Health
Vol. 4 No. 4 (2012) , Article ID: 18836 , 8 pages DOI:10.4236/health.2012.44025
Medical errors and their prevention
![]()
Computer and Information Science, Brooklyn College, New York City, USA; *Corresponding Author: mariusz.tybinski@gmail.com
Received 24 December 2011; revised 8 January 2012; accepted 20 February 2012
Keywords: Medical Errors; Mishaps; Complications; CPOE; CDSS; Wrong-Side Surgeries; WSS; 19-Item Checklist Study
ABSTRACT
New protocols and procedures for reducing medical errors will be discussed and evaluated in this paper. Further Computerized Physician Order Entry and Clinical Decision Support Systems coupled with monitoring of adverse drug events will be explored. Then lastly some common mistakes of “Wrong-Side” type surgeries and methods to prevent them will be discussed.
1. INTRODUCTION
The matter of medical errors is not a new topic and it did not become a widespread subject until the last decade. Statistics show the medical field has improved greatly since IOM’s report in 1999; However, those error ratios can still be improved upon or even eliminated completely.
2. MEDICAL ERRORS AND THEIR PREVENTION
2.1. 19-Item Checklist Study
In the study published in 2009 by The New England Journal of Medicine it was reported that implementation of the Surgical Safety Checklist (based on the first edition of the World Health Organization Guidelines for Safe Surgery) helped eliminate some surgical complications and mishaps.
2.2. The Checklist
The Back in 2008 the World Health Organization published recommended guidelines, principles, and recommended practice to improve the safety of patients. Based on WHO’s guidelines, a 19-Item check list was designed with the intention of reducing the rate of major surgical complications and mishaps [1].
The implementation involved a two step process. First, the initial baseline data was collected, and then each local investigator was advised of the analyzed deficiencies and asked to implement the 19-Item check list (Table 1).
This study was conducted in eight participating hospitals within the WHO region (Table 2). For each hospital a local data collector was chosen and trained accordingly (Table 3). This employee worked full time on the conducted study and was not assigned any clinical or hospital duties at the time. The list was introduced to the staff by lectures, written material, or direct training. Each hospital designated between 1-to-4 operating rooms and all patients of 16 years of age and older ware consecutively enrolled [1].
2.3. Observations and Data Gathering
The study data was collected from the individual local collectors and/or from the clinical teams involved. The information gathered from surgery recovery period included demographics of patients, procedural safety, and type of the anesthetic data. The information was collected primarily from patient’s first 30 days or until discharge. The collection of data aimed for 500 consecutively enrolled patients [1].
The researchers’ defined complications included “acute renal failure, bleeding requiring the transfusion of 4 or more units of red cells within the first 72 hours after surgery, cardiac arrest requiring cardiopulmonary resuscitation, coma of 24 hours’ duration or more, deep-vein thrombosis, myocardial infarction, unplanned intubation, ventilator use for 48 hours or more, pneumonia, pulmonary embolism, stroke, major disruption of wound, infection of surgical site, sepsis, septic shock, the systemic inflammatory response syndrome, unplanned return to the operating room, vascular graft failure, and death” [1].
2.4. 19-Item Checklist Results
In this study a 20% reduction in complications was found by the researchers after the checklist was implemented with a statistical power of 80%.
There were 3733 enrolled patients during the baseline period and 3955 patients after the introduction of the 19-Item check list (Table 4).
The error complications for any of the sites dropped to 7% from 11% (at the initial baseline) on the average of every site, and the total in-hospital rate of death dropped
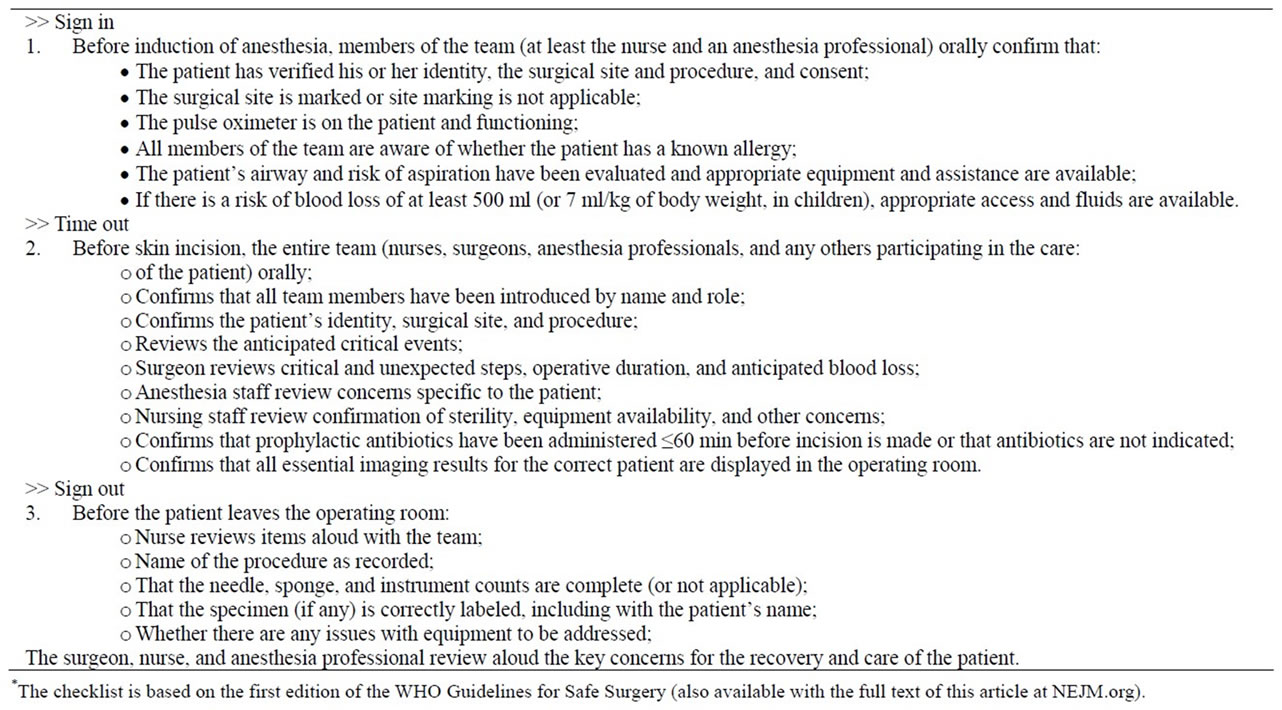
Table 1. Elements of the surgical safety checklist*.
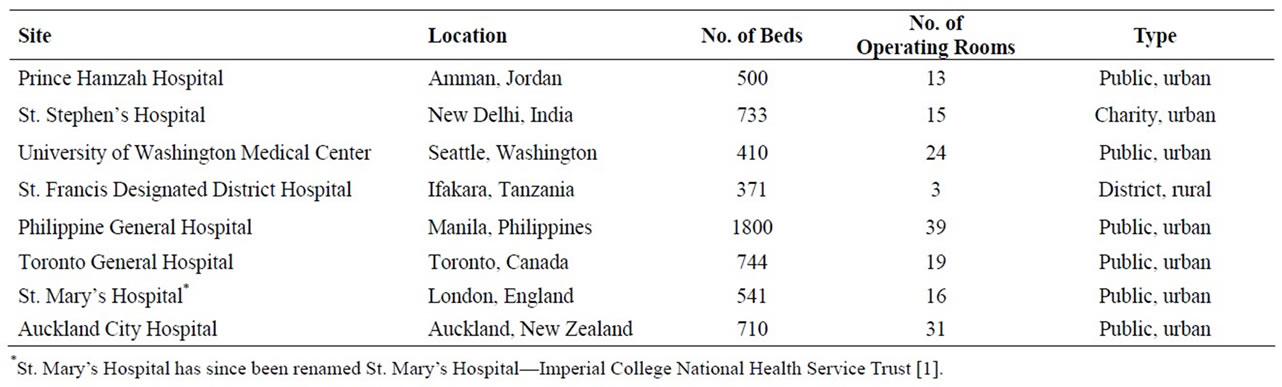
Table 2. Characteristics of participating hospitals.

Table 3. Surgical safety policies in place at participating hospitals before the study.

Table 4. Characteristics of the patients and procedures before and after checklist implementation, according to site*.
to. 08% from 1.5% (Table 5). The surgical complications and death rate fell on average by 36%. Every hospital had a decrease of major postoperative complications with a significant reduction at three sites (one in a high-income location and two in lower-income locations). Even though in some hospitals a few effects of the intervention were stronger than the others, no single hospital was responsible for the overall rate change, nor was the rate limited exclusively to a high or low income hospital. From these findings it was concluded that the checklist program is an improvement among diverse clinical and economical environments.
3. COMPUTERIZED PHYSICIAN ORDER ENTRY (CPOE) AND CLINICALDECISION SUPPORT SYSTEMS (CDSS) OVERVIEW
One of the most common, clinically important and costly problems is Medication errors and adverse drug events (ADEs)—injuries that result from the use of a drug [2]. Both adult and pediatric studies have found that about half of all medication errors occur during the drug ordering, although another technique—direct observation, has shown that errors also occur during the administration stage. The principle types of medication errors are: missing a dose, incorrect dose, route or frequency of taking the medications. The introduction of computerized physician order entry (CPOE) with clinical decision support systems (CDSSs) may reduce medication-related errors [3].
Complete and standard formatted orders are only accepted by the basic CPOE systems. Almost all modern CPOE systems are somehow integrated with CDSSs— either include complete CDSSs or have an interface. Clinical decisions can include values or suggestions for drug routes, frequencies, doses. More advanced CDSSs perform allergy, interaction and value checks. They can also provide reminders about orders and other useful features.
The second type of CDSSs is called isolated CDSSs. They are stand-alone systems that provide advice on selection, dosage, and duration or drugs. More refined CDSSs are using patient-specific information and their advice is based on this information. After using CDSS system, the physician has to proceed with a handwritten medication order.
It is estimated that about 780,000 patients were injured or died in hospitals across the US from ADEs annually. Based on studies by a few US hospitals, incidence rates of ADEs range between 3 to 7 per every 100 admissions. Researchers use different definitions and criteria and that is why it is difficult to calculate a national estimate. One study demonstrated that 57% OCEs occurred at the ordering stage, 34%-administration stage, 7%-transcribing stage, and 3%-dispensing [3].
3.1. CPOE and CDSS Study Designs
This paper reviews four studies that evaluate CPOE with CDSSs. The first study is a randomized controlled trial that evaluates utility of CPOE in improving prescriptions. This study was done by the Regenstrief Institute for Health Care. Other three studies evaluate CPOE systems at Brigham and Women’s Hospital (BWH). The first BWH study compares a period of intervention of CPOE with CDSSs on surgical, intensive and medical care wards with a historical period. The other two studies are time-based analysis of orders [4].
Table 6(b) shows four studies that evaluate isolated CDSSs.
The first BWH study demonstrated a 55% decrease in non-intercepted serious medication errors. This study

Table 5. Outcomes before and after checklist implementation, according to site*.
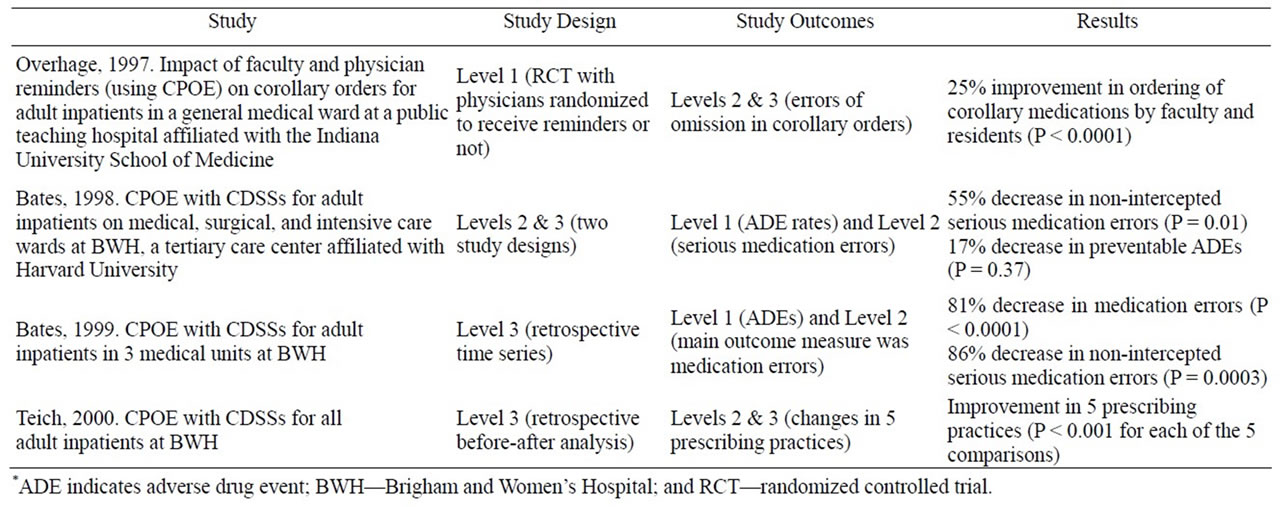
Table 6(a). Studies of computerized physician order entry (CPOE) with clinical decision support systems (CDSSs)*.
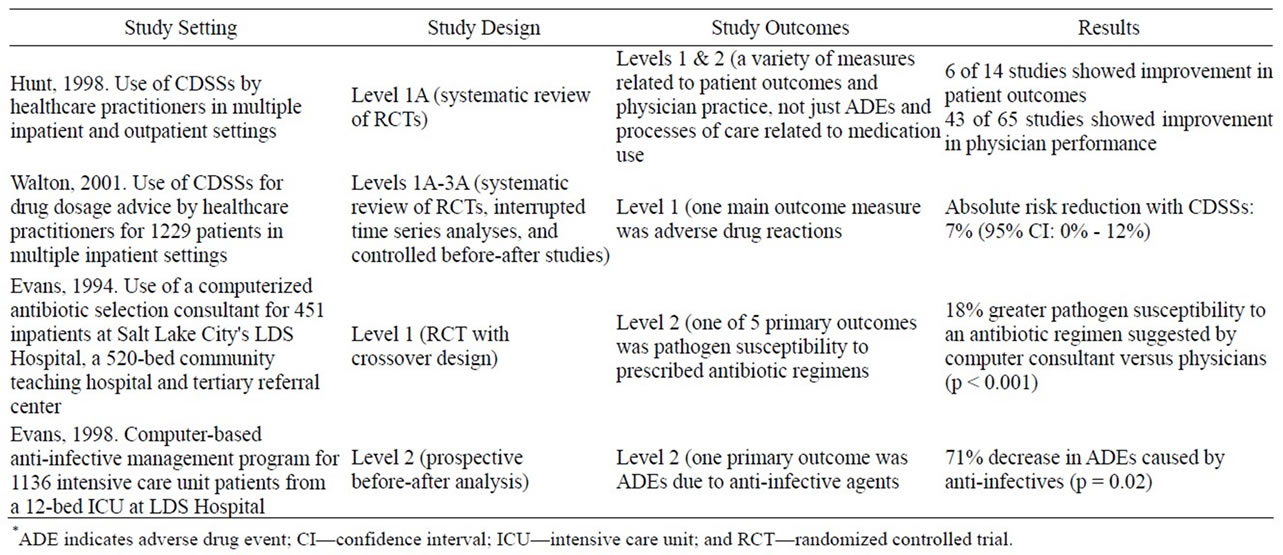
Table 6(b). Studies of clinical decision support systems (CDSSs)*.
also found a 17% decrease in preventable ADEs. The second study, showed marked reductions in all errors except dose errors and in non-intercepted serious errors. The number of ADEs was small—only 25 during the baseline. The total number of ADEs per thousand patient days decreased from 14.5 to 9.5 (p = 0.09). For preventable ADEs, the reduction was 0.05 [5].
Both Overhage and Teich studies demonstrate the evidence that CPOE with CDSSs can decrease medication errors in all areas. At the same time the reduction in ADEs did not achieve any significance in one study, and only achieved some in one of the outcomes in the other study [6]. Furthermore, the all the systems were developed internally and were not purchased.
In the studies evaluating CDSSs, two were systematic reviews. Hunt’s review showed that 6 of 14 studies demonstrated improvement in patient outcomes and 43 of 65 studies demonstrated improvement in physician performance. The conclusion here is that CDSSs can enhance preventive care, drug dosage, other aspects of medical care performance, but the CDSS’s impact on patient outcomes is still unclear. Walton’s review evaluated computerized drug dosage and showed a 7% decrease in adverse drug reactions. The 1994 Evans study evaluated the use of a computerized antibiotic selection consultant, and showed an 18% greater susceptibility to an antibiotic suggested by an electronic system versus a physician. The 1998 study by Evans demonstrated a 71% decrease in ADEs caused by anti-infectives when using a computer based anti-infective systems [7]. These CDSSs studies showed improvements in medical errors with significance.
3.2. Potential for Harm
While CPOE and CDSS systems proved themselves to be very effective systems for reducing medical errors, they may also cause additional problems. For example, an incorrect dosage suggestion may lead to an incorrect ordering choice by the physician.
There were Also cases where a physician would accidently write an order in the wrong patient records.
In addition, alarm systems should be appropriately balanced between sensitivity and specificity. Physicians should receive a warning whenever a potential harm is possible, but at the same he/she should not be overwhelmed by many “false positive” alerts. Hardware and software outage should also be considered.
3.3. Costs and Benefits
Six of the studies evaluated in this paper are known as “home-grown” systems. The costs of commercial systems are significantly greater than the costs of developing the same systems. For BWH, the CPOE development and implementation cost was estimated to be $1.9 million, with a maintenance cost of $500,000 annually. At the same time, the cost of complete commercial systems varies and may be on the order of tens of millions of dollars [8].
While everyone recognizes that CPOE systems require a significant capital investment, research has shown that the average return on investment for such systems can range from $180,000 - $900,000 annually [8]. Furthermore, with some additional improvements in reduction in testing and imaging as well as resource utilization, some hospitals can save millions of dollars annually.
4. WRONG-SITE SURGERIES
A wrong-side surgery is a surgery that was made on the wrong site of the body or for a wrong patient. This problem became even more prevalent for the past decade. During the Joint Commission’s Sentinel Event program the number of wrong-side surgeries (WSS) that were reported increased from 15 cases in 1998 to a total number of 592 cases by June 30, 2007 [9]. “Incidence, patterns, and prevention of wrong-site surgery” study states that these kind of errors happen once in 112,994 cases [10]. For instance the New York State Department of Health reported 46 cases in 2 years using a mandatory reporting system. A survey of hand surgeons stated that 20% of the 100 respondents had operated on the wrong site at least once during their professional career and even 16% of them had prepared to operate on the wrong site, but realized their error before making an incision [11]. However this number of errors is much higher out of operating rooms, for example they may occur during ambulatory surgery or interventional radiology.
Wrong-site surgeries usually occur in orthopedic or podiatric procedures, general procedures, urological and neurosurgical procedures.
So why do we pay so much attention to them if wrongsite surgeries are approximately rare (1:100,000) and most of them (64%) do not result in permanent injury?
WSS are pretty important as they are a result of some previous small failures and become a symptom of the systems and culture of the health care. Where by fixing them we will address a much bigger problem for health care.
Failures that result in a WSS may occur any moment during the time a patient has entered a hospital until a surgery has completed. Poor handwriting, wrong medical record review, wrong patient assessment, lack of communication among operative team are key problems. A chance of error may increase when multiple procedures are operated on the same patient, when the operative team is under time pressure and some previous changes were made to the operative team.
4.1. Ways of Preventing a WSS
Initial attempts to avoid WSS were focused on developing an awareness mechanism for identifying a correct site. American Academy of Orthopedic Surgeons developed a campaign to prevent WSS by marking the correct surgical site that was named “Sign Your Site” [12]. Apparently a simple process was actually confusing doctors because they often thought that the marked site was the site where they should not operate. So later on to make this program more effective doctors had to mark an incorrect site with word “No” and after that a surgical team had to work together to verify the correct site.
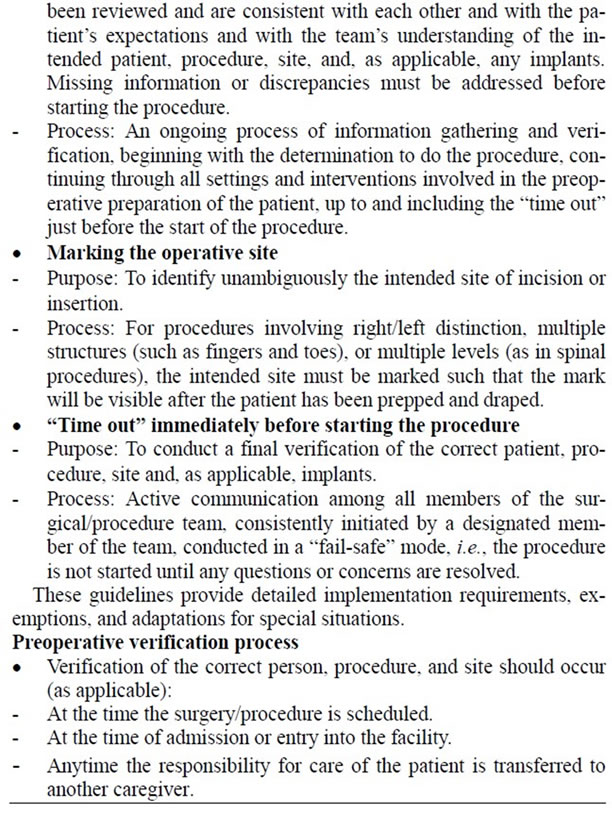
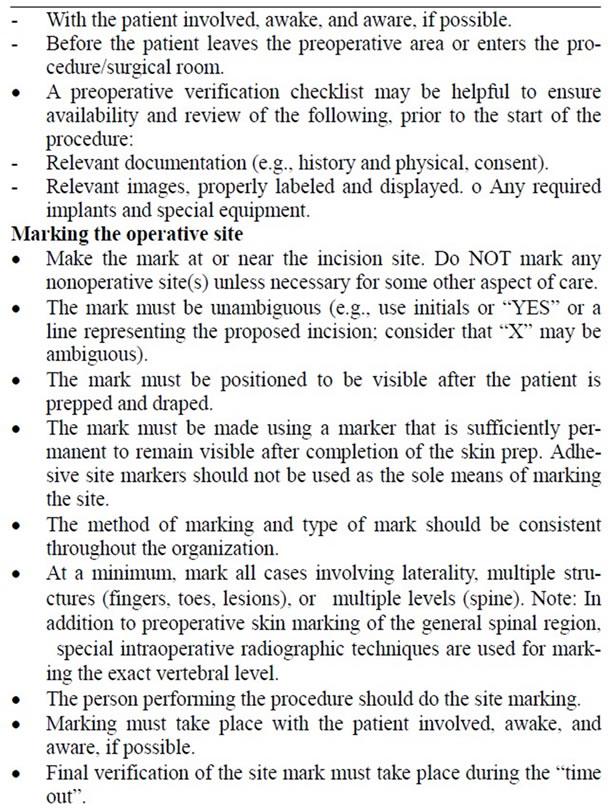
A summit of Joint Commission in 2003 brought many health care professionals and others to discover a way to reduce or eliminate WSS. This summit was devoted to problems of WSS impact on patients, their families and health care professionals and had to address continued escalation of reported WSS cases. As a result of this summit The Universal Protocol for Preventing Wrong Site, Wrong Procedures, and Wrong Person Surgery TM was created [13].
4.2. The Universal Protocol
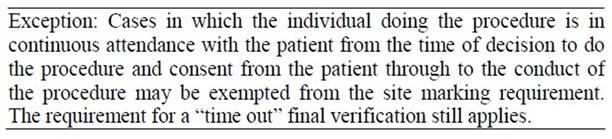
The Universal Protocol requires a critical 3-step process: “A pre-procedure verification, marking the correct surgical site and a “time-out” for the operating stuff just before the surgery”. For the study Stanhel’s team was able to collect surgical errors data from the company that provides liability insurance to 6000 doctors in Colorado [13].
The Universal Protocol has to be used in ambulatory care, hospitals, critical access hospitals, and office-based settings. It was first used on July 1, 2004 when all three key elements were included in accreditation process for health care organizations.
The Universal Protocol is stated below in Text Box 1.
The Joint Commission Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery TM.
4.3. Reports
The collected data by the authors indicates 27,370 reported events between January 2002 and June 2008 and among them the researchers found 25 wrong-patient and 107 wrong-side operations. From 25 reported patients, 5 received unnecessary surgeries and 38 patients (from 107 wrong-side reported patients) received operations that significantly harmed patients’ health—including one death.
There was an 85% judgment error rate for the operations on the wrong-side of the body and 72% due to not performing the “time-out” which was required by the protocol.
“Time-out” is an occurrence just before the operation begins where all parties involved check for the right patient and what he or she will be operated on. Stahel notes that the system alone cannot solve any of the surgical related problems in the OR.
The researchers further point out that “Once we were fully responsible for our actions—now we hide behind a safety system that should cover the problem. The time-out is performed, but people are not mentally involved—the system alone cannot protect you from wrong-site surgery”. Then he points out that the doctors should take more personal responsibility for their errors stating “We are going from a culture of blame to a culture of system safety, and we should move on to a culture of patient safety and accountability” [13].
An Associate Professor of Surgery at Johns Hopkins University and author of an accompanying journal editorial, Dr. Martin A. Makary said, that “a simple checklist does not solve the problem; it’s not that simple. The culture has to change to promote people speaking up when they see a safety concern and promote good teamwork”.
Consequently Makary states that often the staff (doctors, nurses etc.) don’t even know each other’s names and that the “mechanical” culture places doctors above the nurses and other staff. He writes “A nurse or a lowlevel person in the surgical hierarchy may sense that something is not right, but they don’t speak up because they are intimidated by the operating room hierarchy.” Then he concludes that this culture needs to change and by removing intimidation.
5. CONCLUSIONS
Based on the research above we conclude that the number of medical errors has become an increasingly larger concern in the last few decades. Methods like safe practice and universal procedures, checklists, and various computerized systems have proven effective in reduction of medical errors. Even though none of the implemented systems, protocols, or formed checklists helped eliminate those mishaps completely—the data however, clearly shows that error rates have been reduced significantly. Yet there is still a room for improvement, considering people’s lives can be saved and hospital financial burden reduced in the near future.
![]()
![]()
REFERENCES
- Haynes, A.B., Weiser, T.G., Berry, W.R., Lipsitz, S.R., Breizat, A.-H.S., Dellinger, P., et al. (2009) A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine, 360, 491-499. doi:10.1056/NEJMsa0810119
- Dyer, C.C., Oles, K.S. and Davis, S.W. (1984) The role of the pharmacist in a geriatric nursing home: A literature review. Drug Intelligence & Clinical Pharmacy, 18, 428-433.
- Jenkins, M.H. and Bond, C.A. (1996) The impact of clinical pharmacists on psychiatric patients. Pharmacotherapy, 16, 708-714.
- Bates, D.W., Cullen, D.J., Laird, N., Petersen, L.A., Small, S.D., Servi, D., et al. (1995) Incidence of adverse drug events and potential adverse drug events: Implications for prevention. JAMA, 274, 29-34. doi:10.1001/jama.1995.03530010043033
- Jha, A.K., Kuperman, G.J., Teich, J.M., Leape, L., Shea, B., Rittenberg, E., et al. (1998) Identifying adverse drug events: Development of a computer-based monitor and comparison with chart review and stimulated voluntary report. Journal of the American Medical Informatics Association, 5, 305-314. doi:10.1136/jamia.1998.0050305
- Classen, D.C., Pestotnik, S.L., Evans, R.S., Lloyd, J.F. and Burke, J.P. (1997) Adverse drug events in hospitalized patients. Excess length of stay, extra costs, and attributable mortality. JAMA, 277, 301-306. doi:10.1001/jama.1997.03540280039031
- Sokol, A.J. (2001) Financial benefits of electronic medical records. www.ehealthcoach.com/FR-FinBenElecMedRec.asp
- Joint Commision (2007) Sentinel event statistics as of June 30. http://www.jointcommission.org/sentinel_event.aspx
- Kwaan, M.R., Studdert, D.M., Zinner, M.J. and Gawande, A.A. (2006) Archives of Surgery, 141, 353-357.
- Meinberg, E.G. and Stern, P.J. (2003) Incidence of wrongsite surgery among hand surgeons. Journal of Bone & Joint Surgery, 85, 193-197.
- American Academy of Orthopedic Surgeons (2006) Wrong site surgery. http://www5.aaos.org/wrong/viewscrp.cfm.
- Joint Commission (2003) Universal protocol for preventing wrong site, wrong procedure, wrong person surgery. http://www.jointcommission.org/
- Steven, R. (2011) Surgery on wrong patients, surgical sites persists, study finds. http://www.businessweek.com/lifestyle/content/healthday/644585.html