Advances in Breast Cancer Research
Vol.2 No.2(2013), Article ID:30474,4 pages DOI:10.4236/abcr.2013.22004
Breast Cancer Survivor’s Views on Duration of Follow Up*
Department of Surgery, Breast Surgery, Inverclyde Royal Hospital, Greater Glasgow and Clyde Health Board, Glasgow, UK
Email: jajadol@gmail.com
Copyright © 2013 Jasim Amin, Michael McKirdy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received December 5, 2012; revised January 7, 2013; accepted January 15, 2013
Keywords: Breast Cancer; Follow Up; Survivors; View; Clinic
ABSTRACT
Background: Breast cancer is one of the commonest cancers in women in the UK and western countries [1]. Follow ups after breast cancer diagnosis is usual practice, but there is no agreed consensus among breast care providers on frequency or duration of follow up after diagnosis and adjuvant treatment. The aim of this study is to find out women’s views on the period of the clinical follow up after breast cancer diagnosis. Method: This was a surveillance study in Greenock and Glasgow in the UK (Between September 2009 and December 2010). The study group comprised of 446 Women, 246 with the history of breast cancer diagnosed 1 - 10 years, (median 4.2 years) were asked to complete a questionnaire about their views of preferred duration of follow up while they were waiting for the annual review at a breast clinic, the same questionnaire was completed by 200 women with no history of breast cancer. Results: Between September 2009 and December 2010, 246 patients were included in the study. 40% of patients were within the first three years of follow up, 27% between the 4th and 6th year and 33% were in follow-up for more than 6 years. 63% of cancer survivors think that, 10 years of follow up is necessary for reassurance, detection and treatment of any new, recurrent or spread of their breast cancer. 14% and 22% of women with a history of breast cancer preferred 3 and 5 years review by trained Radiologist/GP respectively. Women without a history of breast cancer were different in their thoughts about follow up after breast cancer: 10%, 25%, and 30% chosen 10, 5 and 3 years, 35% preferred don’t know the answer. Conclusion: Follow up programs for breast cancer survivors need to be organized, evidence based, flexible and patient tailored. Patients’ views should be taken into account when considering provision of follow-up care for breast cancer patients.
1. Introduction
Breast cancer is the most common women cancer in the UK. There are an estimated 550,000 people living in the UK today who have been diagnosed with breast cancer. In 2008, there were 48,034 new cases of breast cancer diagnosed in the UK: 47,693 (>99%) in women and 341 (less than 1%) in men [1,2]. One woman in eight will be diagnosed with breast cancer in her lifetime, Around 12,000 women and 90 men will die from breast cancer each year. More people are surviving breast cancer than ever before, 80% of people with breast cancer are still alive five years after diagnosis. People are surviving longer due to advances in research, new treatments, earlier diagnosis, breast screening and breast cancer awareness, peak of recurrence is first three years but the risk continues beyond 10 years (approximately 80% of recurrences happen within 5 years) [1-3]. There is no solid consensus for follow up, different countries or units within the same country may have different programs: e.g. NICE recommends: two to three years follow up should be agreed by each network, while BASO guidelines suggest five years, and ASCO guidelines are more complex (review: every three to six months for the first three years after the first treatment, every six to 12 months for years four and five, and every year thereafter? And a mammogram one year after diagnosis, then every 6 to 12 months thereafter? Lifelong) [4-7]. In a systematic review of the literature, Montgomery, D.A. et al., revealed, among 1187 EBC with 7 years follow up 108 loco-regional, including 31 contralateral breast cancer, were detected in which only 14% were diagnosed in routine follow up clinic, 51% radiological, 12% symptomatic and 23% interval cancers presented with symptoms [8]. Every person treated for cancer is different. The recommendations are also different. The final decision is a doctor-patient agreement based on patient’s individual circumstances. The aim of this study is to demonstrate views of women with or without breast cancer in clinical follow up of survivors of breast cancer.
2. Methods
446 Eligible participants included in this study which was performed in Greenock and Glasgow in the UK (Between September 2009 and December 2010) Figure 1; group one 246 BC survivor women, 1 - 10 years after diagnosis, capable to give informed consent and completed their primary treatments. The second group were 200 women with no history of BC and able to give informed consent to contribute. They were handed out a preset print out of brief statistical facts and figures about breast cancer followed by a questionnaire on their views about duration of follow up (a choice of 3, 5 or 10 years of specialist Breast clinic review or by trained Radiologist/GP) after diagnosis and adjuvant treatment of BC. The first group also asked to record (age, date of BC diagnosis, type and side of surgery, adjuvant therapy and a family history of breast cancer). The second group reported their age, family history of breast cancer and had, don’t know answer, field in their print out. Data analysed using student’s t test, and chi test for categorical analysis.
3. Results
246 survivors completed the questionnaire while attending follow up clinic, median age 60 (range 35 - 88) years. Family history of BC reported by 54 women in this group. 123, 118 and 5 were diagnosed with left, right and bilateral BC respectively, Table 1. The second group were younger by 10 years, median age 50 (36 - 72) years. Only 10% of this cohort had a family history of breast cancer, Table 1.
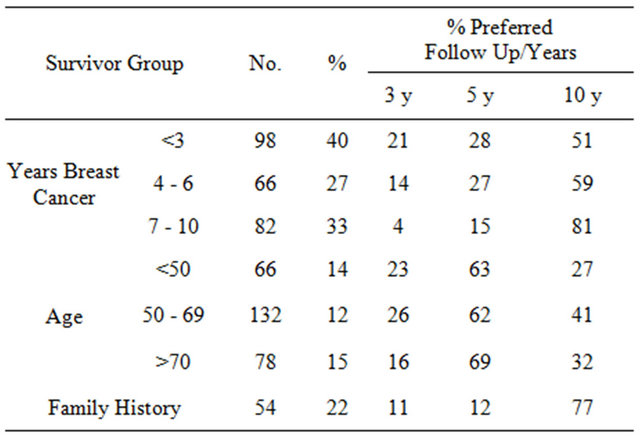
40% of clinic attendants were diagnosed in the last 3 years, and nearly half of them preferred 5 year or less of follow up. While long survivors (7 - 10 yr), surprisingly more in favour of 10 year follow up, 81%. On the other hand, those with a family history were very keen to continue to follow up for 10 yr, 77%, Table 2, Figure 1.
Younger survivors were slightly less fanatic of 10 year follow-up than older ones(63% vs 69%), Table 2, Figure 2. There was no significant effect of type of surgery,
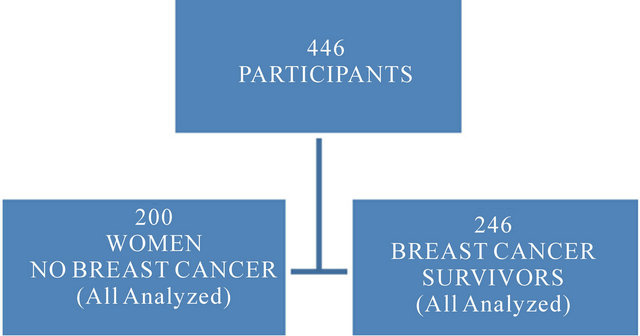
Figure 1. Flow chart.

Figure 2. Breast Ca duration and survivors views.
Table 1. Participant’s demographics.
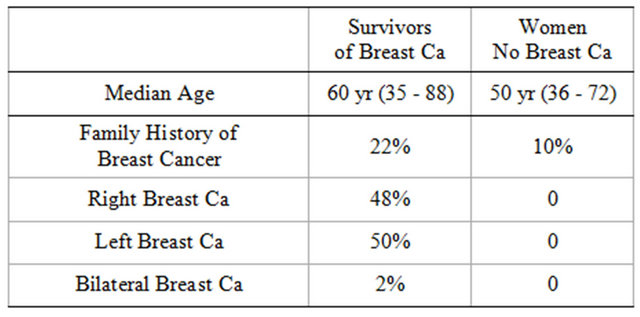
Table 2. Breast Ca survivors; years’ post breast Ca, age group and family history.
adjuvant therapy and side of BC on the results.
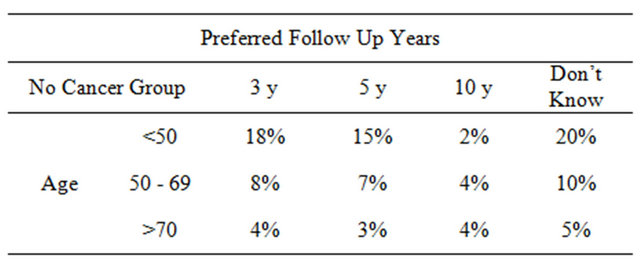
In the second group, one in three participants was unsure and voted don’t know. Family history of BC did not change their decision making, data not included. Generally this group was in favour of 3 or 5 year followup, 30% and 25%. Only 10% supported 10 years, Table 3, Figure 3.
4. Discussion
The aim of follow up after breast cancer diagnosis can be looked at in different angles, nice guide lines; is to

Figure 3. Age group and survivors with family history of breast cancer.
Table 3. No cancer group.
detect and treat local recurrence, deal with adverse effects of treatment and to provide psychological support. ASCO has similar view; the purpose of follow-up care for breast cancer is to help maintain good health after treatment, which includes coping with the side effects of treatment, reducing the risk of recurrence, and watching for signs of recurrence. Patients’ perceptions may be different; e.g. psychosocial support and reassurance [9-12]. At the same time, access to cancer expertise, the availability of diagnostic tests and specialist facilities are valued features of hospital follow-up [13,14]. Outpatient follow up can be a good area for audit and research [15]. However, Routine follow-up of patients operated for primary breast cancer is a very expensive service (£300 today in the UK) and there is no evidence that routine follow-up of mastectomised patients influences morbidity, mortality, or quality of life [16,17]. On the other hand, there is no solid evidence of improvement of cancer recurrence detection of clinical follow up; in a study by Donnely et al., 74% of recurrence were interval presentation and 19% radiological detected and 7% presented to clinicians with symptoms [17]. according to another study by Montgomery et al., only 15% of recurrences’ was detected during clinical follow ups [8].
Alternatives to the hospital clinic follow ups for BC survivors were around and tried in different ways; trained Radiologist, Oncologists, GPs, Nurse Specialist, group meeting, patient initiative, automated answering machines and telephone/questionnaire, with a good will and successful studies [8,18-21]. Participants of this study were BC survivors and ordinary women without BC history; their view was about the most common cancer among women and it is clear that they prefer to have a routine check-up with a preference of hospital review by approximately two thirds of survivors.
The limitations of this study are; being survey, it depends on the way that the questionnaire was set out, the timing of the survey, survivors were asked to give their view while waiting for follow up, this may influence decision making. The answer for the main question was a choice of (3, 5 or 10 years) no more or less?
We think that follow ups for survivors depend on patients circumstances and patients view needs to be taken into account for any future decision about the way these follow ups set out.
REFERENCES
- J. Ferlay, H. R. Shin, F. Bray, D. Forman, C. Mathers and D. M. Parkin, “Women and Cancer: Screening and Treatment Save Lives Estimates of Worldwide Burden of Cancer in 2008: GLOBOCAN 2008,” International Journal of Cancer, Vol. 127, No. 12, 2010, pp. 2893-2917. doi:10.1002/ijc.25516
- D. M. Parkin, S. L. Whelan, J. Ferlay, L. Teppoand and D. B. Thomas, “Cancer Incidence in Five Continents,” Vol. 8, IARC Scientific Publications No. 155, Lyons, 2003. Office for National Statistics, Series MB1 No. 39, National Statistics, London, 2010.
- Cancer Research UK, “Living Well beyond Breast Cancer: A Survivor’s Guide for When Treatment Ends and the Rest of Your Life Begins,” 2nd Edition, Three Rivers Press, Marisa and Ellen Weiss, 2010.
- R. L. Bowen, et al., “Early Onset of Breast Cancer in a Group of British Black Women,” British Journal of Cancer, Vol. 98, No. 2, 2008, pp. 277-281. doi:10.1038/sj.bjc.6604174
- J. Maddams, H. Moller and C. Devane, “Cancer Prevalence in the UK, 2008. Thames Cancer Registry and Macmillan Cancer Support,” 2008. http://www.thames-cancer-reg.org.uk/news/uk_prevalence_14072008.pdf
- S. Potter, S. Govindarajulu, M. Shere, F. Braddon, J. Turner, A. K. Sahu and S. J. Cawthorn, “Does Limiting Long-Term Follow-Up for Breast Cancer Allow All Referrals to Be Seen in 2 Weeks?” Annals of The Royal College of Surgeons of England, Vol. 90, No. 5, 2008, pp. 381-385. doi:10.1308/003588408X301181
- J. Jassem, M. Buchanan, F. Jänicke, M. Baum, L. Cataliotti, S. L. Kyriakides, M. Piccart, E. J. T. Rutgers and A. Costa, “The Hamburg Statement: The Partnership Driving the European Agenda on Breast Cancer,” European Journal of Cancer, Vol. 40, No. 12, 2004, pp. 1810- 1811. doi:10.1016/j.ejca.2004.04.020
- D. A. Montgomery, K. Krupa and T. G. Cooke, “Follow-Up in Breast Cancer: Does Routine Clinical Examination Improve Outcome? A Systematic Review of the Literature,” University Department of Surgery, Queen Elizabeth Building, Glasgow Royal Infirmary, Glasgow, 2007.
- M. Brennan, P. Butow, A. J. Spillane, M. Marven and F. M. Boyle, “Follow up after Breast Cancer—Views of Australian Women,” Australian Family Physician, Vol. 40, No. 5, 2011, pp. 311-316.
- S. Lawler, K. Spathonis, J. Masters and J. Adams, “Follow-Up Care after Breast Cancer Treatment: Experiences and Perceptions of Service Provision and Provider Interactions in Rural Australian Women,” Supportive Care in Cancer, Vol. 19, No. 12, 2011, pp. 1975-1982. doi:10.1007/s00520-010-1041-4
- M. Al-Gailani, P. Dudani, M. Fletcher, S. Beard and A Parkin, “Breast Cancer Follow-Up: What about the Patients’ Views?” European Journal of Surgical Oncology, Vol. 36, No. 11, 2010, p. 1119. doi:10.1016/j.ejso.2010.08.050
- K. Beaver, S. Williamson and K. Chalmers, “Telephone Follow-Up after Treatment for Breast Cancer: Views and Experiences of Patients and Specialist Breast Care Nurses,” Journal of Clinical Nursing, Vol. 19, No. 19-20, 2010, pp. 2916-2924. doi:10.1111/j.1365-2702.2010.03197.x
- E. Greimel, “Patients’ View of Routine Follow-Up after Breast Cancer Treatment,” 2011 ASCO Annual Meeting, 3-7 June 2011, Category: Patient and Survivor Care— Quality of Life Mgmt, Chicago, Article ID: e19516.
- F. M. Kew and K. Galaal, “Patients’ Views of Follow-Up after Treatment for Gynaecological Cancer,” Journal of Obstetrics & Gynaecology, Vol. 29, No. 2, 2009, pp. 135- 142. doi:10.1080/01443610802646801
- S. Morris, “What Are the Benefits of Routine Breast Cancer Follow-Up?” Postgraduate Medical Journal, Vol. 68, No. 805, 1992, pp. 904-907. doi:10.1136/pgmj.68.805.904
- K. Beaver, D. Tysver-Robinson and M. Campbell, “Comparing Hospital and Telephone Follow-Up after Treatment for Breast Cancer: Randomised Equivalence Trial,” British Medical Journal, Vol. 338, 2009, p. 337. doi:10.1136/bmj.a3147
- S. Carmel, “Breast Cancer Follow-Up: Literature Review and Discussion,” European Journal of Oncology Nursing, Vol. 11, No. 4, 2007, pp. 340-347.
- E. Grunfeld, “Primary Care Physicians and Oncologists Are Players on the Same Team,” American Society of Clinical Oncology, Vol. 26, No. 14, 2008, pp. 2246-2247.
- P. Donnelly, L. Hiller, S. Bathers and S. Bowden, “Questioning Specialists’ Attitudes to Breast Cancer Follow-Up in Primary Care,” Annals of Oncology, Vol. 18, No. 9, 2007, pp. 1467-1476.
- M. E. Del Giudice, E. Grunfeld and B. J. Harvey, “Primary Care Physicians’ Views of Routine Follow-Up Care of Cancer Survivors,” Journal of Clinical Oncology, Vol. 27, No. 20, 2009, pp. 3338-3345.
- M. Vanhuyse, P. Bedard, J. Sheiner, B. Fitzgerald and M. Clemons, “Transfer of Follow-Up Care to Family Physicians for Early-Stagebreast Cancer,” Clinical Oncology, Vol. 19, No. 3, 2007, pp. 172-176. doi:10.1016/j.clon.2007.01.115
NOTES
*The authors declare no conflict of interest.

