Open Journal of Urology
Vol.3 No.1(2013), Article ID:28002,4 pages DOI:10.4236/oju.2012.31001
Comparison of 80 W versus 120 W 532 nm Laser Prostatectomy for BPH
1James Buchanan Brady Foundation Department of Urology, Weill Cornell Medical College, New York, USA
2Department of Surgery, Weill Cornell Medical College, New York, USA
Email: #ril9010@med.cornell.edu
Received August 11, 2012; revised October 24, 2012; accepted November 15, 2012
Keywords: Transurethral Resection of Prostate; Prostatic Hyperplasia; Surgical Procedures; Minimally Invasive; Lasers
ABSTRACT
Purpose: Improvements to photoselective vaporization of the prostate (PVP) have been made over time, particularly with the introduction of higher power systems. Few studies however have compared the performance of these systems to their predecessors. The purpose of this study was to compare the clinical and perioperative outcomes of 80 W vs. 120 W PVP. Materials and Methods: A series of 267 and 209 consecutive patients underwent 80 W and 120 W PVP, respectively, from September 2001 to May 2009 at Weill Cornell Medical College (GreenLight™ laser system, American Medical Systems, Inc., Minnetonka, MN). Data were collected on patient demographics, International Prostate Symptom Score (IPSS), prostate-specific antigen (PSA), and perioperative parameters. Maximum flow rate (Qmax), postvoid residual (PVR), and transrectal ultrasound prostate volume were recorded. Statistical analyses were carried out utilizing the Shapiro-Wilk, Mann-Whitney, Wilcoxon and unpaired t tests (SPSS 15.0, SPSS Inc., Chicago, IL, USA). Results: Baseline parameters were similar between the two groups except for greater median age (72.8 vs. 69.2 years, p = 0.01) and lower median PSA (2.0 vs. 3.3, p = 0.01) in the 80 W group. Median laser time was longer in the 80W group (85 vs. 51 minutes, p < 0.001) with a higher median energy utilized (253 vs. 210 kJ, p = 0.001). Final IPSS, Qmax, PVR, and PSA were equivalent between the two groups. Conclusions: In our series, PVP was safe and effective. Durable and similar improvements in symptoms and objective parameters were achieved in patients with both 80 W and 120 W laser systems. PVP with the 120 W system, however, provided faster and more efficient vaporization compared to the 80 W system.
1. Introduction
Benign prostatic hyperplasia (BPH) represents a leading cause of bladder outlet obstruction in men over the age of 50, with an incidence in more than half of the male population [1]. The gold standard for treatment of BPH consists of transurethral resection of the prostate (TURP), an electrocautery based technique to remove excess prostatic tissue [2,3]. Although effective, it is however also associated with a significant risk of surgical complications and side effects [3-6], particularly TUR syndrome or dilutional hyponatremia, which is caused by the systemic absorption of hypotonic irrigant [6]. These risks are particularly increased with a large gland (greater than 45 g) or if the surgical time is excessively long [3]. TURP also carries a significant risk of intraand postoperative bleeding, leading to the possibility of inadequate resection [6].
In light of these complications, other minimally invasive therapies to treat BPH have emerged. One such therapy is photoselective vaporization of the prostate (PVP). This technique utilizes the Greenlight™ potassium-titanyl-phosphate (KTP) 532 nm laser (American Medical Systems, Minnetonka, MN) to vaporize and remove obstructive prostate tissue. This technique has been shown to result in comparatively fewer complications, e.g. reduced incidence of TUR syndrome as well as bleeding [7-15], Improvements to the Greenlight™ laser system have been made over time, particularly with the introduction of the 120 W HPS system in 2006. Few however have compared the clinical performance of the newer systems with their predecessors. In this study, we sought to examine the clinical performance of the 80 W vs. 120 W Greenlight™ laser systems for PVP.
2. Materials and Methods
After obtaining approval from the Institutional Review Board (IRB), a retrospective review was performed. Between September 2001 and May 2009 a series of 267 vs. 209 patients underwent PVP with the 80 W vs. 120 W GreenLight™ laser system (American Medical Systems, Inc., Minnetonka, MN) by a single surgeon (AET) at Weill Cornell Medical College. Data was collected on patient demographics, international prostate symptom score (IPSS), prostate-specific antigen (PSA) and perioperative parameters. Maximum flow rate (Qmax), postvoid residual (PVR) and prostate volume as determined by transrectal ultrasound, were recorded.
Patients in the study included males aged 50 years or greater, with moderate or severe LUTS, defined by an IPSS greater than 8 with significant bother, as well as a maximum flow rate (Qmax) of <10 mL/sec, with obstruction confirmed on urodynamics by a Bladder Outlet Obstruction Index (BOOi) of >40.
Intraoperative parameters collected included the number of laser fibers used, total amount of laser energy used, total procedural time, ASA score, and complications.
Patients were evaluated for follow-up at 1, 3, 6, and 12 months. At each of these visits, patients were evaluated for IPSS score, Qmax, and PVR. At 12 months, serum PSA was remeasured. Statistical analyses were carried out utilizing the Shapiro-Wilk, Mann-Whitney, Wilcoxon and unpaired t tests (SPSS 15.0, SPSS Inc., Chicago, IL, USA).
3. Results
A series of 267 and 209 patients qualified for 80 W and 120 W PVP respectively. Baseline parameters were similar between the two groups, except for a greater median age in the 80 W group (72.8 vs. 69.2 years, p = 0.01) and higher median PSA levels in the 120 W group (3.3 vs. 2.0, p = 0.01, see Table 1). Median laser time was longer in the 80 W group (90 vs. 51 minutes, p = 0.001, see Table 2) with a higher median energy utilized (253 vs. 210 kJ, p = 0.001) despite an equivalent prostate volume in both groups. A median of 2 fibers per procedure was used in both groups (p = 0.26). Median duration of follow-up was longer in the 80W group (25.4 vs. 16.6 months, p = 0.001). Data was available at 12 months and beyond for 162 and 108 patients, respectively.
Postoperatively, clinical improvements were observed in both groups (see Table 3, all p < 0.05 compared to baseline). IPSS scores improved in similar fashion by approximately 9 points in each group, as did QOL by 2 to 3 points in each group. Qmax increased by 3 to 4 mL/s in each group, while PVR decreased (96 vs. 52.5 mL and 61 vs. 30 mL in 80 W and 120 W groups, respectively) and PSA levels (2.0 vs. 1.40 ng/mL and 3.3 vs. 1.45
Table 1. Baseline patient characteristics.

Please note that mean are listed with SD, medians with IQR.
Table 2. Perioperative outcomes.

Please note that mean are listed with SD, medians with IQR.
Table 3. Postoperative patient outcomes.

Please note that mean are listed with SD, medians with IQR.
ng/mL, respectively) decreased in both groups. Final IPSS, Qmax, PVR and PSA were not statistically different between the two groups.
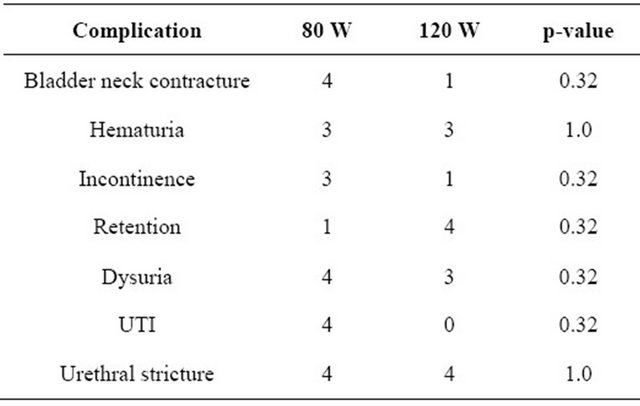
Complications were graded according to the modified Clavien classification and assessed at interval follow-ups (see Table 4) [16]. In the 80 W group, most complications were grade 1 in nature. The most common complications included urinary tract infection (UTI, n = 4), urgency/dysuria (n = 4), urethral stricture (n = 4), and bladder neck contracture (n = 4). In the 120 W group, most complications were also grade 1 in nature. The most common complications included transient urinary retention (n = 4), urethral stricture (n = 4), urgency/dysuria (n = 3), and transient hematuria (n = 3). No grade 4 or 5 complications occurred in either group. The rate of complications was statistically equivalent
Table 4. Postoperative complications (all between both groups (p = 0.32 to 1.0). No patients required blood transfusions postoperatively. 4. Discussion The gold standard intervention for the surgical treatment of BPH has been TURP. Although effective, the technique can be associated with significant complications, including TUR syndrome and bleeding [3-6]. Newer technologies such as PVP offer safer and equally effective alternatives to relieve symptomatic bladder outlet obstruction [7-15]. Few studies however have directly examined the clinical differences between 80 W vs. 120 W PVP [17]. In this study, we present and compare our experience with the 80 W and 120 W Greenlight™ platforms for PVP. PVP was found to be safe and effective at both 80 W and 120 W, with similar improvements in symptoms noted in both groups. Qmax increased to a similar extent, while PVR and PSA levels decreased in both groups. Of note, 120 W PVP did demonstrate a significant reduction in median lasing time (34 minutes) as well as energy utilization (43 kJ) compared to the 80 W counterpart (p = 0.001) despite an equivalent prostate volume in both groups. 120 W PVP was therefore more efficient than 80 W PVP in terms of time and energy despite using an equivalent number of laser fibers (n = 2, p = 0.26). Complication rates were low for both groups, demonstrating safety of the higher power technology. The study echoes the safety and efficacy of other studies examining the 120 W laser [18-22]. Lukacs, et al. reported on the REVAPRO study, the largest randomized controlled trial of a group of 139 patients undergoing 120 W PVP vs. monopolar TURP [22]. Although IPSS scores were not significantly different between the two groups at 12 months (6 vs. 5, respectively, p = 0.494), the study was not able to demonstrate noninferiority of PVP as originally intended. Nonetheless, length of stay was shorter in the PVP group (1 vs. 2.4 days, p < 0.0001). Qmax, PVR, and satisfaction and complication rates were comparable in both groups. Thangasamy, et al. recently reported on a meta-analysis of randomized trials of 80 W or 120 W PVP vs. TURP [15]. With 448 patients identified in nine trials, the PVP group demonstrated shorter catheterization time (−1.91 days, p < 0.00001) and length of stay (−2.13, p < 0.00001) although operative time was shorter with TURP by 19.64 minutes (p = 0.0003). Complication rates were equivalent between the two groups with the exception of a lower blood transfusion rate in the PVP group (p = 0.003). Of the nine studies, six showed no functional differences in terms of IPSS, Qmax, and PVR between PVP and TURP, two favored TURP, while one favored PVP. Nonrandomized studies have also assessed 120 W PVP. In the largest of these, Spaliviero, et al. evaluated 70 consecutive patients treated with the 120 W PVP [20]. At 12 months follow-up, stable and significant improvements in IPSS and Qmax were seen. Postoperative complications included delayed hematuria in 2 patients, short-term urinary retention in 2 patients, and UTI in 3 patients. Again, there were no other clinical studies directly comparing 80 W vs. 120 W PVP. Our study did possess several limitations. The first is that the data were collected in a retrospective fashion. The study also encompasses a high volume, tertiary care practice whose patient composition may not correlate with that seen in a community practice. The duration of follow-up is limited. The learning curve during the early PVP cases is also not taken into account. Results from this study need to be validated in a prospective, randomized fashion over a longer period of time. 5. Conclusion In our study, both 80 W and 120 W PVP techniques proved safe and effective for the treatment of BPH. Equivalent improvements in IPSS, QOL, Qmax, PVR and PSA levels occurred in both groups. However, 120 W PVP provided faster and more efficient vaporization compared to the 80 W system. REFERENCES NOTES *Denotes equal first co-authorship. #Corresponding author.