Open Journal of Urology
Vol.4 No.5(2014), Article ID:46346,8 pages DOI:10.4236/oju.2014.45008
Comparison of Results of TIPU Repair for Hypospadias with “Spongioplasty Alone” and “Spongioplasty with Dorsal Dartos Flap”
Amilal Bhat1*, Manish Singla1, Mahakshit Bhat2, Karamveer Sabharwal1, Vinay Kumar1, Ravi Upadhayay1, Ram Kishan Saran1
1Department of Urology, S.P. Medical College Bikaner, Bikaner, India
2Department of Preventive and Social Medicine, S.P. Medical College Bikaner, Bikaner, India
Email: *amilalbhat@rediffmail.com, drmanishsingla@gmail.com, mahak199027@gmail.com, drkvsabharwal@gmail.com, vinaysinghkgmc99@gmail.com, surgeon.ups@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 26 February 2014; revised 20 March 2014; accepted 28 March 2014
ABSTRACT
Objective: The aim of our study was to compare the results of tubularized plate urethroplasty with interposing healthy tissue spongioplasty alone and spongioplasty with dorsal dartos flap to assess the role of dartos flap in prevention of fistulae. Patients and Methods: A retrospective study was performed on 80 patients, aged 4 months to 27 years who underwent hypospadias repair using the Snodgrass technique. The patients were assigned to two groups. In group I (40 patients) the neourethra was covered with spongioplasty only, and in group II (40 patients) the neourethra was covered with spongioplasty plus dartos flap. Integrity of the urethral plate was maintained in all the cases. The ventral curvature & torsion was corrected by penile de-gloving, mobilization of the urethral plate and spongiosum and mobilization of the proximal urethra if needed. The results were analysed in view of complication rates. The average period of hospital stay was 7 days & follow-up varied from 8 months to 28 months with a mean of 14 months. Results: In group I, hypospadias were distal penile in 31 (77.5%), mid-penile in 4 (10%) and proximal/peno-scrotal in 5 (12.5%) patients. In group II, hypospadias were distal penile in 17 (42.5%), mid penile in 9 (22.5%) and proximal/peno-scrotal in 14 (35%) patients. Sixty five percent in group I and 80% in group II had ventral curvature but the difference was not statistically significant. Good functional results were achieved in 97.5% patients in group I and in 95% patients in group II which were statistically similar (p value—0.585). Urethral fistula was encountered in 2.5% in group I & in 2 cases (5%) in group II. Meatal stenosis was noted in 7.5% each in both groups, which responded to urethral dilatation. One patient in group II had complete disruption. There was no statistically significant difference in early and late complications in both groups (p value—0.812). Conclusions: Spongioplasty with healthy spongiosal tissue is strong enough and is effective waterproofing as an interposition layer. However, more prospective studies in different hands are needed to omit the step of dorsal dartos interposition.
Keywords:Congenital Anomalies, Hypospadias, Urethroplasty, Dorsal Dartos Cover, Spongioplasty Hypospadias Repair Complications, Urethral Fistula

1. Introduction
Since its introduction in 1994, Tubularized Incised Plate Urethroplasty (TIPU) has gained widespread popularity because of its versatility, low complication rate, and good cosmetic results [1] . Although TIPU repair is well described, there are some variations in surgical technique which can affect the functional and cosmetic outcome. Many methods have been described in the literature for the interposition of tissue to cover the neo-urethra beginning with transverse island dorsal subcutaneous flap, which was soon found to be unfavorable because of skin coverage problems and penile torsion [2] . Later various other methods included dorsal [3] , lateral, single or double [4] , dartos flaps, ventral based dartos flap [5] [6] , scrotal dartos [7] , de-epithelised local penile skin [2] , preputial flap, paraurethral tissue [8] , spongioplasty [9] -[17] , or tunica vaginalis flaps [18] [19] . Out of all these, the dorsal dartos flap is used by most surgeons, but there is still no consensus over the ideal interposing tissue in TIPU. Because of edema, necrosis of skin, hematoma and torque with mobilization of the dorsal dartos flap [20] its role as an interposing tissue had been questioned [17] . So in view of these complications, we analyzed our data and compared the results of TIPU repair with spongioplasty alone and with dartos flap.
2. Patients and Methods
A retrospective study was performed on 80 patients (from January 2006 to December 2010) aged 4 months to 27 years who underwent hypospadias repair using the Snodgrass technique (TIPU).
Exclusion criteria: Poorly developed corpus spongiosum, redo cases and cases requiring transection of the urethral plate.
Inclusion Criteria: All patients who had spongioplasty alone or spongioplasty with dartos flap and came for follow-up at least three times or more annually.
Quality of spongiosum was considered as follows: 1) thin fibrous with minimal spongiosal tissue which on spongioplasty was less than the diameter of proximal healthy urethra as “poorly developed” (Figure 1), 2) good

Figure 1. Showing poorly developed spongiosum with minimal spongiosal tissue. A. Mobilized spongiosum on right side; B. Mobilized spongiosum on left side; C. Spongisum seen from both side with minimal spongiosal tissue; D. Spongioplasty after tubularization of urethral plate.
spongiosum tissue with good vascularisation, healthy robust spongiosum, which becomes bulkier than the native spongiousm on spongioplasty as “well developed” (Figure 2). Six patients with a poor spongiosum were excluded from the study in group I and 8 cases in group II. The patients were assigned to two groups. In group I (40 patients) the neo-urethra was covered with the paraurethral spongial tissue only and in group II (40 patients) the neo-urethra was covered with spongioplasty plus the dartos flap.
Surgical Technique: An inverted U-shaped incision is made encircling the meatus to the corona, preserving the urethral plate, and then extended circumferentially around the corona (except where prepucioplasty is contemplated). A Gitte’s test is done to evaluate the chordee after penile de-gloving. Mobilization of the urethral plate and the corpus spongiosum is done after creating a plane just proximal to the meatus. Dissection is performed lifting the spongiosum from corporal bodies, taking care taken not to damage the corpus spongiosum or corpus cavernosum (Figure 1A & Figure 1B). The proximal urethra is mobilized up to the bulbar region in case of persistent chordee/torsion until adequacy is confirmed by Gitte’s test. Subsequently the corpus spongiosum is dissected into the glans (Figure 2A), glanular wings are raised, and glanular chordee correction is checked by Gitte’s test [20] . The urethral plate is tubularized with or without a dorsal incision using 7-0 PDS, and spongioplasty is done with 7-0 PDS by suturing the edges of mobilized spongiosum to complete the urethroplasty (Figure 1D & Figure 2D). A 6Fr to 10 Fr urethral catheter, depending on patient age, left in situ. The dorsal dartos vascular flap wrap is performed to allow additional tissue cover in group II cases. Skin sutures are applied with or without drainage. Pressure dressing is applied in all cases with cotton gauze and double elastic adhesive tape. The urethral catheter is removed on postoperative day 7 to 10 and patient is discharged. Patients are followed up at 1, 3, 6 and 12 months and then annually for cosmesis, fistula, meatal stenosis and any other complication. Patients were asked to void to visualize the stream and checked for any leakage/stream other than the meatus (suggestive of a fistula) and the urethra was calibrated to check urethral stricture and meatal stenosis. The average period of hospital stay was 7 days & follow-up varied from 8 months to 28 months with a mean of 14 months.
Statistical Method: Statistical analysis was done by using Student’s t-test with p < 0.05 considered to be statistically significant.
3. Results
In group I age of the patients varied from 1 year to 27 years with a mean of 9.2 years while in group II (40 patients) age varied from 4 months to 23 years with a mean of 8.2 years; this was comparable in both groups (χ² value—6.252, p value—0.282 Table 1). In group I the meatus was coronal/sub-coronal in 11 (27.75%), distal penile in 20 (50%), mid-penile in 4 (10%) and proximal/ penoscrotal in 5 (12.5%) patients. Similarly In group II, the meatus was coronal/subcoronal in 6 (15%), distal penile in 11 (27.5%), mid-penile in 9 (22.5%) and proximal/penoscrotal in 14 (35%) patients. There was a significant difference in the type of hypospadias in both
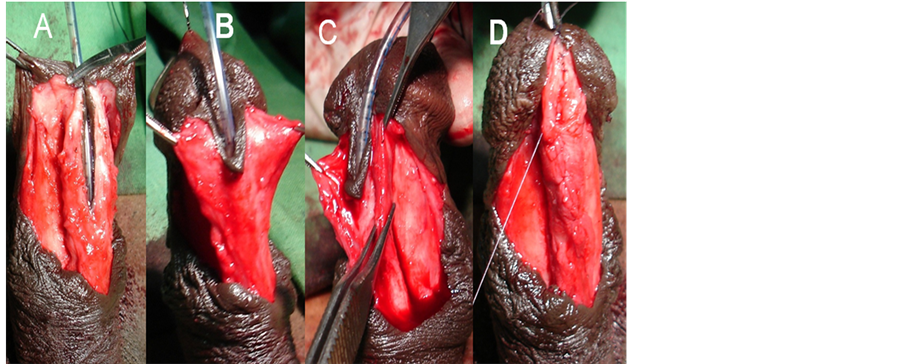
Figure 2. Showing well developed spongiosum with robust healthy spongiosal tissue: A-C. Mobilized healthy robust spongiosum; D. Showing diameter after spongioplasty larger than normal proximal healthy urethra.
groups with χ² value—10.26 p value—0.005 (Table 2). Mild chordee was seen in 10 patients, moderate in 6 patients and severe in 10 patients in group I while mild chordee was present in 17 patients moderate in 5 while severe in 10 patients in group II. There was no significant difference in ventral curvature in both groups; χ² value —1.298 p value—0.522 (Table 3). Chordee correction was done by penile de-gloving in 6 cases, mobilization of the proximal urethra in 2 cases and combination of penile de-gloving and urethral plate mobilization in 18 cases in group I. While in group II curvature correction was done by penile de-gloving in 11 cases, by the urethral mobilization in 3 cases and a combination of penile de-gloving and the urethral plate mobilization was used in 18 cases. There was no significant difference in the steps used for correction of curvature in both groups; χ² value—1.298 p value—0.522 (Table 4) In group I, 1 patient had mild torsion(≤45˚), which was corrected by mobilization of the urethral plate with the spongiosum 5 had moderate torsion (45˚ - 90˚) which required mobilization the urethral plate in to the glans in addition to mobilization of the urethral plate with the spongiosum while 2 had severe torsion (≥90˚) which required proximal urethral mobilization along with the above two steps. In group II, 10 patients had mild torsion, 2 had moderate torsion and 1 had severe torsion. Correction of torsion was done by penile de-gloving 5 cases, de-gloving with the urethral plate mobilization in 6 cases and proximal urethral mobilization in addition required in two cases. Though there was difference in number of patients having torsion and degree of torsion but there was no significant difference in steps used for correction of torsion (Table 5 & Table 6). Integrity of the urethral plate was maintained in all the cases, the technique used for cor
Table 1. Showing the comparison number patients in both group in relation to age.
χ² value—6.252, p value—0.282 (non significant).
Table 2. Showing the comparison number patients in both groups in relation to type of hypospadias.
χ² value—10.26, p value—0.005 (significant).
Table 3. Showing the comparison number patients in both groups in relation to ventral Curvature.
χ² value—1.298, p value—0.522 ( non significant).
Table 4. Showing the comparison number patients in both groups in relation to correction of curvature.
Table 5. Showing the comparison number patients in both group in relation to penile torsion.
χ² value—9.37, p value—0.009 ( significant).
Table 6. Showing the comparison number patients in both group in relation to correction of penile torsion.
rection of chordee, torsion and tubularization was similar in both groups and had no statistical difference. In eight patients in group I and seven cases in II urethra were tubularized without incision.
Excellent or good results were achieved in 39 patients in group I and in 38 patients in group II. Early post operative complications of Clavien Classification grade II were mainly mild prepucial edema in 5 cases each in both groups, and hematoma in one patient in group I and two patients in group II, the difference in two group was not statistically significant (p value—0.585). A urethral fistula was noticed in one case in group I & in 2 cases in group II. One patient in group II had complete disruption of the wound .The fistulae and urethral disruption of Clavien Classification grade IIIb was repaired successfully. Mild meatal stenosis was noted in 3 cases each in both the groups and was successfully treated by meatal calibration (Clavien Classification grade IIIa). There was no statistically significant difference in early and late complications in both groups (p value— 0.812 Table 7). We achieved 100% positive results after fistula repair and meatal dilation. None of the patients had residual chordee, torsion, stricture or a fistula during follow-up.
4. Discussion
TIPU repair is recommended as the primary treatment for anterior hypospadias, mid-shaft hypospadias and possible selected proximal ones [21] -[23] . A transverse island of dorsal subcutaneous tissue is used as a interposition flap in original description of TIPU. Later on modification like a buttonhole fashion to cover the neourethra ventrally, lateral dartos flap and spongioplasty with separation of the corpora cavernosa were used [1] [24] -[27] . We do spongioplasty after mobilization of the spongiosum lateral to medial along with urethral plate and suturing the edges to midline converting the diverting Y spongiosum to I as reported by Yerkes et al. [27] with the difference that we don’t incise the spongiosum transversely at corona but mobilize into glans and spongioplasty up to distal most part of neourethra which has an added advantage of covering the neourethra with healthy spongiosum to prevent fistula at corona. Dodet et al. have incised the spongiosum both medially starting from the meatus to the tip of glans and laterally on the external borders of the urethral plate then the urethra.

Table 7. Showing comparison of early and late complications in both groups.
Then the spongiosal pillar are mobilized from corpora cavernosa and sutured medial edges of spongium over neourethra [26] . Advantages of mobilization of spongiosum with urethral plate are that tubularization of urethral plate and spongioplasty is without any tension on the sutures [28] . Mobilization of the spongiosum with urethral plate also helps in tubularization without a midline incision [20] [27] . We could tubularize 20% cases in group I and 17.5% cases in group B without a midline incision.
The variable rate of success can be due to anatomy of spongiosum and its technique suturing the spongiosum [28] . We did not find any classification of spongiosum in the literature but it is important as vascularity vary with the development. So we graded the spongiosum as to well developed good healthy robust vascularised spongiosum which becomes bulkier than the native proximal spongiousm on spongioplasty and poorly developed thin minimal spongiosal tissue with poor vascularisation which on spongioplasty was less than the diameter of proximal healthy urethra. Results of spongioplasty with well developed are usually good, so proposed classification will be useful in choosing the cases of spongioplasty alone. We included patients with well developed spongiosum.
The reported fistula rate with spongioplasty ranges from 0% to 31%. While several investigators have shown spongioplasty to be as protective as a dartos flap [13] [26] -[28]
But others placed dorsal dartos barrier flap over the neo-urethra though they has shown reduced fistula rate but it alone is not sufficient [13] [17] . Bilici et al. compared results of TIPU compared to the dartos flap alone and spongioplasty plus dorsal dartos flap and had (8%) higher fistula rate in the dorsal dartos alone group. They concluded that the use of the corpus spongiosum as an intermediate layer in urethral coverage, combined with the dartos flap, reduces the likelihood of fistula formation and can be applied easily and effectively [8] . In our series, results with spongioplasty alone were almost equivalent or better as compared to TIPU with spongioplasty plus a dartos cover. The fistula rate was the same in both groups but one of the patients in the spongioplasty plus dartos group had total disruption of the neo-urethra. Probable explanations for the better results of spongioplasty alone in our series are that we included cases with a well developed healthy spongiosal tissue; minimal dissection resulted in less hematoma/infection and skin vascularity was well preserved. Also since all cases were done by a single surgeon so efficiency increased with subsequent procedures. The reasons of failure with spongioplasty in results of other authors may be that they used a poorly developed spongiosum tissue alone which was not strong enough to prevent fistula formation or may be other factors like a narrow urethral plate or severe chordee negatively affected the overall results. Other advantages of the Y to I spongioplasty after mobilization of spongiosum are, that it adds length to the urethra and penis, which, also helps in the correction of chordee. In addition, spongioplasty gives an almost normal shape to the urethra, and the repair is more anatomical. Finally spongioplasty adds an extra layer of locally available healthy vascular tissue avoiding dissection for other flaps [26] -[28] . Spongioplasty alone spares the dorsal hood that can be utilized for preputioplasty which is demanded by many patients/parents [29] . Disadvantages of a dartos flap are that dissecting the dartos fascia from the preputial skin would compromise the vascularity of the skin which if required to cover the ventral side would give way and be responsible for an increase in the incidence of fistulae. Combining both the dartos plus spongiosum would also increase the tissue bulk and lead to glans and skin dehiscence. The sequelae of a dorsal dartos flap are edema, necrosis of skin, hematoma, torsion and longer operating time. So we are of the opinion that when the corpus spongiosum is dissected and mobilized adequately from meatus to the glans tip, spongioplasty alone is strong enough for neourethral coverage and the step of dartos cover can safely be omitted in cases where the corpus spongiosum is well developed.
We discharged the patients from hospital after removal of per urethral catheter after 5 - 7 days, thus increasing the hospital stay, but this was done deliberately because of lack of the basic/specialist surgical services at home towns/villages of our patients who come from far off/remote places to our tertiary centre.
The limitations of our study were being retrospective, a small sample size, and a time lapse between the two study groups. Also, cases in both groups did not have an exact match, but this is difficult in retrospective studies. There was a difference in the type of hypospadias and degree of the torsion in two groups but there was no difference in the numbers of cases for each step in correction of curvature, torsion and urethroplasty done in both groups, which thus makes them comparable. The strength of our study is that all cases were done by the same author; in similar work conditions and, cases were of the same socioeconomic status.
5. Conclusion
Excellent functional and cosmetic results were achieved after repair of hypospadias by using TIPU and spongioplasty. Not using the dartos flap, with the corpus spongiosum as an intermediate layer in urethral coverage, did not affect the complication rate in our experience. Considering the results of our study, the step of dorsal dartos coverage can easily be omitted after spongioplasty done with a well developed spongiosum, but still more prospective studies will be useful to confirm the facts in multiple hands to omit the dorsal dartos cover.
References
- Snodgrass, W. (1994) Tubularized, Incised Plate Urethroplasty for Distal Hypospadias. Journal of Urology, 151, 464- 465.
- Ross, J.H. and Kay, R. (1997) Use of a De-Epithelialized Local Skin Flap in Hypospadias Repairs Accomplished by Tubularization of the Incised Urethral Plate. Urology, 50, 110-112. http://dx.doi.org/10.1016/S0090-4295(97)00212-4
- Mustafa, M., Wadie, B.S. and Abol-Enein, H. (2008) Standard Snodgrass Technique in Conjunction with Double-Layer Covering of the Neourethra with Dorsal Dartos Flap Is the Therapy of First Choice for Hypospadias. International Urology and Nephrology, 40, 573-576. http://dx.doi.org/10.1007/s11255-008-9363-6
- Yildiz, A. and Bakan, V. (2010) Comparison of Perimeatal-Based Flap and Tubularized Incised Plate Urethroplasty Combined with Singleor Double-Layer Dartos Flap in Distal Hypospadias. Urologia Internationalis, 84, 265-268. http://dx.doi.org/10.1159/000288226
- Soygur, T., Arikan, N., Zumrutbas, A.E., et al. (2005) Snodgrass Hypospadias Repair with Ventral Based Dartos Flap in Combination with Mucosal Collars. European Urology, 47, 879-884. http://dx.doi.org/10.1016/j.eururo.2005.02.022
- Furness 3rd, P.D. and Hutcheson, J. (2003) Successful Hypospadias Repair with Ventral Based Vascular Dartos Pedicle for Urethral Coverage. Journal of Urology, 169, 1825-1827. http://dx.doi.org/10.1097/01.ju.0000058429.18975.30
- Hayashi, Y., Kojima, Y., Kurokawa, S., et al. (2005) Scrotal Dartos Flap for the Prevention of the Urethrocutaneous Fistula on Hypospadias Urethroplasty. International Journal of Urology, 12, 280-283. http://dx.doi.org/10.1111/j.1442-2042.2005.01028.x
- Bilici, S., Sekmenli, T., Gunes, M., et al. (2011) Comparison of Dartos Flap and Dartos Flap plus Spongioplasty to Prevent the Formation of Fistulae in the Snodgrass Technique. International Urology and Nephrology, 43, 943-948. http://dx.doi.org/10.1007/s11255-011-9943-8
- Beaudoin, S., Delaage, P.H. and Bargy, F. (2000) Anatomical Basis of Surgical Repair of Hypospadias by Spongioplasty. Surgical and Radiologic Anatomy, 22, 139-141. http://dx.doi.org/10.1007/s00276-000-0139-7
- Bhat, A. (2008) General Considerations in Hypospadias Surgery. Indian Journal of Urology, 24, 188-194. http://dx.doi.org/10.4103/0970-1591.40614
- Almodhen, F., Alzahrani, A., Jednak, R., et al. (2008) Nonstented Tubularized Incised Plate Urethroplasty with Y-to-I Spongioplasty in Non-Toilet Trained Children. Canadian Urological Association Journal, 2, 110-114.
- Delaage, P.H., Bargy, F. and Beaudoin, S. (2005) Spongioplasty in the Treatment of Hypospadias. Progrès en Urologie, 15, 1120-1123.
- El-Sherbiny, M.T., Hafez, A.T., Dawaba, M.S., et al. (2004) Comprehensive Analysis of Tubularized Incised-Plate Urethroplasty in Primary and Re-Operative Hypospadias. BJU International, 93, 1057-1061. http://dx.doi.org/10.1111/j.1464-410X.2004.04781.x
- Kocvara, R., Dvoracek, J., Dite, Z., et al. (2005) Comprehensive Long-Term Analysis of Hypospadias Repair Using Vascularized Flaps and Tubularized Incized Plates—Report on 588 Cases. Casopis Lékaru Ceských, 144, 7-11.
- Mezzine, S., Beaudoin, S. and Bargy, F. (2005) Medium and Long-Term Evaluation of Spongioplasty in Hypospadias Repair. Progrès en Urologie, 15, 519-523.
- Sarhan, O.M., El-Hefnawy, A.S., Hafez, A.T., et al. (2009) Factors Affecting Outcome of Tubularized Incised Plate (TIP) Urethroplasty: Single-Center Experience with 500 Cases. Journal of Pediatric Urology, 5, 378-382. http://dx.doi.org/10.1016/j.jpurol.2009.02.204
- Snodgrass, W. and Yucel, S. (2007) Tubularized Incised Plate for Mid Shaft and Proximal Hypospadias Repair. Journal of Urology, 177, 698-702.
- Snow, B.W., Cartwright, P.C. and Unger, K. (1995) Tunica Vaginalis Blanket Wrap to Prevent Urethrocutaneous Fistula: An 8-Year Experience. Journal of Urology, 153, 472-473. http://dx.doi.org/10.1097/00005392-199502000-00061
- Chatterjee, U.S., Mandal, M.K., Basu, S., et al. (2004) Comparative Study of Dartos Fascia and Tunica Vaginalis Pedicle Wrap for the Tubularized Incised Plate in Primary Hypospadias Repair. BJU International, 94, 1102-1104. http://dx.doi.org/10.1111/j.1464-410X.2004.05111.x
- Bhat, A. (2007) Extended Urethral Mobilization in Incised Plate Urethroplasty for Severe Hypospadias: A Variation in Technique to Improve Chordee Correction. Journal of Urology, 178, 1031-1035. http://dx.doi.org/10.1016/j.juro.2007.05.074
- Nguyen, M.T., Snodgrass, W.T. and Zaontz, M.R. (2004) Effect of Urethral Plate Characteristics on Tubularized Incised Plate Urethroplasty. Journal of Urology, 171, 1260-1262. http://dx.doi.org/10.1097/01.ju.0000110426.32005.91
- Oswald, J., Korner, I. and Riccabona, M. (2000) Comparison of the Perimeatal-Based Flap (Mathieu) and the Tubularized Incised-Plate Urethroplasty (Snodgrass) in Primary Distal Hypospadias. BJU International, 85, 725-727. http://dx.doi.org/10.1046/j.1464-410x.2000.00479.x
- Mizuno, K., Hayashi, Y., Kojima, Y., et al. (2002) Tubularized Incised Plate Urethroplasty for Proximal Hypospadias. International Journal of Urology, 9, 88-90. http://dx.doi.org/10.1046/j.1442-2042.2002.00426.x
- Snodgrass, W.T. (2002) Tubularized Incised Plate (TIP) Hypospadias Repair. Urologic Clinics of North America, 29, 285-290. http://dx.doi.org/10.1016/S0094-0143(02)00045-9
- Al-Hunayan, A.A., Kehinde, E.O., Elsalam, M.A., et al. (2003) Tubularized Incised Plate Urethroplasty: Modification and Outcome. International Urology and Nephrology, 35, 47-52. http://dx.doi.org/10.1023/A:1025995811691
- Dodat, H., Landry, J.L., Szwarc, C., et al. (2003) Spongioplasty and Separation of the Corpora Cavernosa for Hypospadias Repair. BJU International, 91, 528-531. http://dx.doi.org/10.1046/j.1464-410X.2003.04110.x
- Yerkes, E.B., Adams, M.C., Miller, D.A., et al. (2000) Y-to-I Wrap: Use of the Distal Spongiosum for Hypospadias Repair. Journal of Urology, 163, 1536-1538. http://dx.doi.org/10.1016/S0022-5347(05)67673-2
- Almodhen, F., Alzahrani, A., Jednak, R., Capolicchio, J.P. and El Sherbiny, M.T. (2008) Nonstented Tubularized Incised Plate Urethroplasty with Y-to-I Spongioplasty in Non-Toilet Trained Children. Canadian Urological Association Journal, 2, 110-114.
NOTES

*Corresponding author.


