Open Journal of Veterinary Medicine
Vol.07 No.01(2017), Article ID:74512,7 pages
10.4236/ojvm.2017.71001
Case Report on Feline Polycythemia Vera
Corinna Beale
Division of Laboratory Animal Medicine, Tufts University, Boston, MA, USA

Copyright © 2017 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY 4.0).
http://creativecommons.org/licenses/by/4.0/



Received: October 5, 2016; Accepted: February 25, 2017; Published: February 28, 2017
ABSTRACT
Polycythemia vera has been reported as a known condition in cats as early as 1966. This condition manifests as an increased mass in red blood cells and ele- vated hematocrit and is defined as an idiopathic chronic myeloproliferative disorder. The patient described in this paper presented with hyperemic gums and pinna and an acute onset of progressive ataxia and lethargy. Several possible underlying primary conditions such as cardiac disease and renal malignancy were excluded by running basic blood work and radiographic imaging. Initial blood work revealed a significantly elevated packed cell volume (88%). After diagnosis, treatment with phlebotomy and chemotherapy lead to a redu- ction in hematocrit and elimination of neurologic signs. This case study repre- sents the diagnosis and successful management of this disease in a private pra- ctice setting. Polycythemia vera is relatively uncommon in dogs and cats, but should still be considered in cases of neurologic disorders, especially with the presence of bright red ears, paws, or gums.
Keywords:
Polycythemia Vera, Feline, Phlebotomy, Hydroxyurea

1. Introduction
Feline hematology is something that private practitioners commonly review as part of their daily clinical practice. A decreased red blood cell count, otherwise noted as anemia, is by far the most commonly noted red blood cell count abnormality or irregularity seen on feline hematology. The list of potential rule outs for anemia is widespread and includes diseases, disorders, and infections of nearly every body system. Conversely, an increased red blood cell count, otherwise noted as polycythemia vera is significantly less common. Known causes of this condition are exceptionally limited. Rule outs for polycythemia vera include primary polycythemia (aka idiopathic) and secondary polycythemia caused by heart disease or erythropoietin (EPO) producing renal tumor. The limited lists of causes for this disorder make the diagnosis relatively simple. While an absolute cure for this disease has yet to be discovered, management and treatment of this condition has a rewardingly high success rate.
2. Case Presentation
A four-year-old, 4.4 kg, neutered, male, indoor-only, domestic-short-hair cat presented to the Revere Pet Clinic with a progressive six-day history of lethargy, ataxia, and inappropriate mentation.
Three days prior to arriving at the Revere Pet Clinic the patient had been seen at a local emergency hospital for lethargy and ataxia. The patient had a history of two urinary tract infections, was not up-to-date on vaccines, was FIV/Felv negative as a kitten, and the owner had one other healthy cat at home.
Physiologic parameters (heart rate, temperature, respiratory rate, and capillary refill time) were all within normal limits. A neurologic consult revealed tetra- ataxia (most pronounced in the hind limbs), lack of menace, and otherwise normal reflexes and proprioception. Due to financial constraints the owner could not afford a further work-up at the referral hospital. In the absence of further consent to diagnostics, the neurologist prescribed Clindamycin to rule out infectious causes (toxoplasmosis) and recommended starting steroids if no improvement was seen on this medication.
On arrival at the Revere Pet Clinic, the cat’s tetra-ataxia was still present and had progressed to partial paresis in the hind legs. The patient was twitching occasionally and acting lethargic with no appetite. A thorough physical exam was performed. In addition to the neurological signs, pertinent findings on physical exam included hyperemic gums, and erythema on ears and paw pads. All other physical exam findings were unremarkable. Initial diagnostics included an in- house blood glucose (49), in-house FIV-FelV test (both negative), and a complete blood count (CBC) and biochemistry panel was sent to Idexx Laboratories, Inc. (North Grafton, MA). The patient was sent home to wait for blood work diagnostics with a guarded prognosis.
The CBC revealed a polycythemia with a mild leucopenia (Table 1). Total protein and albumin were within normal limits. The biochemistry panel reflected normal total protein and albumin with a slight elevation in GGT (Table 2). A cytology review confirmed the polycythemia and found no significant abnormalities in the erythrocytes, white blood cells (WBC), or platelets. Radiographs were recommended to check for evidence of secondary causes of polycythemia such as hypoxia secondary to heart or lung disease, or an erythropoietin producing renal tumor. Twenty-four hours after initial presentation to the clinic, a three-view series of full body radiographs revealed no abnormalities in the thorax or abdomen.
Overnight the cat’s neurological state continued to deteriorate. The patient had two seizures, five hours apart. His neurological signs had progressed to complete hind limb paralysis/weakness, and constant facial and limb twitching were noted. He had not eaten anything and the owner had syringed some water into his mouth in an attempt to hydrate him. An in-house packed cell volume (PCV) was 88%.
The cat was immediately prepped for phlebotomy. The skin over the cephalic and left jugular veins was shaved and sterilely prepped. A standard intravenous (IV) catheter was placed in the cephalic vein. A twenty-one-gauge butterfly catheter was flushed with heparin and saline solution and placed in the jugular vein. 82 mls were removed via a 25 cc syringe and three-way stop cock. Immediately following the phlebotomy, 120 mls of lactated ringer’s solution (LRS) was given through the cephalic IV catheter over a one-hour period.
An hour after phlebotomy and immediately after administering IV fluids, the patient’s PCV had dropped to 71%. The cat’s mentation had already improved and he was sitting up and looking around. No tremors or twitching were noted. He was able to stand and walk back into his carrier although marked hind-leg weakness was noted. The cat was sent home with instructions on how to give subcutaneous fluids daily (150 mls LRS/day).
The cat spent a week on daily subcutaneous fluids. One week after the initial phlebotomy occasional twitching was noted and a second phlebotomy was performed (starting PCV 77%, 75 mls of blood extracted and replaced with saline.
Table 1. Comprehensive Complete Blood Count.
WBC (White Blood Cell); RBC (Red Blood Cell); HGB (Hemoglobin); HCT (Hematocrit); MCV (Mean Corpuscular Volume); MCH (Mean Corpuscular hemoglobin); MCHC (Mean Corpuscular Hemoglobin Concentrations). Platelet Comments: Scanning of the blood smear revealed adequate platelet numbers. Due to clumping and/or large platelets the automated platelet number cannot be accurately determined. Remarks: Slide reviewed microscopically. WBC and RBC morphology appears normal.
Table 2. Blood Chemistry Analysis.
Test Result Reference Range Low Normal Hig: ALP (Alkaline Phosphatase); ALT (Alanine Transaminase); AST (Aspartate Aminotransferase); GGT (Gamma-Glutamyl Transpeptidase); BUN (Blood Urea Nitrogen).
Post phlebotomy PCV was 62%). The cat was started on hydroxyurea at 125 mg every other day for two weeks. One-week post treatment the PCV was 65%. The hydroxyurea was continued at every other day for an additional week and recheck PCV a week later was 61% with no clinical signs (no twitching, seizures, or other neurologic signs with a normal appetite and disposition). The cat was then weaned onto a maintenance dose of hydroxyurea at 250 mg twice weekly. The hydroxyurea was compounded and given by mouth as a liquid. The cat seemed lethargic after the recommended 250 mg dose, so the owner elected to give 160 mg 3 times per week as maintenance. No lethargy was noted at this dose and fre- quency.
Long term treatment plan consisted of weekly PCV checks, and CBC and biochemistry panels run every three months to monitor WBC count for myelosuppression and recurrence of polycythemia. After three months of stabilization, CBC and chemistry checks were run 3 - 4 times a year to monitor. Two years la- ter the cat continued to do well with no episodes of twitching or seizure. The cat still had occasional minor hind leg weakness, and retained the hyperemic mucus membranes, and erythematous pinnae and paws. Anecdotally, he is one of the nicest cats the prescribing veterinarian has encountered.
3. Discussion
Polycythemia vera is relatively uncommon in small animal practice [1] , but should still be considered in cases of neurologic disorders, especially with the presence of bright red ears, paws, or gums [2] . Due to the vascular effects of the disease such as decreased oxygen transport and obstructed blood flow, atypical cases may present first with secondary symptoms such as uveitis [3] . It has been reported as a known condition in cats as early as 1966 [3] . Once treated, this di- sease has a relatively good prognosis [4] . This case study represents successful management of this disease in a private practice setting.
True or absolute polycythemia is suspected when there is an elevated PCV in the absence of dehydration. If dehydration is present, then a relative polycythemia must be considered. Breed specific elevations in PCV (e.g., Greyhounds) must also be considered [4] .
Diagnosing of primary vs. secondary polycythemia vera can be slightly challenging. Radiographs, ultrasound, and blood gases can be used to rule-out secondary polycythemia due to underlying heart disease [5] , or erythropoietin (EPO)-producing kidney tumor. Checking EPO blood levels has limited diagnostic use since the concentrations in polycythemic patients may overlap with normal levels and there is a lack of species specific assays in the dog and cat [6] .
Primary polycythemia or polycythemia vera manifests as an overproduction of normal red blood cells within the bone marrow. This malignant clone of red blood cells exists despite normal or even low levels of erythropoietin. Some alternative theories behind the etiology of this disorder suggest that the condition exists due to a hypersensitivity to EPO rather than a malignant cell population within the marrow [7] .
In most cases of polycythemia vera, the condition is not diagnosed until clinical signs have become severe. The increasing number of clinics with in-house blood screening abilities has made general health screening of blood work both more affordable and more common. Regular blood screening tests at wellness visits will likely increase the incidence of diagnosing this disease earlier before clinical signs become evident. The clinical signs most commonly noted by owners and veterinarians are due to the hyperviscosity of the blood which causes a decreased cerebral perfusion and leads to such symptoms as blindness, ataxia, or seizures. Phlebotomy is the fastest and most effective way to decrease the PCV and resolve the patient’s neurological signs [7] . Several different calculators can be used to determine how much blood to remove. In the example case, the following formula was used [8] :
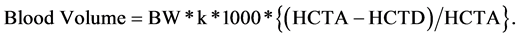
BW = Body wt in kg, K = 0.09 for dogs, 0.07 for cats, HCTA = actual HCT, and HCTD = desired HCT.
No more than 20 mL/kg per day with a goal of a PCV of less than 60%.
In the case example, heart disease or a malignant kidney tumor could not be completely ruled out based on radiographs and clinical signs alone. However, the blood work and radiographic evidence were presumed significant enough to proceed with treatment options for polycythemia vera considering the owner’s financial constraints and limited ability to pursue further diagnostic workup. If money were no concern, additional diagnostics may have included an arterial blood gas, abdominal ultrasound, and possible EPO level (less diagnostically valuable, i.e. results will be inconclusive). Notably, bone marrow biopsy cannot distinguish primary from secondary polycythemia and is not considered a useful test for this condition [7] .
4. Conclusion
This case represents the successful diagnosis and treatment of a polycythemic cat in a general practice setting. In rare cases, polycythemia patients may spontaneously regress so a follow up is important [9] . Side effects of long term use of the chemotherapeutic agent hydroxyurea are usually reversible and can include bone marrow suppression, hair loss, and gastrointestinal upset [7] . If a patient has an adverse reaction to the hydroxyurea, alternative methods of treatment include serial phlebotomies, other chemotherapy drugs or the less conventional medical grade leeches [10] . Since evidence of this disorder can be seen on basic blood work, this disease represents one example of the potential benefits for regular blood work screenings at annual appointments [11] .
Acknowledgements
Many thanks to Dr. Olga Iglikova for providing exceptional mentorship and support on numerous cases and patients and for her dedication to improvement and excellence in small animal veterinary medicine.
Cite this paper
Beale, C. (2017) Case Report on Feline Polycythemia Vera. Open Journal of Veterinary Medicine, 7, 1-7. https://doi.org/10.4236/ojvm.2017.71001
References
- 1. Evan, L.M. and Caylor, K.B. (1995) Polycythemia Vera in a Cat and Management with Hydroxyurea. Journal of the American Animal Hospital Association, 31, 424-438.
https://doi.org/10.5326/15473317-31-5-434 - 2. Quesnel, A.D., Parent, J.M. and McDonell, W. (1997) Diagnostic Evaluation of Cats with Seizure Disorders: 30 Cases. Journal of American Veterinary Medical Association, 210, 65-71.
- 3. Gray, H.E., Weigand, C.M., Cottrill, N.B., Willis, M.A. and Morgan, R.V. (2003) Polycythemia Vera in a Dog Presenting with Uveitis. Journal of the American Animal Hospital Association, 39, 355-360.
https://doi.org/10.5326/0390355 - 4. Ettinger, S.J. and Feldman, E.C. (2005) Textbook of Veterinary Internal Medicine. 6th Edition, Elsevier Inc., St. Louis.
- 5. Groulade, P. and Guilllon, J.C. (1966) Erythremic Syndrome in Cats. Bulletin de L’Academie Verinaire de France, 39, 127-131.
- 6. Randolph, J.F. (2013) The Merck Veterinary Manual Overview of Erythrocytosis and Polycythemia.
http://www.merckvetmanual.com/mvm/circulatory_system/erythrocytosis_and_Polycythemia/overview_of_erythrocytosis_and_Polycythemia.html - 7. Foster, E.S. and Lothrop Jr., C.D. (1988) Polycythemia Vera in a Cat with Cardiac Hypertrophy. Journal of American Veterinary Medical Association, 192, 1736-1738.
- 8. Cook, S.M. and Lothrop Jr., C.D. (1994) Serum Erythropoietin Concentrations Measured by Radioimmunoassay in Normal, Polycythemic, and Anemic Dogs and Cats. Journal of Veterinary Internal Medicine, 8, 18-25.
https://doi.org/10.1111/j.1939-1676.1994.tb03191.x - 9. Hell, L. (1992) Polycythemia. Clinical Resources: Canine Associate Database.
http://www.vin.com/Members/Associate/Associate.plx?DiseaseId=1292 - 10. Cowan, D.H., Messner, H.A., Jamal, N., Aya, M.T. and Smiley, R.K. (1994) Spontaneous Remission of Polycythemia Vera: Clinical and Cell Culture Characteristics. American Journal of Hematology, 46, 54-56.
https://doi.org/10.1002/ajh.2830460110 - 11. Nett, C.S., Arnold, P. and Glaus, T.M. (2001) Leeching as Initial Treatment in a Cat with Polycythaemia Vera. Journal of Small Animal Practitioners, 42, 554-556.
https://doi.org/10.1111/j.1748-5827.2001.tb06027.x


