treating current problems such as co-morbid depressive and anxiety symptoms or syndromes [7].
In recent years, efforts have focused on early intervention, even as early as the prodromal phase preceding schizophrenia onset [8]. Proponents of early intervention argue that outcomes can be improved if more therapeutic effort is focused on the early stages of schizophrenia or on people with prodromal symptoms [9]. The challenge is to identify the minority of patients with prodromal criteria who are likely to progress to a first episode of schizophrenia, because such patients often respond well to antipsychotics and might benefit from early intervention [10]. In addition, research indicates that psychological interventions for prodrome can improve functioning and symptomatology [5]. A major challenge has been to prospectively identify prodrome, particularly given the nonspecific nature of such symptoms [7]. Researchers in prodromal psychosis forcefully argued for the inclusion of a “risk syndrome of psychosis” as a diagnostic category in DSM V [11], as this phase is a potential target for intervention.
Identifying prodromal symptoms will require family cooperation. However, awareness of prodromal symptoms, and help-seeking and attitudes toward schizophrenia, may differ between fathers and mothers. Studies showed that males were significantly more likely than females to have a longer DUP [1]. If this finding is indeed the case, it may be necessary to develop different education programs for fathers and mothers. However, the manner in which fathers and mothers differ with respect to their knowledge and attitudes toward schizophrenia has not been recently studied. In this study, we attempt to identify such differences between fathers and mothers.
We previously developed a schizophrenia education program that attempts to hasten intervention for the disorder. In a previous study, we did not separately evaluate the effects of this education program in fathers and mothers [12]. Thus, this study has two aims: to investigate prospective cohort study about prodromal symptoms of schizophrenia and to identify differences between Japanese fathers and mothers of high school students.
2. PARTICIPANTS AND METHODS
2.1. Participants
The participants were Japanese parents (666 fathers and 613 mothers) of high school students and were extracted from among 1,370,000 candidates in a database administered by a private Japanese company specializing in questionnaire research. Stratified random sampling was used, as previously described [12-14]. The study was approved by the Ethics Committee of the Niigata University School of Medicine.
2.2. Measurement
The participants answered questions on sociodemographic characteristics. Attitude toward schizophrenia was evaluated by using the Social Distance Scale-Japanese version (SDS-J) [15] and the Link Devaluation-Discrimination Measure [13], individual stigma was evaluated by the Social Distance Scale-Japanese version (SDS-J) [15] and social stigma was evaluated by the Link Devaluation-Discrimination Measure [13]. A detailed explanation of this questionnaire is available elsewhere [13,15].
Fathers and mothers were asked about what help they would seek if they had a child with sleeplessness and social withdrawal, which are nonspecific symptoms of schizophrenia, and about the type of medical facility at which they would seek a consultation.
Finally, we asked about basic knowledge of schizophrenia and discrimination of prodromal symptoms using items that we developed for that purpose. A detailed explanation of this questionnaire was previously published [12].
2.3. Statistical Analysis
All analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 18.0. The unpaired t-test was used to compare the distributions of scores between fathers and mothers on the SDS-J and Link Devaluation-Discrimination Measure, and on questions regarding basic knowledge of schizophrenia and discrimination of prodromal symptoms. Crosstabulation and the χ2 test were used to compare help-seeking between fathers and mothers. Multiple regression analysis was used to examine the relative importance of different survey variables for fathers and mothers.
3. RESULTS
3.1. Participant Characteristics
Most (97.5%) fathers were aged 40 - 59 years; most (78.3%) mothers were aged 40 - 49 years. More than half (59.3%) of fathers had a university education, and 40.9% of mothers had attended vocational school or junior college. The most common occupation was transportation and communication (34.4%) among fathers and agriculture, forestry and fisheries (42.4%) among mothers.
3.2. Knowledge of Schizophrenia, Discrimination of Prodromal Symptoms, Link Devaluation-Discrimination Measure and Distribution of Scores on SDS-J
Fathers and mothers significantly differed in their basic knowledge of schizophrenia (P < 0.001; Table 1) but not in their ability to discriminate prodromal symptoms (P > 0.05). In addition, there were no significant differences in scores for attitudes toward schizophrenia (Link Devaluation-Discrimination Measure and distribution of scores on SDS-J) (P > 0.05).
3.3. Help-Seeking in Fathers and Mothers: Sleeplessness
Fathers and mothers who were asked what treatment they would seek for a sleepless child significantly differed with respect to the decision to seek medical treatment in a department of psychosomatic medicine or a psychiatric clinic (P < 0.05 for both; Table 2): fathers were less likely to seek help in a department of psychosomatic medicine, and mothers were less likely to seek help in a psychiatric clinic. Fathers and mothers also significantly differed with regard to seeking help from the nurse at their child’s school (P < 0.001): fathers were less likely to seek help from the school nurse. Fathers were also significantly more likely to seek no help (P < 0.001).
3.4. Help-Seeking in Fathers and Mothers: Social Withdrawal
Fathers and mothers who were asked what treatment they would seek for a child with social withdrawal significantly differed with respect to the decision to seek medical treatment in a department of psychosomatic medicine (P < 0.001; Table 2): fathers were less likely to seek such help. As compared with mothers, fathers were also less likely to seek help from the school nurse (P < 0.001) and more likely to seek no help (P < 0.001).
3.5. Multiple Regression Analysis with Fathers and Mothers as Dependent Variables
Multiple regression analysis revealed that basic knowledge of schizophrenia significantly differed between fathers and mothers (P = 0.001; Table 3). Regarding a child with sleeplessness, multiple regression analysis revealed that a decision to seek help at a psychiatric clinic, at a department of psychosomatic medicine and from the school nurse and a decision not to seek help significantly differed between fathers and mothers (P = 0.026, P = 0.045, P = 0.001 and P = 0.001, respectively). Regarding a child with social withdrawal, multiple regression analysis revealed that a decision to seek help at a department of psychosomatic medicine, from the school nurse and at school and a decision not to seek help significantly differed between fathers and mothers (P = 0.001, P = 0.001, P = 0.032 and P = 0.001, respectively).
4. DISCUSSION
The first episode of psychosis frequently occurs during adolescence and early adulthood and is associated with high levels of trauma, affective disturbance and suicide [16]. Current definitions of the prodromal (or at-risk mental state) phase of schizophrenia include attenuated and/or transient psychotic symptoms as well as a combination of different risk indicators and a recent substantial deterioration in global functioning [17]. Abnormalities in mood (e.g., anxiety, depression) and sleep disturbances are often accompanied by blunted or inappropriate emotional expressions [5]. In recent years
Table 1. Basic knowledge of schizophrenia, discrimination of prodromal symptoms, Link Devaluation-Discrimination Measure, and distribution of scores on Social Distance Scale-Japanese version (SDS-J) among fathers and mothers.
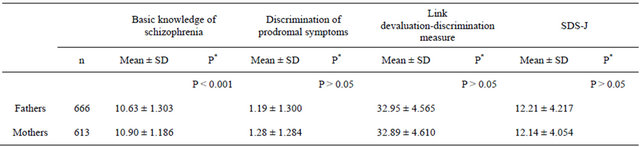
*t-test.
Table 2. Help-seeking among fathers and mothers for child sleeplessness and social withdrawal.

Cross-tabulation, χ2 test.
there has been some research on early intervention in psychosis, which was done during the prepsychotic period (prodrome) and/or after the onset of full blown psychotic episode [18]. Several research groups found that the prospectively identified prodromal period was associated with a high rate of conversion to schizophrenia or another psychotic disorder [5]. Accumulated data suggest that the rate of conversion to frank psychosis within two years is 25% to 40% of cases [17]. Prospective identification and subsequent treatment of patients could prevent development of full blown psychosis and might delay the onset or promote recovery from the disorder [18]. In a study by Bechdolf et al., integrated psychological intervention appeared effective in delaying psychosis onset during a 24-month time period among people in the early initial prodromal state [19]. Early intervention is expected to reduce illness severity in patients with schizophrenia and to contain health-care costs by reducing hospital admissions and improving social functioning of patients [4,6,20]. We think that it is important to involve parents in interventions during the prodromal phase. In Western countries, general practitioners are often the first point of contact for patients with prodromal schizophrenia [8]. However, general practitioners are not common in Japan. Thus, Japanese parents must make their own choices
Table 3. Results of multiple regression analysis of fathers and mothers as dependent variables.

β, standardized regression coefficient; t, t-value; R, multiple correlation coefficients. Multiple regression analysis.
regarding help-seeking. We hypothesized that there would be differences between fathers and mothers in such helpseeking and found that fathers were less likely than mothers to seek help (10% of fathers opted not to seek help). However, this result may be peculiar to Japanese parents.
Symptoms such as anxiety, depression and sleep disturbance are termed general psychopathology symptoms and often accompany clinical presentation of psychotic disorders [5]. A person presenting with sleep disturbance, depressed mood and even attenuated (sub threshold) psychotic symptoms may turn out to be a true positive, false positive or a false false positive [7]. Although some people with an apparent prodrome do indeed progress to a psychotic disorder (true positives), many do not [7]. There is concern that a high rate of false-positives (identification of an individual as prodromal who does not go on to develop psychosis) may result in individuals being stigmatized or undergoing unnecessary treatment [5]. Stigma raises barriers to access [21]. However, contrary to our expectations, attitudes toward schizophrenia among fathers and mothers did not significantly differ. In a word, neither social stigma nor individual stigma significantly differed between fathers and mothers.
Our study examined differences between fathers and mothers. However, such analysis is insufficient. In a Canadian study, Addington et al. found that the substantial barriers to getting help included not knowing the early signs of psychosis, concerns about being labeled mentally ill or psychotic and not knowing where to go for help [21]. They assessed public mental health literacy regarding psychosis and found that there was a high reported knowledge of the term schizophrenia (76%) and no difference between fathers and mothers [21]. Our study found no difference between fathers and mothers regarding discrimination of prodromal symptoms. However, basic knowledge of schizophrenia significantly differed between fathers and mothers: mothers had more basic knowledge of schizophrenia. These results may be important for improving education programs, which are necessary because they could prevent onset of full-blown disorder, or at least ameliorate or delay onset of such a condition.
5. ACKNOWLEDGEMENTS
The authors thank the study participants. This work was supported by a 2010 Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (22592581), entitled “Investigations of the Consciousness of Parents of Junior and Senior High School Students Concerning Schizophrenia and the Development of Educational Enlightenment Media”. None of the authors has any conflict of interest associated with this study.
REFERENCES
- Chang, W.C., Tang, J.Y., Hui, C.L., Lam, M.M., Wong, G.H., Chan, S.K., Chiu, C.P., Chung, D.W., Law, C.W., Tso, S., Chan, K., Hung, S. F. and Chen, E.Y. (2012) Duration of untreated psychosis: Relationship with baseline characteristics and three-year outcome in first-episode psychosis. Psychiatry Research, 198, 360-365. doi:10.1016/j.psychres.2011.09.006
- Shrivastava, A., Johnston, M., Terpstra, K., Stitt, L. and Shah, N. (2012) Atypical antipsychotics usage in longterm follow-up of first episode schizophrenia. Indian Journal of Psychiatry, 54, 248-252. doi:10.4103/0019-5545.102425
- Koike, S., Takano, Y., Iwashiro, N., Satomura, Y., Suga, M., Nagai, T., Natsubori, T., Tada, M., Nishimura, Y., Yamasaki, S., Takizawa, R., Yahata, N., Araki, T., Yamasue, H. and Kasai, K. (2012) A multimodal approach to investigate biomarkers for psychosis in a clinical setting: The integrative neuroimaging studies in schizophrenia targeting for early intervention and prevention (IN-STEP) project. Schizophrenia Research, 4.
- Yap, H.L. (2010) Early psychosis intervention. Singapore Medical Journal, 51, 689-693.
- Larson, M.K., Walker, E.F. and Compton, M.T. (2010) Early signs, diagnosis and therapeutics of the prodromal phase of schizophrenia and related psychotic disorders. Expert Review of Neurotherapeutics, 10, 1347-1359.
- O’Callaghan, E., Turner, N., Renwick, L., Jackson, D., Sutton, M., Foley, S.D., McWilliams, S., Behan, C., Fetherstone, A. and Kinsella, A. (2010) First episode psychosis and the trail to secondary care: Help-seeking and health-system delays. Social Psychiatry and Psychiatric Epidemiology, 45, 381-391. doi:10.1007/s00127-009-0081-x
- Yung, A.R. and Nelson, B. (2011) Young people at ultra high risk for psychosis: a research update. Early Intervention in Psychiatry, 1, 52-57. doi:10.1111/j.1751-7893.2010.00241.x
- Simon, A.E., Jegerlehner, S., Müller, T., Cattapan-Ludewig, K., Frey, P., Grossenbacher, M., Seifritz, E. and Umbricht, D. (2010) Prodromal schizophrenia in primary care: A rando mised sensitisation study. British Journal of General Practice, 60, 353-359.
- Marshall, M. and Rathbone, J. (2011) Early intervention for psychosis. Schizophrenia Bulletin, 37, 1111-1114. doi:10.1093/schbul/sbr110
- Weiser, M. (2011) Early intervention for schizophrenia: The risk-benefit ratio of antipsychotic treatment in the prodromal phase. American Journal of Psychiatry, 168, 761-763. doi:10.1176/appi.ajp.2011.11050765
- Shrivastava, A., McGorry, P.D., Tsuang, M., Woods, S.W., Cornblatt, B.A., Corcoran, C. and Carpenter, W. (2011) “At tenuated psychotic symptoms syndrome” as a risk syndrome of psychosis, diagnosis in DSM-V: The debate. Indian Journal of Psychiatry, 53, 57-65. doi:10.4103/0019-5545.75560
- Yoshii, H., Watanabe, Y., Kitamura, H., Chen, J. and Akazawa, K. (2011) Effect of an education program on improving knowledge of schizophrenia among parents of junior and senior high school students in Japan. BMC Public Health, 11, 323. doi:10.1186/1471-2458-11-323
- Yoshii, H., Watanabe, Y., Kitamura, H., Nan, Z. and Akazawa, K. (2011) Stigma toward schizophrenia among parents of junior and senior high school students in Japan. BMC Research Notes, 4, 558. doi:10.1186/1756-0500-4-558
- Yoshii, H., Watanabe, Y., Kitamura, H., Nan, Z. and Akazawa, K. (2012) Effect of an education program on improving help-seeking among parents of junior and senior high school students in Japan. Global Journal of Health Science, 4 , 33-41.
- Yoshii, H., Watanabe, Y., Kitamura, H., Ling, Y. and Akazawa, K. (2012) Social distance toward schizophrenia among parents of adolescents. Health, 4, 386-391. doi:10.4236/health.2012.47061
- Onwumere, J., Bebbington, P. and Kuipers, E. (2011) Family interventions in early psychosis: Specificity and effectiveness. Epidemiology and Psychiatric Sciences, 20, 113-119. doi:10.1017/S2045796011000187
- Keshavan, M.S., Delisi, L. E. and Seidman, L. J. (2011) Early and broadly defined psychosis risk mental states. Schizophrenia Research, 126, 1-10.
- Coentre, R., Levy, P. and Figueira, M.L. (2010) Early inter vention in psychosis: Prepsychotic period. Acta Mé- dica Portuguesa, 23, 1083-1090.
- Bechdolf, A., Wagner, M., Ruhrmann, S., Harrigan, S., Putzfeld, V., Pukrop, R., Brockhaus-Dumke, A., Berning, J., Janssen, B., Decker, P., Bottlender, R., Maurer, K., Moller, H.J., Gaebel, W., Hafner, H., Maier, W. and Klosterkotter, J. (2012) Preventing progression to first-episode psychosis in early initial prodromal states. British Journal of Psychiatry, 200, 22-29. doi:10.1192/bjp.bp.109.066357
- Cocchi, A., Mapelli, V., Meneghelli, A. and Preti, A. (2011) Cost-effectiveness of treating first-episode psychosis: Five-year follow up results from an Italian early intervene tion programme. Early Inter Psychiatry, 5, 203-211.
- Addington, D., Berzins, S. and Yeo, M. (2012) Psychosis literacy in a Canadian health region: Results from a general population sample. Canadian Journal of Psychiatry, 57, 381-388.

