Open Journal of Medical Psychology
Vol.3 No.1(2014), Article ID:40989,17 pages DOI:10.4236/ojmp.2014.31001
Comparing Women and Men’s Experiences with Kallmann Syndrome
1Institut und Poliklinik für Sexualforschung und Forensische Psychiatrie, Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany
2Universität Osnabrück, Fachbereich Humanwissenschaften, Institut für Psychologie, Osnabrück, GermanyEmail: *hrichter@uke.de
Copyright © 2014 Johannes Hofmann et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In accordance of the Creative Commons Attribution License all Copyrights © 2014 are reserved for SCIRP and the owner of the intellectual property Johannes Hofmann et al. All Copyright © 2014 are guarded by law and by SCIRP as a guardian.
Received October 24, 2013; revised November 24, 2013; accepted December 2, 2013
Keywords:Kallmann Syndrome; Hypergonadotropic Hypogonadism; Hormone Disorder; Delayed Puberty; Pubertal Development
ABSTRACT
Topic: Kallmann syndrome (KS) is a congenital olfacto-genital disease. Affected persons show an absence of physical pubertal development, and their sense of smell is reduced or absent (anosmia). The prevalence is 1:40,000 in women and 1:8000 to 1:10,000 in men. Development of gender identity corresponds to the assigned gender at birth. The cause of KS is a genetic defect. To date, only a few systematic investigations have delved into the psychological disstress and consequences of the somatic characteristics of KS. In order for affected persons to be appropriately informed, well-founded research results are necessary. The focus of the present study aims at examining the similarities and differences between the psychological disstress and consequences women and men experience through the development, on the one hand, and through its medical treatment on the other. The present text complements current findings on the psychological consequences of KS in men [1] and women, respectively [2]. Two questions lie at the center of the comparison: 1) Which similarities and which gender-specific differences are there concerning the perceived burdens? 2) Which coping strategies have been developed in dealing with the burdens and consequences caused by KS in the affected women and men? Which similarities and which gender-specific differences are there with respect to these coping strategies? Methodology: The survey has been carried out by means of topically focused narrative interviews of 16 men and 5 women. Based on the qualitative content analysis according to Mayring [3], categories have been generated and evaluated on the basis of the interview material. The results of the male and female samples have been contrasted and analyzed in gender-specific relevant key subjects [1,2]. Results: The comparison shows that the burdens women and men experience through KS go beyond the somato-medical problems, and that the psychosocial consequences are a heavy burden for the members of both groups. Men bear a heavier burden through insecurities and shame about the absence of virilization and subsequently suffer more from bullying and marginalization experiences. They also perceive mood changes more frequently and as more burdensome through the course of hormone treatment. Women also develop shame due to the absence of female body development; they do, however, perceive this as less burdensome than do men. They suffer particularly from a loss of libido before and also during hormone treatment. Differences occur concerning the gender-specific hormone treatment and its effects on mood and libido. Wellfounded statements relating to this do, however, require further-reaching studies. In women, KS is frequently misdiagnosed as simply estrogen deficiency, which could be an explanation for the differing degree of prevalence. The preferred coping strategies for both sexes include confidential talks with suitable people, such as parents, the partner, friends, or a psychotherapist. Using support from psychotherapists, sex education, and/or sexual therapists is recommended when necessary. Conclusion: Psychotherapeutic/psychological support is recommended for both women and men diagnosed with KS, taking into account the gender-specific differences in dealing with the burdens KS imposes. The focus for both sexes should be on developing and strengthening body image and self-esteem. In medical treatment for both women and men, normal or inconspicuous body development should be emphasized. Particularly in the case of women, sex therapy should be available for support due to loss of libido. For men, therapy should be recommended, so as to strengthen their social capabilities and self-confidence. Additional studies are necessary for examining the effects of hormonal treatment on mood and libido and phenotyp.
1. Introduction and State of Research
KS belongs to the clinical picture of hypogonadotropic hypogonadism (HH) [4,5]. The production of sex hormones that normally leads to the initiation of physical pubertal development is absent through a congenital genetic defect [4,5]. The sense of smell is limited (hyposmia) or totally absent (anosmia) among persons affected with KS, whereby KS distinguishes itself from other forms of HH [6-8]. Moreover, affected persons are frequently affected by osteoporosis through the lack of testosterone (among men) or through the lack of estrogen (among women) [8,9]. Among women, the prevalence of KS is 1:40,000 [6], among men, 1:8000 to 1:10,000) [10]. Individuals are treated by supplementation of the sexual hormones that are lacking [11].
1.1. Physical Symptoms of Kallmann Syndrome among Women
The absence of pubertal development among women with KS is caused by a disorder of estrogen production [4,5]. Due to a dysfunction of female ovaries, affected women have low GnRH-values (Gonadotropin releasing hormone) in their blood and as a consequence, low LHvalues (luteinizing hormone) and FSH-values (folliclestimulating hormone) [12,14].
The physical effects of the lack of estrogen in KS-affected women are insufficiently developed secondary sex characteristics [8,12]. Impaired body development in women during puberty includes lack of menstruation (primary amenorrhoea, which can be found in 90% of women with HH) [11]; absent breast development [8,13]; small ovaries [12,14]; no development of gametes, and no follicle genesis [13]; and infertility [15]. The growth of normal pubic hair is induced through the hormones of the adrenal gland; this, however, may also be absent due to the lack of estrogen [8,16]. In addition, vaginal dryness may accompany the endocrine disorder, and sexual intercourse is frequently perceived as painful and unpleasant by the affected women. Sexual desire is mostly low among these women, and as a consequence they have very few sexual contacts [15].
The absent estrogen is substituted among the affected women, first of all in low doses with 1mg estradiol, later increasing [8,11,16]. In the second treatment year, estradiol is administered together with chlormadione acetate [11,16]. For women wishing to become pregnant, GhRh is administered in order to stimulate the production of LH and FSH. Chances of success for this kind of treatment are regarded as good [14]. Alternatively, LH or FSH can be administered directly [8,14].
Due to the lack of a sense of smell, KS can be assumed and diagnosed in pre-puberty [11]. By means of an odor test, KS can be distinguished from Pubertas tarda and other forms of HH [8,16]. If breast development in girls has not yet started at the age of 14.5 years, a medical examination is recommended [16]. KS is diagnosed through an examination of the development of secondary sex characteristics, through an examination of blood values of LH, FSH, PBI (protein-bound iodine), and estradol, through cranial CTs or cranial MRTs, and by examining the family history [11,16].
1.2. Physical Symptoms of KS among Men
KS-affected men lack the following physical developments at puberty: penis growth, the growth of testicles and muscles, pubic hair, axillary hair, and beard growth as well as voice break [17]. In addition, sperm agenesis is not initiated [17], and potency and libido are low for the affected men [9,18-20]. Through substituting the testosterone that is lacking, pubertal body development can be initiated [11,20]. The treatment is carried out analogous to the treatment for Pubertas tarda, through the intake of 50 mg of testosterone enanthate every four weeks [11], increased to as much as 250 mg of T-enanthate every four weeks over a period of several years [11]. In the case of an early diagnosis, the therapy should start between the age of 12 and 13 [11]. Alternatively to the T-enanthate treatment, affected men may be given subcutaneous hCG (human chorion gonadotropin) and rhFSH (recombinant human follicle-stimulating hormone) or pulsatil GnRH (gonadotropin-releasing hormone). The therapy is changed to an estostrone substitution for men who wish to father a child [11].
KS is diagnosed by examining the development of secondary sex characteristics, by examining blood values of LH, FSH, testosterone, GnRH, and hCG, through cranial CTs or cranial MRTs, and through an examination of the family history. KS may be suspected early on where there is a poor sense of smell or total anosmia [11].
1.3. Psychological Accompaniment of Kallmann Syndrome
Medical research primarily concentrates on the somatic aspects of KS. Studies of the physical symptoms and individual case reports suggest that psychological and psycho-social burdens are present for the affected men and women due to the lack of testosterone or estrogen and the resulting absence of physical pubertal development [18,19,21-24]. If psychological problems such as depression occur within the treatment, an increase of hormone substitution is recommended as per the treatment guidelines of the German Society for Pediatrics and Adolescent Medicine. Psychotherapeutic treatment should be added, if necessary [11].
Medical reports on KS do not address the development of gender identity. Merely two case descriptions in which men affected by KS, experienced atypical development of gender identity despite testosterone substitution can be found in the literature [25]. Thus, as a rule, undisturbed development of gender identity in the affected men and women can be assumed.
1.4. Psychological Impairments of Kallmann Syndrome among Women
Girls with a diagnosis of KS are described as feeling “shocked”, “confused”, and “devastated”. As a reason, fear of infertility and fear of stigmatization through the disease are mentioned ([15], p. 2). Those affected may develop insecurely and with restraint [15], since the difficulties of absent physical maturation cause “psychological conflict situations” in children and adolescents ([21], p. 633). Usually, the low libido strongly restricts affected women in their sexuality, leading to severe psychosexual strains [15]. The importance of well-coordinated hormonal treatment and, if necessary, sex therapy, have to be emphasized in such cases [15].
1.5. Psychological Consequences of Kallmann Syndrome among Men
Besides the physical symptoms described above, men affected by the lack of testosterone show the following psychological symptoms: depressive mood and mood changes, decrease of their general activity, lack of motivation, listlessness, and decreasing muscle power [9,18, 19,21].
Investigations have shown that the affected men experience insecurities, problems with self-esteem, and social marginalization as a consequence of absent physical development [19,22,23,26,27]. The insecurities and self-esteem problems result from a range of issues that include bullying and marginalization by peers due to the lack of virilization, as well as feelings of shame concerning their own bodies [23]. Han and Bouloux [18] point out that it is difficult for those affected to enter sexual relationships because of these lack of assertiveness. Furthermore, they state that those affected have difficulties in dealing with their newly “awakened” sexuality after a successful hormone treatment. In this context they simultaneously develop the feeling of having missed out on something. Negative sexual experiences and selfdoubts [19] may lead to problems with their psychic and sexual development. In these cases, support by psychotherapists or sex therapists is recommended [18].
1.6. Research Question
The previous research results, as well as the results from the research project of the University Clinic of Hamburg-Eppendorf by Hofmann, Watzlawik, and RichterAppelt [1,2] reveal the following: KS affects both women and men far more than only on a purely somatic medical level, and requires a holistic perspective. For this reason, the psychosocial aspects of KS should be perceived as severely limiting quality of life, and must be taken into account when informing affected men and women about KS, as well as during treatment of KS.
In the medical literature, there are hints of the differences between KS-affected men and women with regards to physical symptoms and psychological consequences. In order to find adequate gender-specific (therapeutic) support methods, it is of particular importance to identify and understand the gender-specific burdens and conesquences for affected women and men.
The central questions by which this research project contributes to this objective are as follows:
1) What are the differences in mental stress and its consequences due to KS among the affected men and women?
2) What are the similarities in mental stress and its consequences due to KS among the affected men and women?
3) What are the similarities and differences in coping strategies among the KS-affected men and women?
2. Methodology
The present investigation has been carried out within the research project at the University Hospital, HamburgEppendorf, on the psychological consequences of KS. The project has been approved by the ethics commission of the Chamber of Psychotherapists, Hamburg. Publication of the individual gender-specific evaluations of the empirical data subject to this comparing analysis is currently being prepared [1,2]. To ensure a thorough exploration of the field, a qualitative and quantitative1 research approach has been used, and data have been collected by means of surveys. Items on demographic questions, body feeling and body development, diagnosis and treatment, sexuality and puberty experience have been employed in the quantitative data collection. In addition, the following standardized questionnaires have been used: a questionnaire on gender identity, Bem Sex-Role-Inventory, questionnaire to assess the own body (Fbek), Brief Smptom Inventory (BSI), dissociation questionnaire (DIS-Q), and a questionnaire on life satisfaction (FLZ). The results of the quantitative study are being prepared for publication. The illustrations and tables have been taken from the publications on gender-specific investigations [1,2].
2.1. Collection of Participants
For the purpose of canvassing affected men and women as interview partners, doctors registered on a national level as well as doctors in local clinics in the subject areas of endocrinology, gynecology, urology, and reproductive medicine were informed about the project. At the same time, self-help groups, Internet pages and newsgroups on the topics of KS, hypogonadism, desire for children, and endocrinology were used as a source of canvassing [1,2]. Three women and nine men were located via the Internet as interview partners. Two women and five men participated in the survey on the recommendation of their doctors; two of the included men were referred to the investigation by family members and friends.
2.2. Implementation
The interview technique chosen was particularly suited to collecting and structuring the individual experiences of those affected, to stimulating the narrative flow, to creating generous space for notes, and to allow topically focused immersions [28]. The interviews were carried out along the design of a concept-map—a “map” complied on the basis of research results on catchwords pertaining to KS (see Chart 1) [1]. This concept-map led the interview partners through the topic areas on a common thread. The interview technique permitted unrestricted frank replies by the participants to the questions they were asked, a very personal description of their results and experiences, and thematization, emphasis, and deepening of subject-relevant aspects [29,30].
All thematic priorities were taken up by the participants almost exclusively without request, which indicates that the thematic priorities of the concept-map are largely consistent with the participants’ experiences. Also, questions have been asked to structure the interview when necessary, and to enlarge upon certain relevant topics from the literature research. The interviews were conducted in suitable rooms of public buildings or at the participants homes and took between 41 and 203 minutes (range: 162 min, average value of the duration: 74.5 min). They were co-written and transcribed according to LuciusHoene and Deppermann [31].
2.3. Sample Description
The interviews were carried out from January 2009 to March 2010. Five women and 16 men were interviewed within the study. The prevalence of KS is also mirrored in the fact that considerably fewer women volunteered for participation in the study. The results of both studies will be compared under explorative features, which is why the possible limitations do not carry weight through the diverging sample sizes. Average age and standard deviation have been calculated for both sexes. The mean age of participating women was 30.8 (SD 7,30), while the mean age for men was 40.48. (SD 12,47) All participants were high-school graduates. A list of detailed data can be found in Table 1.
At 40.48 years, the average age of men participants was significantly higher than that of women. Detailed data can be found in Table 2.
2.4. Evaluation
The interview data have been evaluated as per the qualitative content analysis according to Mayring [3] and with the help of the evaluation programme MAXQDA 10 (MAX Qualitative Data Analysis). Interview sequences have been assigned to categories, which have been
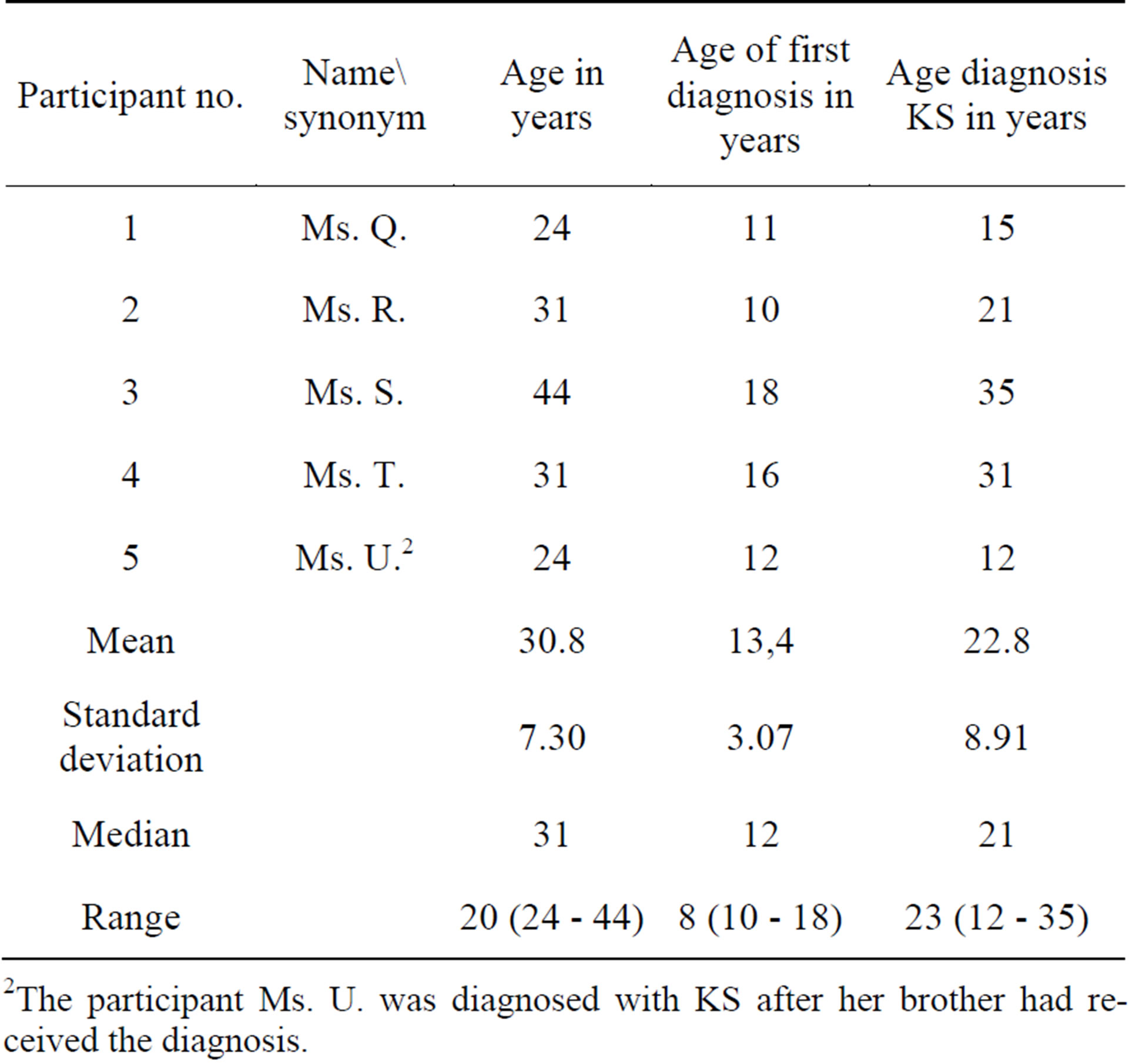
Table 1. Female participant’s age and age at diagnosis at the time of questioning.
2The participant Ms. U. was diagnosed with KS after her brother had received the diagnosis.
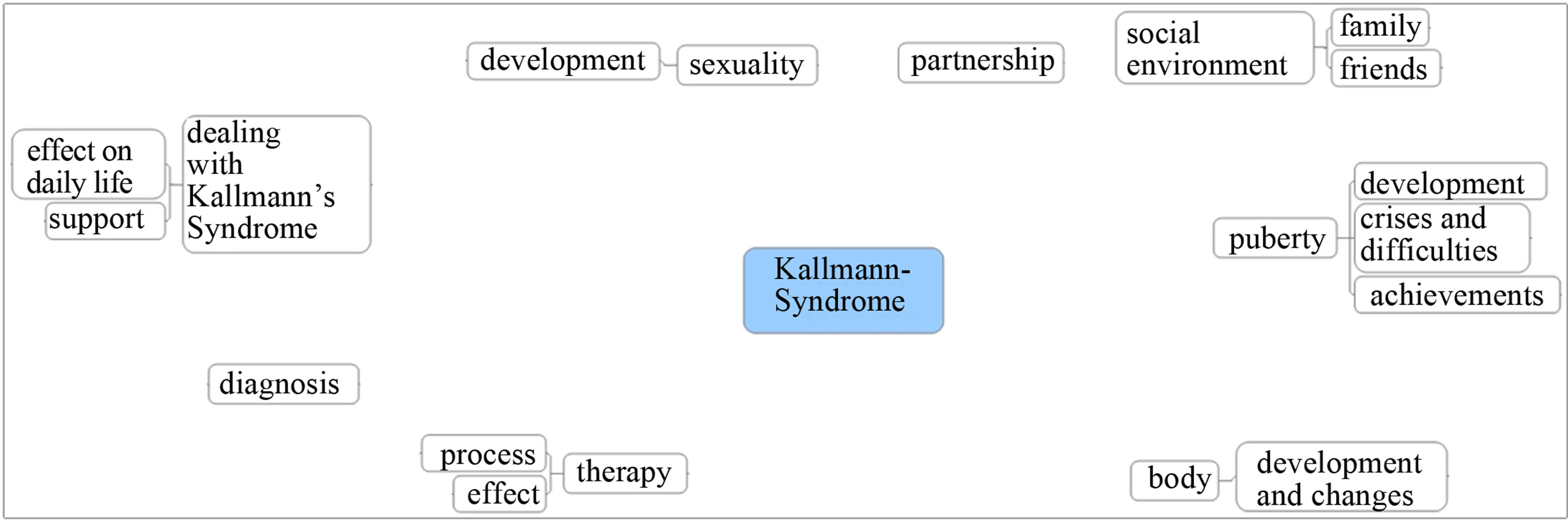
Chart 1. Concept-map.
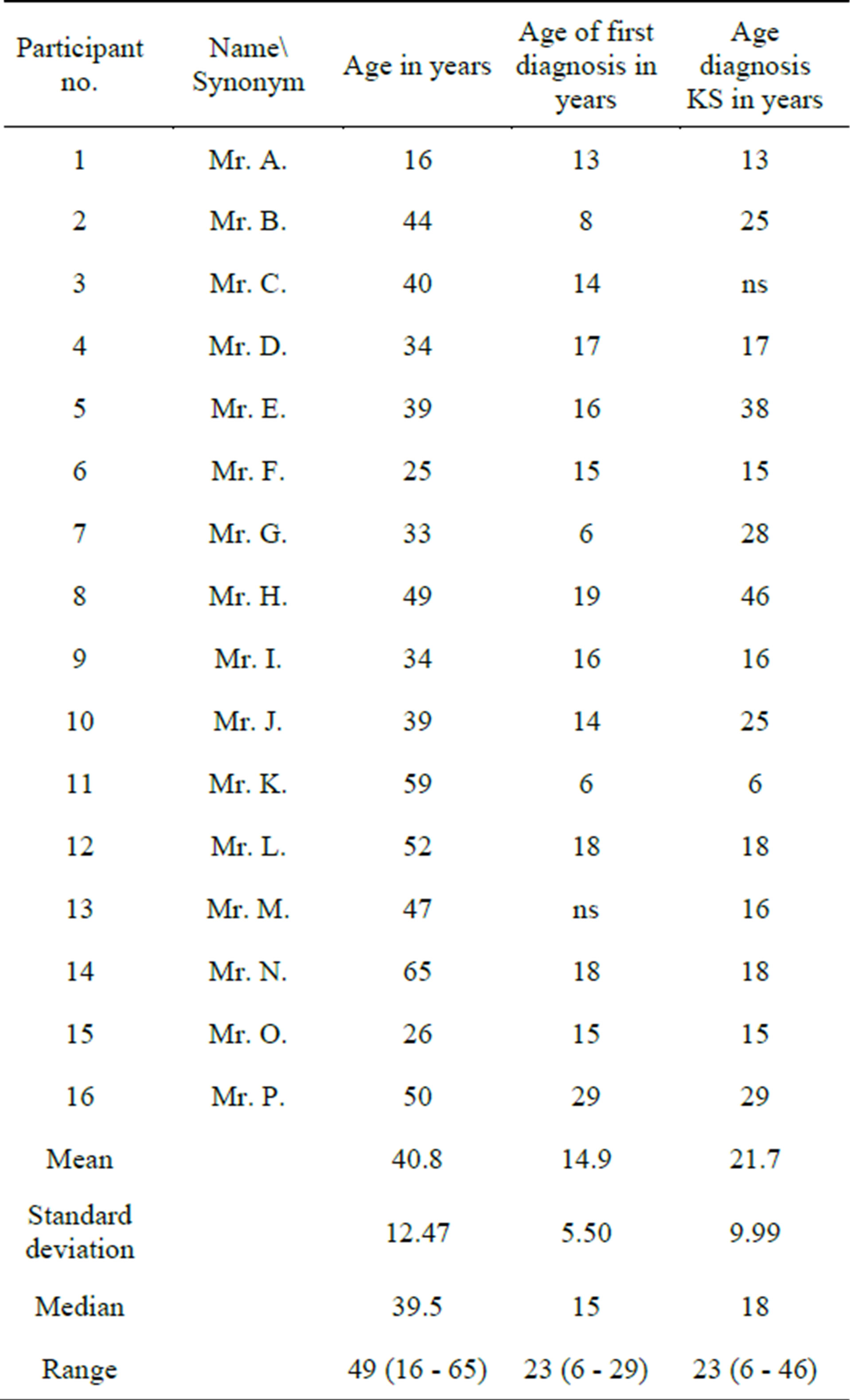
Table 2. Male participant’s age and age at diagnosis at the time of questioning.
worked out of the central research concepts and the central questions of the interviews (see Chart 1, conceptmap) or from the topics newly addressed in the interviews. In doing so, the researchers adhered to both deductive and inductive logic. The categories are shown in Table 3.
3. Results: Gender-Specific Comparison of Participant’s Experiences
3.1. Body Feeling before Disclosure of the Diagnosis and before Hormonal Treatment
Between their own pre-pubertal development and that of their peers, the participants did not perceive any abnormalities or differences. Only during the time of puberty were deviations noticed. These differences and lagging physical development were experienced as a deficit by both women and men, since it had a burdensome and unsettling effect on self-perception. This deficit was described as a feeling of “otherness” by both participant groups:
Ms. Q. (24): At the age of 12, 13, 14 it started again that I thought: “Something is not right. Somehow I am different again.”
Ms. S. (44): I won’t get my period and found that super embarrassing because that makes me different. I was so shy. I wasn’t really a huge outsider but inside it felt very much like that.
Mr. H. (49): My physical development was not the same as that of my fellows. I knew and realized that I simply was not developed.
Mr. B. (44): What I was much more worried about were the effects. All the boys in my environment started changing, suddenly they got a deep voice and a beard. And sometimes 16 - 17 year olds were running about with a full beard. And I found that really cool, under the motto: listen; I already am a real man. And myself running about smooth as a kid’s bum.
The body, which was stagnating during development and remained rather infantile, was perceived with huge feelings of shame. The participants of both sexes suspected a developmental disturbance in this context and mostly felt diffuse fears and insecurities. The copingstrategy in both groups was to declare oneself a “late bloomer”:
Ms. Q. (24): The usual excuses, you are a late bloomer, we are all a little later in our family, and we all look a little bit younger. It will surely come.
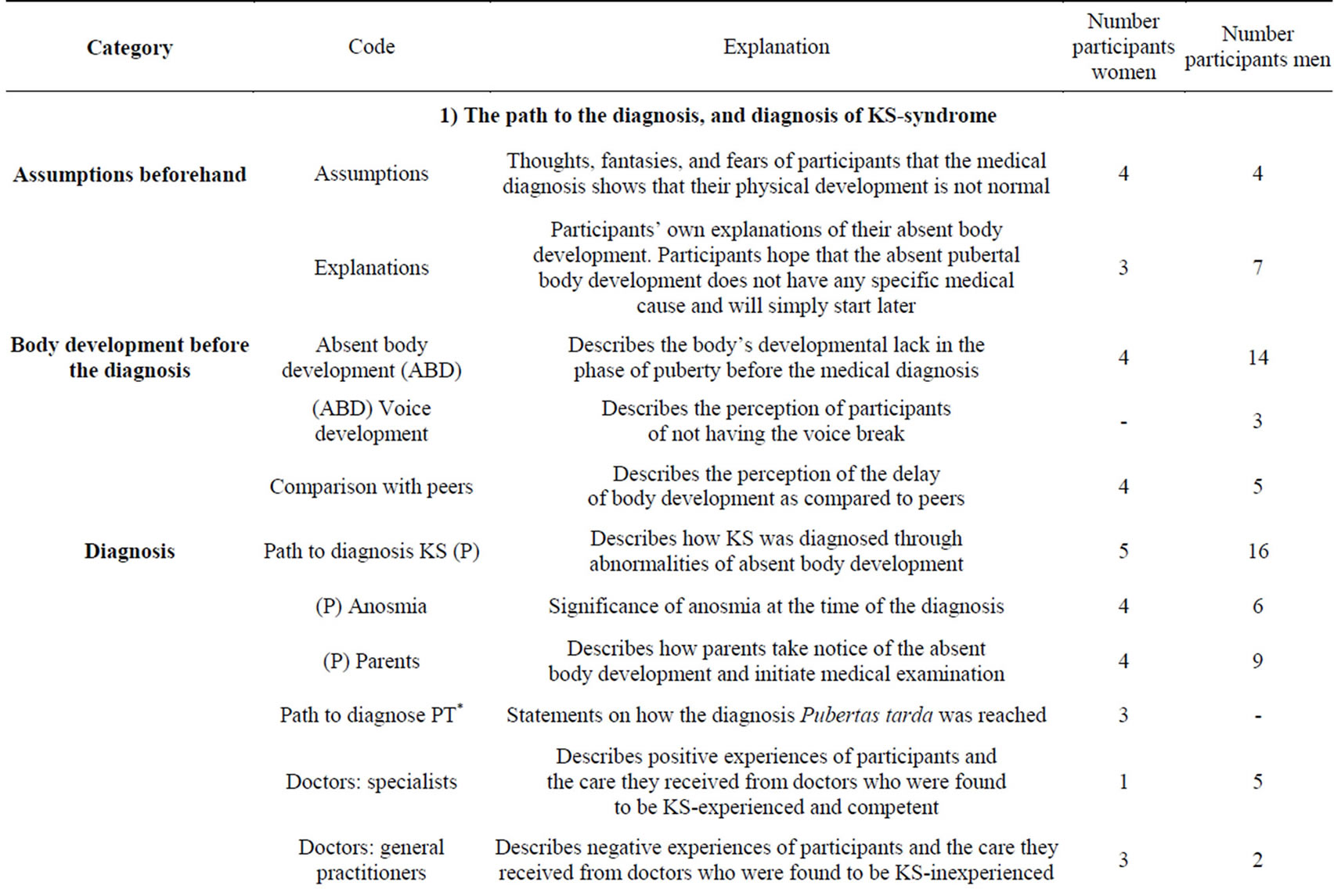
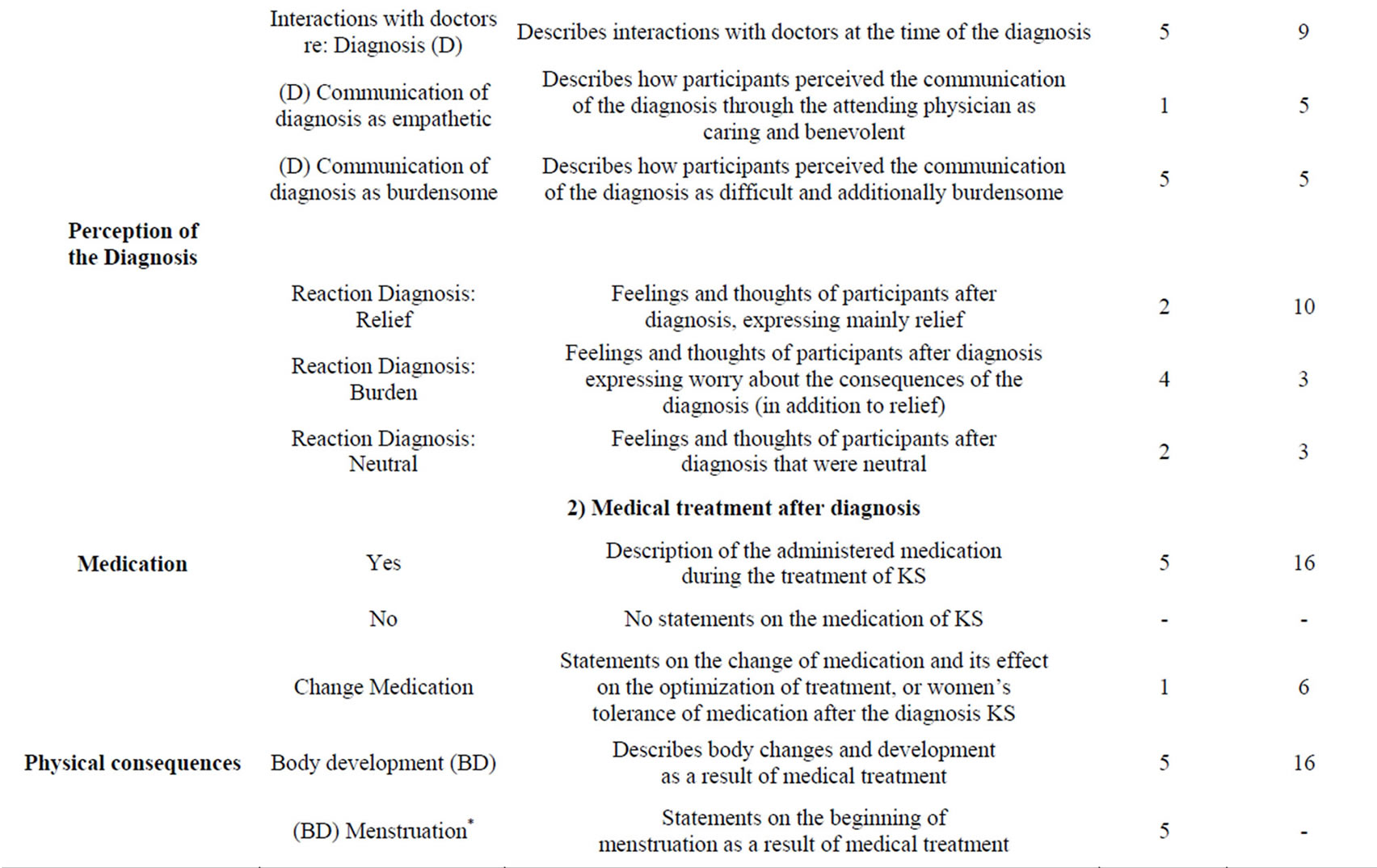
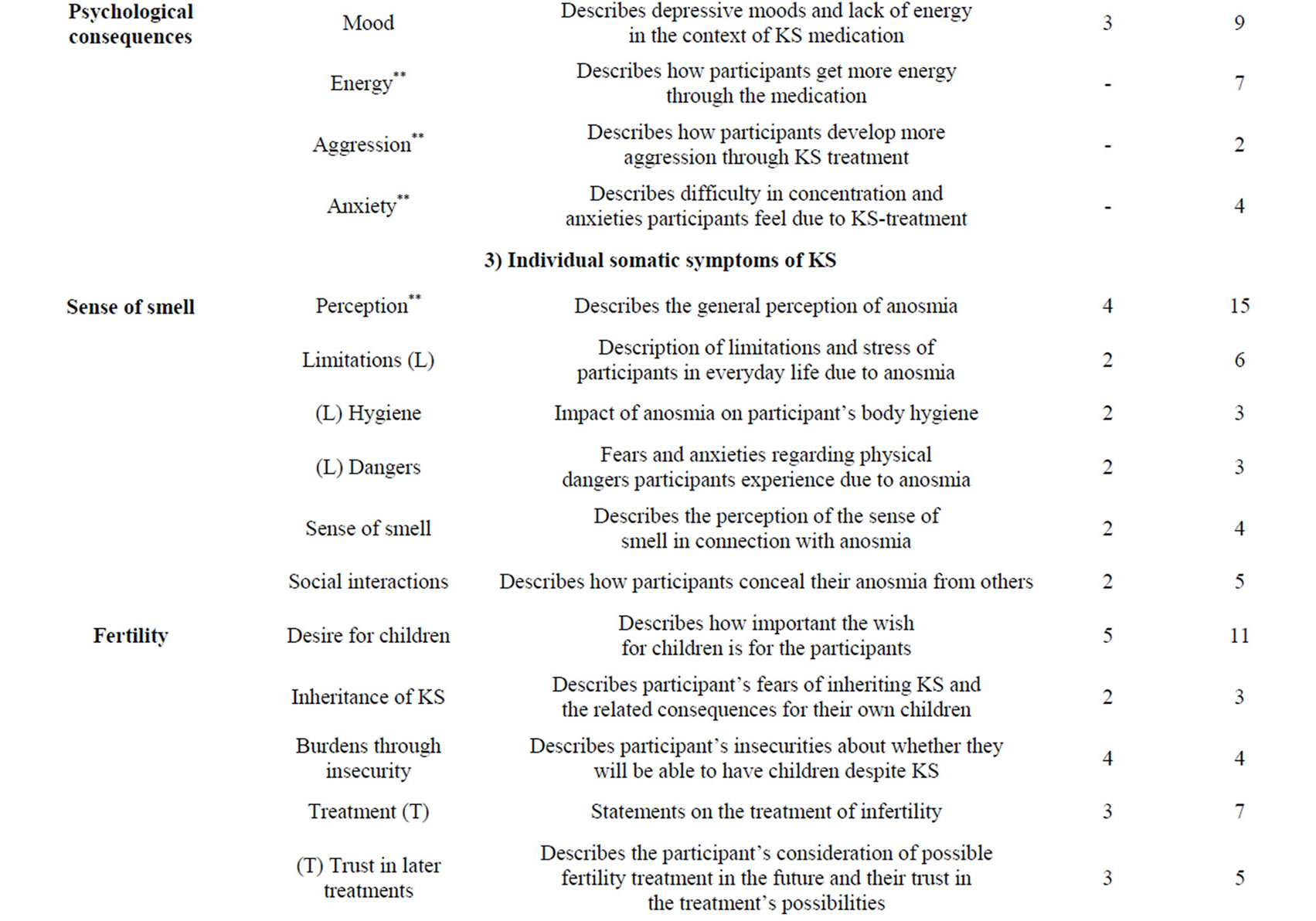
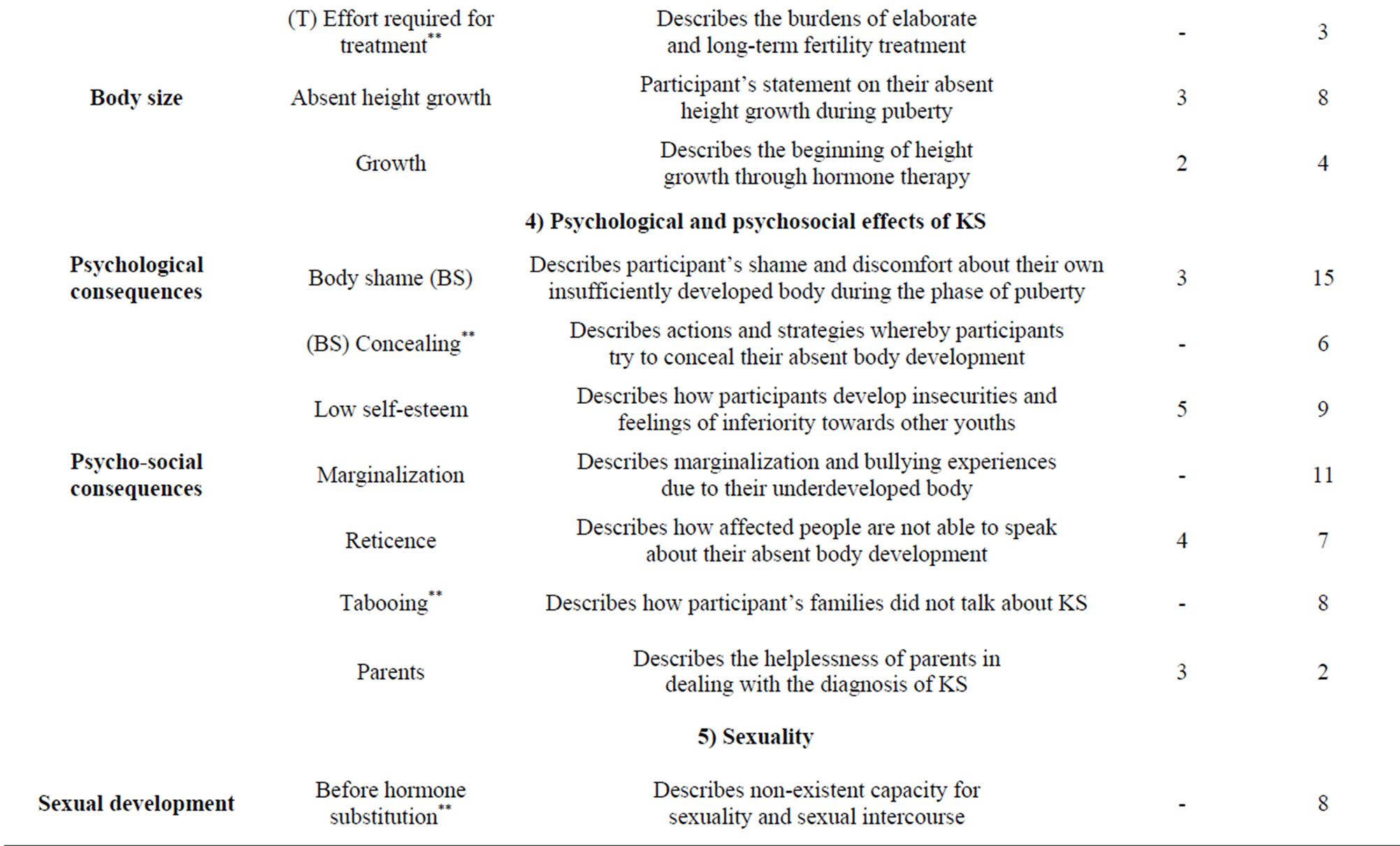
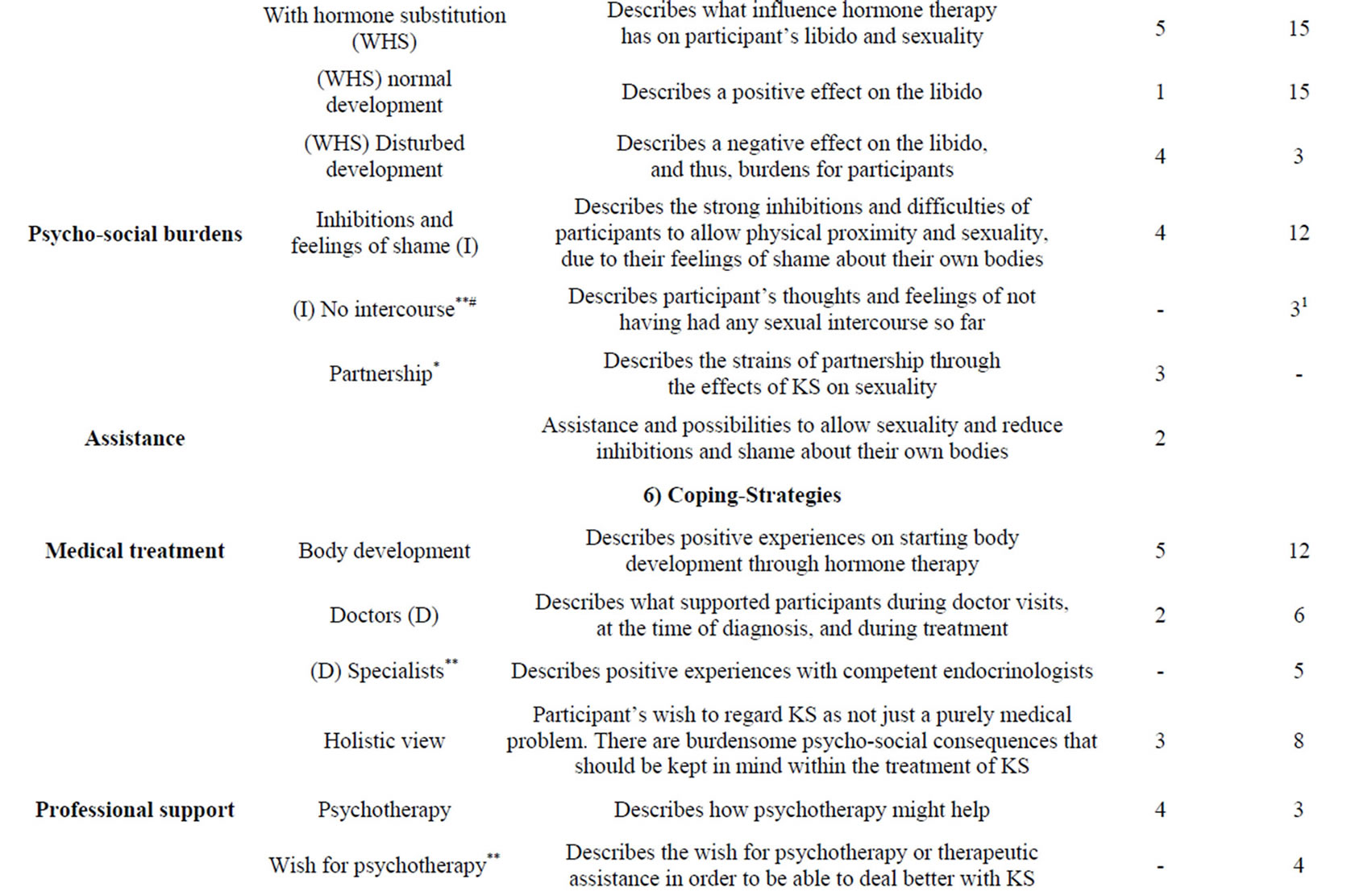
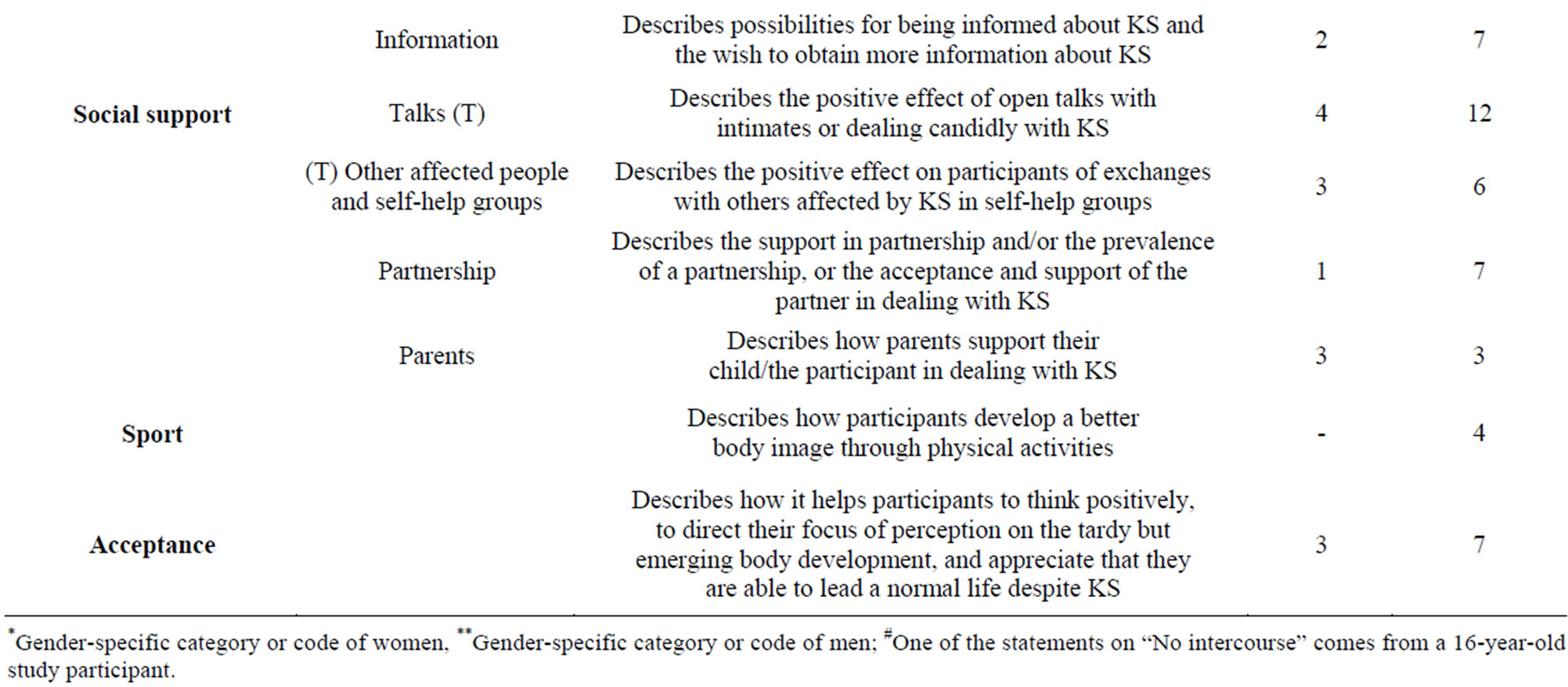
Table 3. Category system.
*Gender-specific category or code of women, **Gender-specific category or code of men; #One of the statements on “No intercourse” comes from a 16-year-old study participant.
Mr. I. (34): It was totally unclear to me. An easy explanation, always, is late bloomer of course. Since my school and kindergarten time I had attended the Waldorfschule where children are given more time.
Mr. H. (49): At that time I had the feeling it will grow out, it will still come. But it never came!
All of the men described the insecurity, the stress, and feelings of shame as more intensive and socially more impairing than was the case for the women’s sample. For half of the male participants, the shame was so great that they took great pains to hide their absent virilization. Insecurities and feelings of shame and marginalization prevented the development of healthy self-esteem. Those feelings continued during the time of puberty and during the time of KS treatment.
Ms. T. (31): Satisfied with my body? Never! At least not since I have been perceiving it consciously. I have never felt well. Going for a swim? No! Put on a T-shirt, danger of sunburn!
Mr. H. (49): And I was 19 and the concrete trigger in my case was the medical examination. That was like a panic-topic… I would have to go, undress myself. And I was terribly scared of that. I thought, if I ever get there, I wouldn’t be able to hide it any longer. So I was aware that I actually was hiding something.
Mr. L. (52): I was suffering more or less from the fact that I wasn’t developed the same way. If I was in my football team for example and when having a shower with the others, that I was teased. And that really hurt so I started to avoid such situations.
Mr. F. (25): I didn’t want to be an eye-catcher in the shower and for this reason: No, I will have a shower at home. And then people used to say something’s wrong with that guy. Yep, those are the problems.
Mr. B. (44): At that time I was in a football club, table tennis club, and during physical education at school we had swimming—all of those occasions where lots of boys change their clothes somewhere together. And of course there they look at you, you have a shower and of course there is also always someone who is running about with such physical peculiarities and therefore immediately a target. What they say is true; children can be cruel even if they are already very big kids. But of course I was a target too. And at that time I was an outsider too. And this gap had been open for a really long time.
Mr. G. (33): I felt ashamed because of it and tried to hide the whole thing as far as possible. Well, I have a brother who is three years younger than I and people became aware of the fact that something didn’t really match.
Mr. I. (34): It was like hell to worry when I felt that I developed differently or rather that the others were developing differently and I didn’t at all. That was like hell!
Two thirds of the male participants experienced marginalization by peers—which is why they perceived the beginning of virilization through the hormone treatment as all the more relieving and freeing.
Mr. I. (35): (Interviewer: What were important experiences or steps for you that your appearance, your self-esteem changed concretely?) In any case, the actual physical development taking place at that time.
Mr. L. (52): I experienced how everything started to change, which I have perceived as positive in every respect.
Mr. F. (25): By all means, it was a good feeling (the virilization, supplement interviewer) also when playing football when the boys are very fast so that I can have a shower with them and things like that. As I said earlier, I found my whole physical development more male than before so that people didn’t take me for a woman on the phone. Such things made me feel more and more secure.
Due to their feelings of shame, the affected men had a difficult time in finding suitable contacts who could address their lagging development, or to initiate a medical clarification. Half of the men commented on the taboo status of KS in their parents’ homes, while none of the women mentioned such experiences.
Mr. B. (44): We didn’t really talk about it at all.
Mr. G. (33): That was because the topic was very much of a taboo in my family.
Mr. H. (49): It was diagnosed at 19, 20 and I was born in ’59. In our family it has never been addressed… I felt that something was wrong with me but I wasn’t able to address it. I suffered from it! Also the topic of puberty and other stuff… Yes, I felt ashamed. I was not even able to address it.
It was easier for women—mostly within the context of their absent period—to address the developmental disorder, or their parents asked them to look for medical help.
Ms. S. (44): Exactly, because I didn’t get my period and at 18 finally decided to go to the gynecologist.
Ms. T. (31): It may start a little later; it doesn’t have to be unusual that it doesn’t start at the age of 12. When I was 16, my mother finally went to a gynecologist with me…
Ms. T. (31): Mainly I waited for my breasts to grow. I always had long hair, because otherwise no one would have recognized me as a girl. I asked myself: when will my body develop further? When will I look a little bit grown-up? When do my breasts start to grow? …. When my breasts started to develop they stopped at Tanner stadium 3 respectively 4.
Female participants also described insecurities and shame about their bodies. However, the feelings of shame were clearly less marked than among male participants and particularly manifested themselves during sexual intercourse (cf. 3.5). The women did not describe any bullying or marginalization experiences.
While men described numerous examples of lagging external physical development (e.g. voice, beard growth, growth of the sexual parts) in the interview, absent menstruation was perceived as very burdensome by women as the focus of their absent physical development, since this was regarded as an important step towards maturing as a woman.
Ms. Q. (24): I was so glad, I was so proud. Oh my God! This first bloody sanitary towel I had, I would have liked to stick it in my diary.
Ms. T. (31): In this sense, the period has been a sign: yes, the step is taken! You are no longer a child.
Two female participants reported that they had remained very childlike in their interests and that they only developed pubertal interests to a limited extent, such as “boys, make-up, buying bras and fashion” (Ms. Q., 24 yrs. old).
3.2. Diagnosis and Treatment
For two-thirds of the male participants and for almost all the female participants, the medical examination took place upon their parents’ advice. For the women, KS was diagnosed on average at the age of 22.8 years (SD 8,91), while the time at which participants became medically suspicious of KS for the first time occurred at the age of 13.4 years. For men, KS was diagnosed on average at 21.7 years (SD 9,99). Even though the diagnosis of KS was later for woman, they became medically suspicious earlier. The diagnosis of KS was significantly later for men than the diagnosis of an endocrine disorder in women. Since it was easier for women to address the absence of menstruation, in that the lack of a period attracted their parent’s attention, a medical examination took place at an earlier point in time for them than for men. Hormone treatment was initiated upon making the diagnosis of KS, and this detailed data is shown in Tables 1 and 2.
KS was diagnosed by a gynecologist for all five female participants. One third of the men depicted the diagnosis and their interactions with doctors as very burdensome despite simultaneous feelings of relief about the diagnosis as an explanation for their condition. In contrast to men, all five women described the examinations, the diagnosis, and interactions with doctors as burdensome.
Ms. Q. (24): (about the diagnosis, supplement interviewer) That was really terrible. I can’t tell if the word Kallmann syndrome was used. Anyhow, he examined me and oh my God, what was that like? Back then I really didn’t get what it was all about. Hormones here and there. All I remember is that he said that I had this syndrome or something and that I am not able to produce some kind of hormones, which is why my bones will break at an early age and that I would never be able to have children. And some other things like that. But all that is not so bad. If all that’s treated, I will still be able to lead a fulfilled life. Yes, that’s what he said. And I was shocked because I didn’t know anything except for this feeling, “Something’s not OK with me, something’s strange and different.” And then all of a sudden you are confronted with such a thing.
Ms. T. (31): After almost one and a half, two years of hiatus from birth control pills my gynecologist told me in 2000: “Yes, your ovaries are in a state of infertility”. Above me a DIN-A2 picture frame with nothing but newborns. In the talk before he told me I wasn’t fine at all. And that sexual interest wasn’t there at all. And his statement was: “Would you like another pill?” And “Go to psychotherapy, then everything will be fine.”
Three women first received a diagnosis of estrogendeficiency, and at a later point the diagnosis of KS. This difference in diagnosis could be one explanation for the strongly differing prevalence of KS among women versus men (cf. Chart 1).
As for the male participants, the suspicion or the diagnosis of KS were mostly reached by a general practitioner. As a result, a referral to an endocrinologist or a clinical center was made. Affected men depicted the examinations and treatments as professional. As previously noted, the male study participants perceived the diagnosis as a relief because it explained their absent pubertal development. That having been said, they were hopeful about an improvement in their condition. Nevertheless, half of the participants also expressed insecurities about what the diagnosis would still mean for their life.
Mr. G. (33): I was actually glad when they found what’s the cause. On the other hand, I also felt scared, what else does it trigger? Yes, but there was more relief. Now you know what it is.
Mr. I. (34): Well, I was extremely happy that there was finally something like a cause and also a treatment. Yet, on the other hand, there are suddenly so many things coming you haven’t thought about before. Fertility, if you want to have children. And of course you wonder: Why? Why did it happen? But you will never really get answers to that.
Mr. B. (44): Actually, it was more this comprehension.
The men who were treated by specialists were more satisfied with their treatment than those men who were treated by a general practitioner.
Mr. O. (26): Well, all of them were very competent. What I really liked very much was the fact that they always indicated where their limits were. For example, when my family practitioner immediately told me: “Well, something’s wrong, that’s all I can say but I can’t do more.” Then the doctor who said very clearly: “We’ll have to do this examination in (name of the city).” All of them dealt very frankly with it. For them it was all a little new. And for me it was a big step, when I was there I went to this chief physician in gynecology who is a fantastic guy. He knew much more than the doc because he specializes on these cases. And he really had patients with this problem, which was really reassuring to me.
Mr. B. (44): If you are confronted with such symptoms, I would recommend to everyone nowadays to move directly to a medically high level and try to consult university clinics by all means.
3.3. Body Development and Body Feeling after Starting Hormonal Treatment
For all women and men who participated in the study, the physical pubertal development was initiated by the hormone therapy. All participants of both groups described the beginning of body development through the medical treatment as positive and relieving. Men in particular reported a significantly better body image triggered by the virilization, and thus an improvement of their selfesteem. The numerous intensive descriptions of virilization among the men point to how relevant it has been for them.
Mr. O. (26): After the treatment, I perceived my body as very positive. Before that, it gave me a lot to worry about and now suddenly only joy because something has changed. I was very satisfied.
Mr. E. (39) Within months. Well, it happened relatively quickly. The growth of my body hair and the penis growth and body size.
As for most women, statements on the physical development are clearly scarcer. The topic of body development is less of a problem.
Ms. S. (44): Hormone-related, I only felt the growth of my breasts a little, nothing else. But it was OK.
Ms. U. (24): Breast growth as normal and all other characteristics where you knew they have to be. When they started, every time it was one step ahead, which made me feel more normal so to speak.
One female participant and three male participants did not perceive their body development as sufficient following the hormone treatment.
3.4. Sexuality
Both sexes addressed insecurities and major inhibitions in establishing contact with the opposite sex, because they felt ashamed of their bodies.
Mrs. T. (31): But always when it came to the point, underneath my shirt or above it. Distance! Distance! It really wasn’t easy. And if it happened, it was rather something like have it happen, bringing myself to do it and showing nakedness towards others that you are not like them.
Mrs. S. (44): There was no orgasm, for example and no desire either, but also this embarrassment.
Men commented on fears of failure when having sexual intercourse at the time of puberty and even after it.
Mr. M. (47): This weird feeling of inhibition when observing others who have got a girlfriend or something and having the feeling yourself you aren’t able to do that.
Mr. H. (44): I have pushed her aside and left her behind. I have just stopped it (Interviewer: What were you afraid of?) Yes, the shame. She would notice something.
Mr. I. (34): Addressing the topic of sexuality, I always had a very strange way because I have always had the fear of not being like the others. I mean even as a teenager with a normal development this thought is a real problem, in dealing with women at this age. How much worse must a problem be for someone who has it in black and white that he has a defect in this area?
Mr. B. (44): And one day she grabbed me between my legs. And then I panicked. I must be very honest here, she grabbed and grabbed and there wasn’t anything to grab, there was nothing. And at that time I didn’t have a stiff member either.
Two men ages 34 and 39 did not establish any contact with women in adulthood, neither in the form of sexual contacts nor other types of relationships. The exact age for the first sexual intercourse and first sexual experiences without sexual intercourse among women and men can be found in Tables 4 and 5. Male participants experienced their first sexual intercourse as helpful if they noticed that their female partners accepted them and their bodies and did not find any fault with their bodies. Male participants realized that their sexual and body-related fears were without reason. All men reported normally functioning sexuality and an increase of libido at the start of the hormone treatment.
Mr, F, (25): When I realized that this cooperation might work somehow. And I have always had positive feedback from women that it is not about me and myself but rather about something else. And that’s when I realized that this interplay of head and body just doesn’t work with me and then I received a little self-confidence and then that also stopped. At the beginning I thought that nobody found me interesting or that nobody would notice that I am different somehow. But then the first steps as far as sexuality is concerned have strengthened me in the liaison. Well, that really was important.
Mr. M. (47): I think the most important moment was the moment I slept with a woman. It just worked. And obviously for our mutual satisfaction. And that I was lucky enough that is was someone I could talk about it without this fear to become unattractive through it.
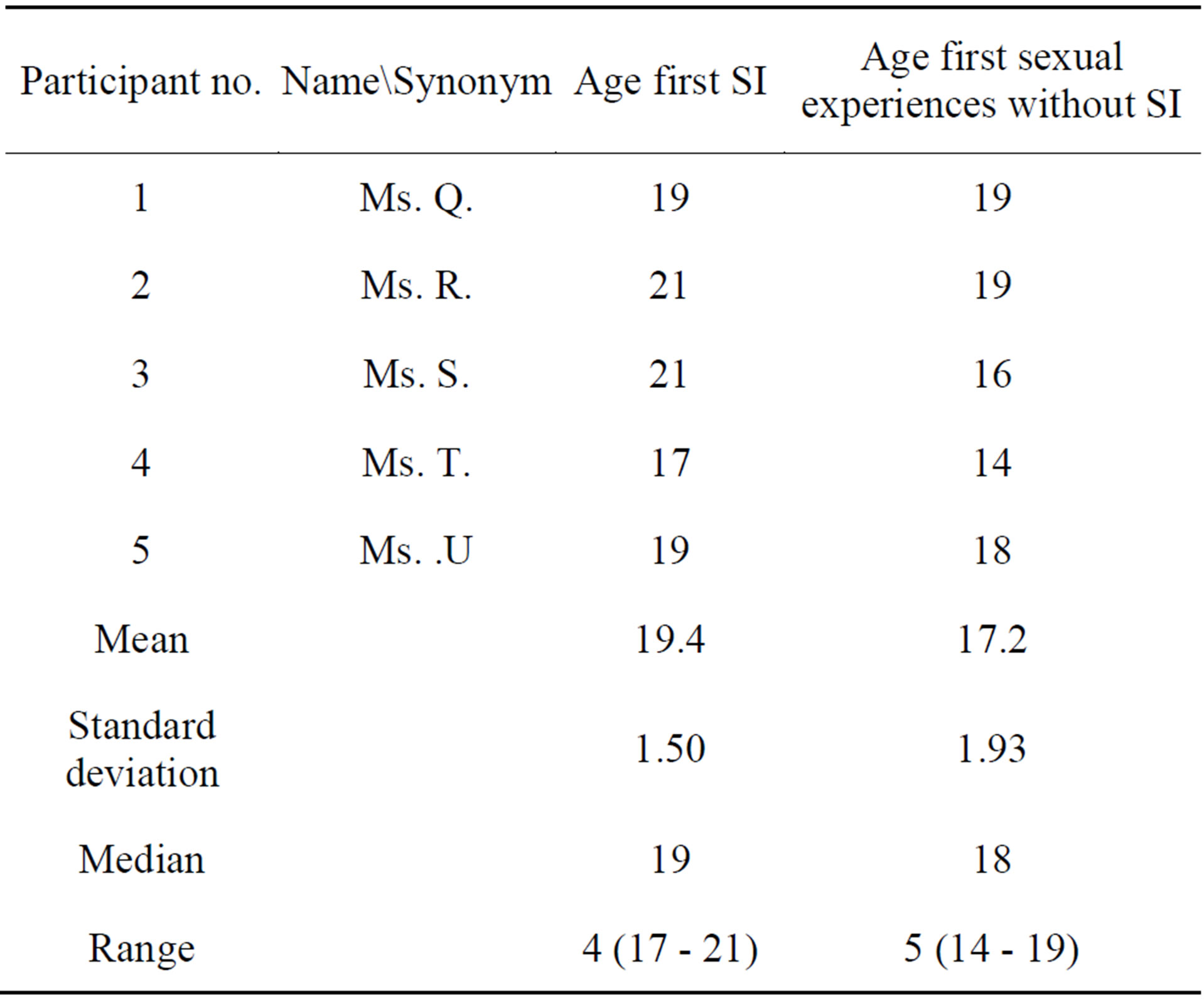
Table 4. Female participants’ age at first sexual intercourse and first sexual experiences without SI.
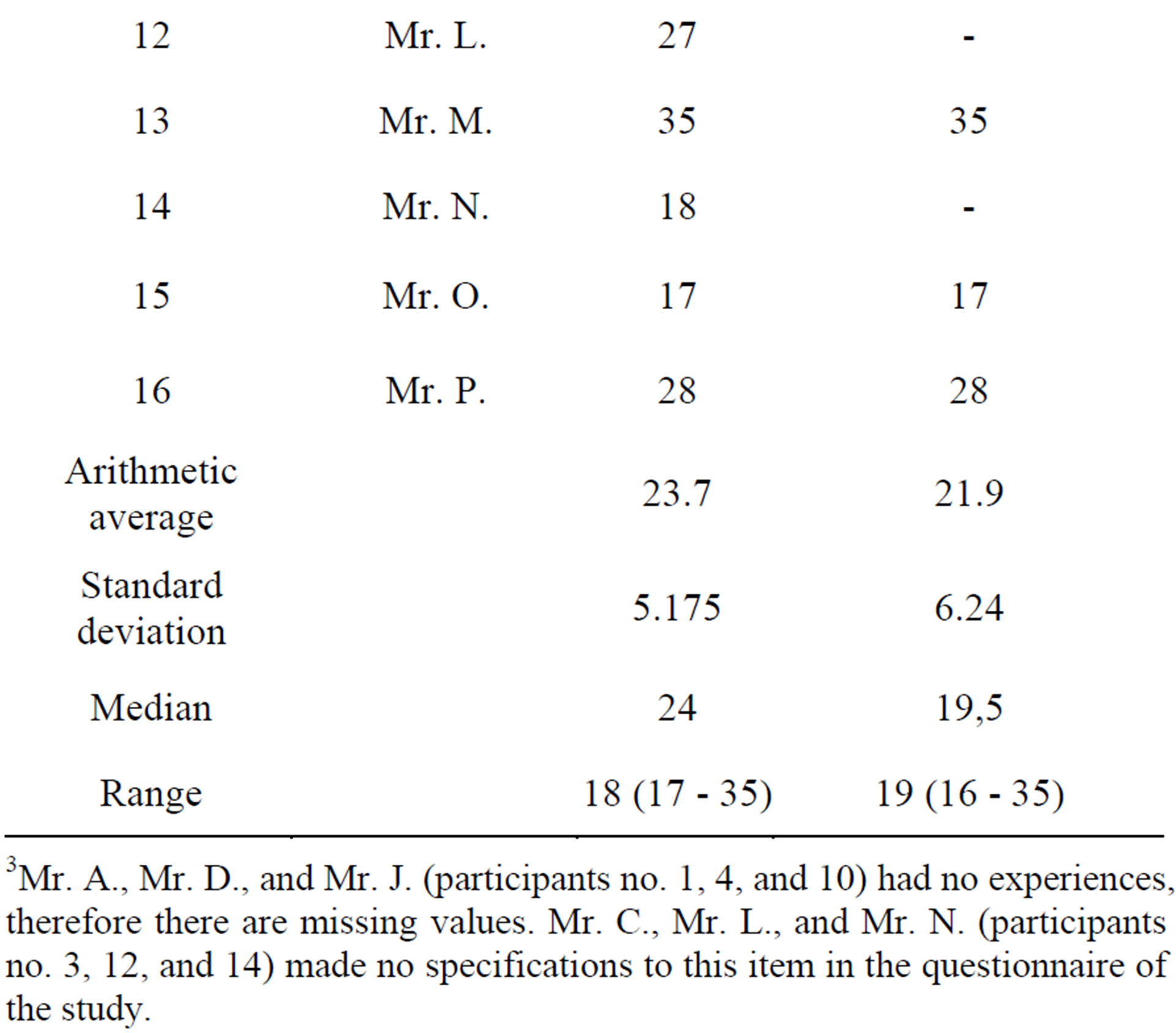
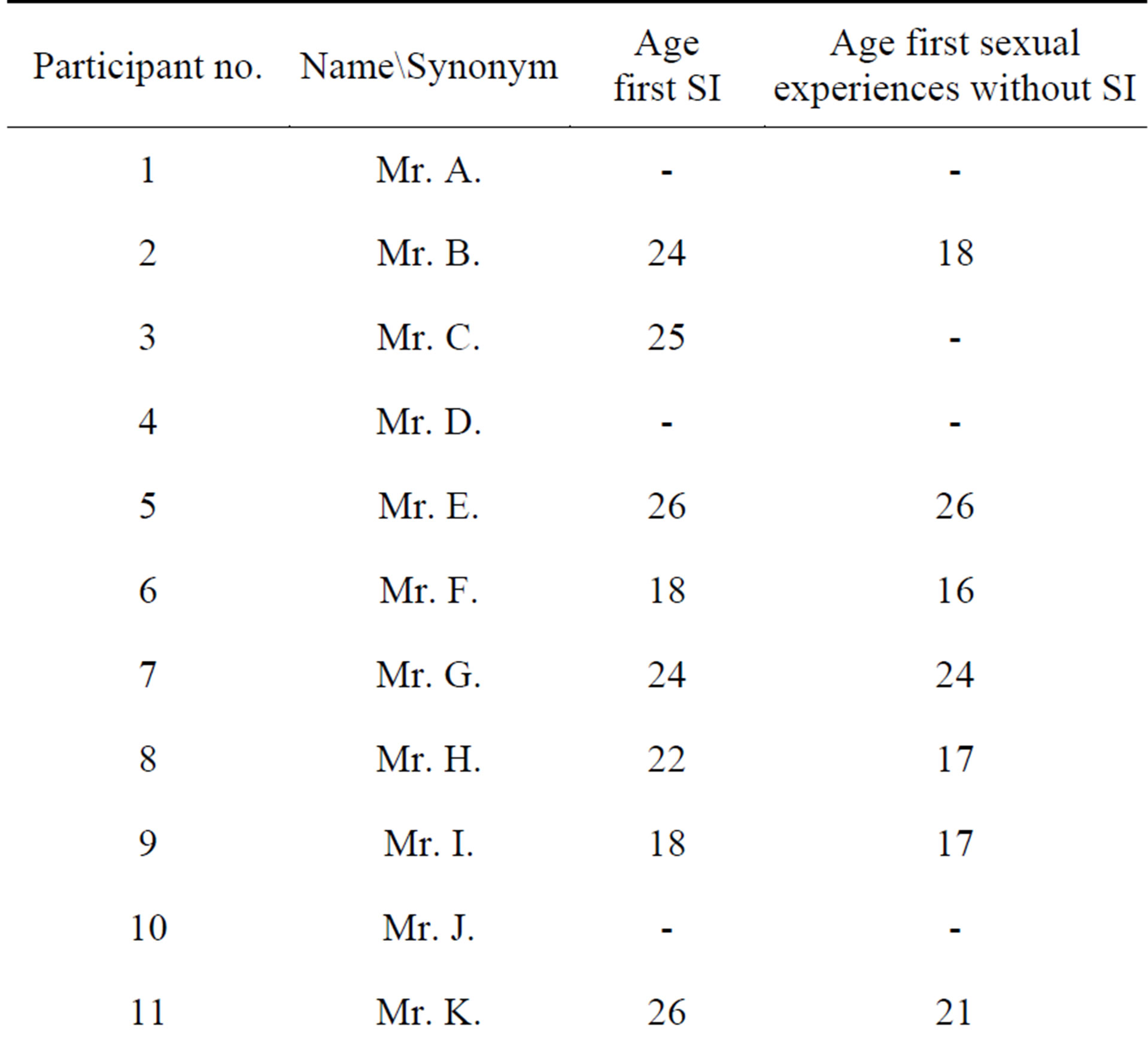
Table 5. Male participants’ age at first sexual intercourse and first sexual experiences without SI3.
3Mr. A., Mr. D., and Mr. J. (participants no. 1, 4, and 10) had no experiences, therefore there are missing values. Mr. C., Mr. L., and Mr. N. (participants no. 3, 12, and 14) made no specifications to this item in the questionnaire of the study.
Mr. I. (34): (About sexual intercourse with women, supplement interviewer) Actually, I was always scared of it. Well, in the theoretical dealing with it. In practice, not at all. Maybe also because you realize sometime that basically it is about very different things.
Mr. C. (40): Yes, the ability for erection. That’s true by all means. Before that there was nothing at all. So you feel a kind of urge. Well, that had always been missing beforehand. It does not necessarily have to come to sexual intercourse, but this inner drive was somehow missing before that.
Three female participants reported a loss of libido during hormone treatment, which has led to problems in their relationships.
Ms. T. (31): I spent two years of my life without any single thought of sex. Somehow I realized that it can’t be normal after all.
Ms. R. (31): Only a little petting with him. There wasn’t much more than that. And then with my current husband. It took about two years until we made love for the first time… I would possibly wish for fewer sexual problems. When we have come to my limits during these sexual actions, however, I hadn’t told him anything about it beforehand and rejected him. At first, he didn’t understand anything. Later I explained it a little bit to him. Yes, then everything was somehow settled. And one day I knew what it was called. It played a role to the extent that if it is connected with the Kallmann, what I expect, that my sexual activity is not very high.
Ms S (44): After 5 years without any sexual-relationship it was of course super difficult on a personal level.
Four of the interviewed women felt sexually restricted due to shame about their own bodies, which manifested itself in hiding their bodies from their partners. For women, inhibition in the area of sexuality was stronger, as it was influenced by their low libido, while for men inhibition was stronger due to low self-esteem and feelings of shame as a consequence of absent body development.
3.5. Fertility
Men and women trust that the medical treatment will enable them to have children. The time of the fertility treatment was burdensome for the male participants due to the stress of frequent doctor’s visits, the expenditure of time and money, insecurity about the chances of success, and also due to fears that they would pass KS on to their children (Mr. B., 44 yrs. old: “the fact that we had very massive problems with our family planning”). One woman got pregnant through a fertility treatment at the time of the survey. She mentioned barely any stress through the treatment. The women who very much wanted to have children faced stronger insecurities due to the diagnosis than women who had dealt with the topic very little or not at all. In particular, the question of whether children might inherit KS caused great insecurity as to whether the coming child could subsequently suffer with this condition.
Ms. R. (31): Well, the topic “what does my child inherit” or “how will it be with them” is more relevant to me. And then there are the fears I had been having for a long time, which is why I had been reluctant to become pregnant for a long time. Because you never know what will happen to the child. If it has the same things as I do, it is OK. I can live very well with it.
Ms. T. (31): Well, there was still a little hope when it comes to the desire for a child or the fulfilment of the wish. And I have to say that if that hadn’t existed, I wouldn’t know if I would still be here today…. It has always been very, very important. Even before the whole thing started. As long as I can remember I wanted to have children, or at least one.
Mr. L. (52): And my wife is by far younger than I, she is 15 years younger. She also is at an age where the desire for a child is very strong. Because in her professional life she has reached a lot of things already, finished her studies and so on. And now the time has come. And that’s what we experience a little as a lack. And I already realize that the desire for a child is very strong in me.
Mr. I. (34): Yes, well I am trying to ‘pregnant’ my wife, so to speak. And yes, that needs a lot of time and organization to do that over a longer period of time.
3.6. Anosmia and Height Growth
Both participant groups described anosmia as a limitation of their quality of life, but one that was not of much consequence. However, they felt insecurities concerning their body hygiene and concerning dangers coming from outside, such as not being able to smell escaping stove gas.
Ms. T. (31) I don’t feel influenced by it. I don’t smell anything 100%. If there was steaming coffee in the pot, I wouldn’t be able to smell it. If I put on some perfume and in the moment the alcohol has not yet evaporated, I notice that there’s something. And I can also say that it’s strange, disgusting or pleasant. But I don’t smell more.
Ms. R. (31): Well, that’s of course a kind of dimension, which somehow escapes you a little bit, actually. But since I don’t know it, I don’t really miss it in that sense.
Mr. C. (40): For us, who can’t smell, it’s not so much of a problem. Yes, because we are accustomed to it. Yes, I don’t really have any big limitations. The only thing I feel I have to pay more attention to than others is my body care because I just don’t smell it.
Mr. O. (26): At the beginning I found it very exciting because it didn’t disturb me much. It has actually never bothered me that I can’t smell, that I miss out on something because I just can’t change it.
Eight of the 16 men interviewed reported height growth disturbances during their time of puberty. They felt insecure due to their small size and perceived it as burdensome, particularly towards peers who had exceeded them in their growth potential. Three of the participating women addressed this aspect, yet did not describe it as particularly burdensome.
Ms. Q. (24): I still have some pictures of that time. Back then, it never really caught my attention but I was at a summer camp and really seemed very small and slender among all the others.
Ms. U. (24): And when I started taking the tablets, it became very normal. I grew just like anybody else, only a little later.
Mr. O. (26): I think all the others did of course grow and got lower voices and grew. I was teased because of my size.
Mr. H. (49): That I was a rather small, slender, and also rather female-seeming teenager at the age of 17, 18… I used to be relatively short as well. After the beginning of the therapy I continued to grow, certainly 10 cm.
3.7. Relationship between Hormonal Therapy and Mental Health
Men experienced a growth of activity and energy, and also something of an increase in aggression and inner turmoil after the start of the treatment. They noticed this increase immediately after starting the medication. A large percentage of them also described how this increase slowly tapered off during the weeks to come. With the decrease of the testosterone level, depressive moods and phases of “tiredness” occurred.
Mr. A. (16): Sometimes you just get a little more cheerful, but also feel a little better in terms of sports.
Mr. G. (33): At the beginning it was difficult when I stopped taking Testogel and then built up the other one. I faced extreme mood changes and wasn’t even able to recognize myself… Then I felt that I was lacking testosterone. Well, lack of drive and zero-tolerance but also imbalance.
Mr. I. (34): Well, a higher testosterone concentration in your blood, which is why it finally led to feeling more energized and much too fit.
Mr. P. (50): He filled me up with testosterone. But the effects were simply too strong and too extreme. I got a voice break and well, my personality, I became more aggressive. I became fitter as well and I constantly had problems with my libido or with sexuality.
Three of the five interviewed women also reported mood changes due to the medication, which they described as continuously depressive phases. In this context, the three complained that their doctors did not react sufficiently to the psychological burdens caused by the hormone treatment4.
Ms. T. (31): Yes. In [name of the city] they first of all gave me Trisequenz. Half a year later the effect wore off. Well, nothing of the positive effect had remained, except for the period. Then I got Trisequenz Forte, which had a positive effect at least on my general condition for about half a year… After Trisequenz Forte, when they didn’t want to give me anything else, my physical condition and self-perception and also my ego, the mind and everything else went very much south.
Ms. Q. (24): Physically speaking, I didn’t have any problems, but just psychologically because I had never been cared for by psychologists in a reasonable manner.
3.8. Coping Strategies, Resources and Aid in Dealing with KS
Both the female as well as the male participants experienced caring talks about KS and its consequences as helpful. For the male participants, it was important to overcome shame and insecurities to be able to talk about KS. They commented that their fears of being perceived “differently” disappeared, particularly in exchanges and contact with other people.
Ms. U. (24): Then my brother (with KS diagnosis, interviewer) went abroad and it was a little difficult then because he had gone and I thought I couldn’t confide in anybody and nobody would understand me in this respect.
Ms. U. (24): Yes, the (peers, supplement interviewer) mostly didn’t know what it was. And they said how that would be treated and if it didn’t have any negative effects or something like that. But they dealt with it quite normally. Not like “You are leprous now.” Actually, not at all. They were relatively understanding, I would say.
Mr. O. (26): Because I couldn’t really deal with this insecurity. Or this secret mongering. I didn’t want to keep it secret towards people who are important to me. I somehow wanted to get rid of it. And my parents advised me to talk to them. That was the best I could do. I believe if it’s about advising people: Dealing candidly with it is the very best. I have experienced that myself. Afterwards it was much easier and everything worked much better! And they also understood it.
Mr. H. (49): (Interviewer: What helped you most in dealing with them?) Well, actually talking about it. Talking about how it was… For me it was really important to be able to talk about it… It always required a certain relationship of trust.
While men found support in their social networks, four of the interviewed women also made use of professional support in the form of psychotherapy or other therapeutic methods. While only three of the interviewed men saw a psychotherapist, a quarter of the remaining interviewed men regarded psychotherapy as a meaningful support in dealing with KS. Six men turned to support groups.
Mr. G. (33): I dealt with it via the forum. Hey, there are still other people who feel the same. That has helped a lot, also for my self-esteem.
All the female and male participants perceived the beginning of pubertal physical development and the emphasis on normalization of body development through hormone treatment as very positive. They experienced it as invigorating and strengthening.
Ms. U. (44): Because back then I was always told: Now you have a very normal development. There was always the focus on the fact I am quite normal. It is basically only replacing your hormones. The development, physical development happens as with all the others. Maybe a little later, but it just happens. That’s why it was quite normal for me, like with every other youngster, too.
Mr. M. (47): Well, it is certainly connected with this feeling that I am able to lead a normal life to some extent.
Many of the men emphasized that the insecurities they had experienced in connection with their body and sexuality relativized thanks to the hormone treatment and with ongoing life experience, or that it even disappeared completely. They realized that other aspects came into focus in their relationships, and that the developmental disorders they had experienced due to KS had a significantly lower effect on their sexuality and relationship than they had feared initially.
While women did not report any comparable experiences, one female participant described how her body image and dealing with her body and sexuality strongly improved through sexual therapy and psychotherapy.
Ms. S. (44): Yes, I would always swear that it doesn’t have anything to do with hormones, but that’s just my psych work.
Concerning the medical treatment, both female and male study participants had the following wishes:
1) That KS be treated from a holistic point of view;
2) A stronger consideration of the psychosocial effects of KS during treatment, e.g., in the form of offering talks about sensitive topics like body development during the time of puberty, where fears and burdens can be addressed;
3) Psychotherapeutic support when necessary.
The male participants particularly wished for an earlier diagnosis, and to start the hormonal treatment as early as possible. The female participants wished for better information emphasizing the role played by doctors in their treatment.
4. Discussion
For the examined men, the psychological consequences of insufficient pubertal body development were perceived as being much more burdensome than for the women. This became apparent through the men’s detailed depictions of their absence of body development and of the viralization they experienced through hormone treatment. The great relief provided by virilization, as addressed by the interviewed men, can be interpreted as an indicator for a decrease in the high degree of pressure they experienced, particularly with reference to personal contacts, and comparison and exchange with peers. A possible explanation for the gender disparity is that male pubertal development is perceived as more striking (e.g. by means of beard growth, voice break, penis growth). This could be another, complementary explanation for the higher prevalence of KS diagnoses among men, other than the more prevalent first diagnosis of estrogen lack among women.
Another possible explanation is that the more striking physical consequences of KS are more burdensome to male youths and adults, giving them a higher degree of suffering. They perceive their bodies as not masculine enough, and are therefore dissatisfied with their body image. They are exposed to a high degree of social pressure, since they are not able to fulfil a particular male body image. This could also explain the taboo on discussing KS or absent body development in the parental home, especially since it was frequently fathers rather than mothers who were overtaxed with the diagnosis when they had wished for a “real man” (quote from Mr. B.) as a son.
Insufficient satisfaction with their bodies led to low self-esteem in the investigated sample of men and women, which intensified the social insecurity of participants even more. Satisfaction with one’s body is closely related to value of self, even in those with unaffected pubertal development [32]. Especially during puberty, teenagers are looking for models of male and female socialization in their environment and in the media [33,34]. The body image of girls in puberty is influenced by the wish for a slim body [33], which KS often imposes. For this reason, the burdens of KS regarding body development seemed to be lower among the interviewed women. It is striking that all female participants addressed the issues of absent menarche and an underdeveloped body only as tangential issues.
In contrast, it can be assumed that for men, the physical effects of KS (childlike appearance, delay of height growth, less muscle development, etc.) prevent attainment of the socially imparted ideal body image, while for girls, the effects of KS are less stigmatizing. Male youths frequently define their boyhood or manhood via physical aspects [35], connected with an athletic and muscular outer appearance [32,33]. The comparison with peers with regard to body, gender, sexuality, and frequently, displays of masculinity take on an increasingly more important role among youths [34]. This may generate a negative body image as a consequence, particularly during puberty where an especially high degree of body consciousness evolves [33].
These youths wish to be part of their clique of peers. This requires physical coherence, since attractiveness and admiration are understood as being very important to popularity among peers, particularly boys [33]. In seeking acceptance, there is also competitive pressure to stand the pace in physical terms ([35], p. 212). In the investigated sample, the physical burdens of absent development only occur in comparisons with the development of peers. This would support the results by Bobrow et al. [26] and Neemuchwala [22,23], who report on delimitations due to the underdeveloped body. Davison [33] goes on to say that youths who are dissatisfied with their own body image have difficulties in relationships with the opposite sex. These findings by Davison [33] confirm the investigation results of the studies.
Emphasizing the normalization of body development though hormone therapy should be a focus of counselling or psychotherapeutic support. Talk sessions allowing KS to be addressed along with the related self-worth problems of those affected are regarded as favorable. This is especially relevant for men affected with KS. In addition, strengthening self-esteem and body perception as well as developing social competences is important for the affected men.
Offering trustworthy opportunities to talk during diagnosis, in which questions on fertility may be clarified, is particularly important for the affected women. Both sexes have expressed a need for a sexual-therapeutic or sexual-pedagogic support, which is confirmed in the statements by Tsimaris, Nikolaos, Iliodromiti, and Deligeorglou [15] as well as Han and Bouloux [18]. Within the medical treatment, the dosage of hormones and observance of their effects on mood are particularly important. Especially for women who react to the administered hormones with mood changes, provisions must be made for relief.
Results as to the impact of medication on libido and mood can only be evaluated to a limited extent, due to the small sample and the qualitative-explorative research design. They do, however, point to the fact that more extensive research with corresponding study design would attain similar results. Still to be expected are investigations exploring to what extent the medication and hormone dosages have psychological consequences for the affected parties. Such studies may verify the above results, and help doctors support the affected people in dealing with KS, so as to meet their care demands in a medically adequate manner.
The following additional questions appeared within the present explorative study:
• Which effects do the gender-specific hormone medications have on mood and libido in the affected women and men? Future studies could take the form of large-scale quantitative investigations of the theses put forward thus far.
• How could early diagnosis and treatment be secured and contribute to decreasing the physical strains and consequences of absent body development, at an early stage? It must be assumed that reduced physical symptoms cause less psychological impairment.
• Which psychotherapeutic offerings are necessary to adequately support those affected? What forms of sexual-therapeutic or sexual-pedagogic support are appropriate? Which effects would they have on the affected people?
Acknowledgements
Thank you to all the study participants who shared their experiences so willingly and honestly, and to the physiccans and other health professionals who gave their time to assist in recruitment.
I would like to thank Dipl.-Psych. Kerstin Krupp, Dipl.-Psych Franziska Brunner and PD Dr. Dorothea Huber for their assistance in the organization of the study.
Funding for this work was received from the German Society of Sexual Research.
REFERENCES
- J. Hofmann, M. Watzlawik and H. Richter-Appelt, “Leben mit dem Kallmann-Sydrom—Narrative Erfahrungsberichte von Männern,” Zeitschrift für Sexualforschung, Vol. 2, No. 26, 2013, pp. 99-121.
- J. Hofmann, M. Watzlawik and H. Richter-Appelt, “Leben mit dem Kallmann-Sydrom—Analyse Subjektiver Erfahrungsberichte von Frauen,” Geburtshilfe und Frauenheilkunde, 2013.
- P. Mayring, “Qualitative Inhaltsanalyse: Grundlagen und Techniken,” Beltz Verlag, Weinheim, 2007.
- C. Dodé and J.-P. Hardelin, “Kallmann Syndrome,” European Journal of Human Genetics, Vol. 17, No. 2, 2009, 139-146. http://dx.doi.org/10.1038/ejhg.2008.206
- A. L. Mitchell, A. Dwyer, N. Pitteloud and R. Quinton, “Genetic Basis and Variable Phenotypic Expression of Kallmann Syndrome: Towards a Unifying Theory,” Trends in Endocrinology and Metabolism, Vol. 7, No. 22, 2011, pp. 249-258.
- H. M. Behre, F. Tüttelmann, S. Ledig and P. Wieacker, “Hypogonadotroper Hypogonadismus Aufgrund eines IHH oder KS beim Mann,” Medizinische Genetik, Vol. 23, No. 2, 2011, pp. 254-258. http://dx.doi.org/10.1007/s11825-011-0278-8
- G. MacColl and R. Quinton, “Kallmann’s Syndrome: Bridging the Gaps,” Journal of Pediatric Endocrinology & Metabolism, Vol. 18, No. 6, 2005, pp. 541-543. http://dx.doi.org/10.1515/JPEM.2005.18.6.541
- J. C. Pallais, M. Au, N. Pitteloud, S. Seminara and W. F. Crowley, “Kallmann Syndrome,” 2011. http://www.ncbi.nlm.nih.gov/books/NBK1334/
- P. Dandona and M. T. Rosenberg, “A Practical Guide to Male Hypogonadism in the Primary Care Setting,” International Journal of Clinical Practice, Vol. 64, No. 6, 2010, pp. 682-696. http://dx.doi.org/10.1111/j.1742-1241.2010.02355.x
- J. D. Kaplan, J. A. Bernstein, A. Kwan and L. Hudgins, “Clues to an Early Diagnosis of Kallmann Syndrome,” American Journal of Medical Genetics Part A, Vol. 152A, No. 11, 2010, pp. 2796-2801. http://dx.doi.org/10.1002/ajmg.a.33442
- DGKJ, “für die Leitliniengruppe Pubertas tarda und Hypogonadismus,” S1—Leitlinie (1. Auflage), DGKJ, AWMF, Berlin, Düsseldorf, 2011.
- P. Skalba and M. Guz, “Hypogonadotropic Hypogonadism in Women,” Polish Journal of Endocrinology, Vol. 62, No. 6, 2011, pp. 560-567.
- J. Balasch, F. Fábregues, F. Carmona, R. Casamitjana and M. Tena-Sempere, “Ovarian Luteinizing Hormone Priming Preceding Follicle-Stimulating Hormone Stimulation: Clinical and Endocrine Effects in Women with LongTerm Hypogonadotropic Hypogonadism,” Journal of Clinical Endocrinology & Metabolism, Vol. 94, No. 7, 2009, pp. 2367-2373. http://dx.doi.org/10.1210/jc.2009-0262
- C. Battaglia, M. Salvatori, G. Regnani, S. Giulini, M. R. Primavera and A. Volpe, “Successful Induction of Ovulation Using Highly Purified Follicle-Stimulating Hormone in a Woman with Kallmann’S Syndrome,” Fertility and Sterility, Vol. 73, No. 2, 2000, pp. 284-286. http://dx.doi.org/10.1016/S0015-0282(99)00535-X
- T. Tsimaris, V. Nikolaos, Z. Iliodromiti and E. Deligeorglou, “Long-Term Follow-Up of Adolescent and Young Adult Females with Hypergonadotropic Hypogonadism,” International Journal of Endocrinology, Vol. 2012, 2012, Article ID: 680569. http://dx.doi.org/10.1155/2012/680569
- J. Brämswig and A. Dübbers, “Disorders of Pubertal Development,” Deutsches Ärzteblatt International, Vol. 106, No. 17, 2009, pp. 295-304.
- F.-M. Köhn, “Diagnostik und Therapie des Hypogonadismus bei erwachsenen Männern,” Der Urologe, Vol. 43, No.12, 2004, pp. 1563-1583. http://dx.doi.org/10.1007/s00120-004-0735-y
- T. S. Han and P. M. G. Bouloux, “What Is the Optimal Therapy for Young Males with Hypogonadotropic Hypogonadism?” Clinical Endocrinology, Vol. 72, No. 6, 2010, pp. 731-737.
- J. Hefner, H. Csef and J. Seufert, “Kallmann-Syndrom: Pathophysiologische Grundlagen und Darstellung zweier Patientengeschichten,” Der Nervenarzt, Vol. 80, No. 10, 2009, pp. 1169-1175. http://dx.doi.org/10.1007/s00115-009-2739-8
- A. Mokosch, C. Bernecker, H. S. Willenberg and N. J. Neumann, “Kallmann-Syndrom. Hautarzt,” Vol. 62, No. 10, 2011, pp. 728-730. http://dx.doi.org/10.1007/s00105-011-2237-3
- C. Land, “Vorzeitiger, Verspäteter und Ausbleibender Pubertätsbeginn,” Monatsschreiben Kinderheilkunde, Vol. 160, No. 7, 2012, pp. 626-637. http://dx.doi.org/10.1007/s00112-011-2609-x
- P. Neemuchwala, “Psychological Aspects of Pubertal Delay—A Psychotherapist’s Perspective,” 1998. http://www.hypohh.net/pdffiles/info2pro.pdf
- P. Neemuchwala, “Towards a Theory of Self-Esteem—A Psychotherapist's Perspective,” 1998. http://www.hypohh.net/pdffiles/info1pro.pdf
- N. Smith and R. Quinton “A Patient’s Journey: Kallmann Syndrome,” BMJ, Vol. 345, 2012, pp. 1-2. http://dx.doi.org/10.1136/bmj.e6971
- B. Meyenburg and V. Sigusch, “Kallmann’s Syndrome and Transexualism,” Archives of Sexual Behavior, Vol. 30, No. 1, 2001, pp. 75-81. http://dx.doi.org/10.1023/A:1026420824200
- N. A. Bobrow, J. Money and V. G. Lewis, “Delayed Puberty, Eroticism, and Sense of Smell: A Psychological Study of Hypogonadotropinism, Osmatic and Anosmatic (Kallmann’s Syndrome),” Archives of Sexual Behavior, Vol. 1, No. 4, 1971, pp. 329-344. http://dx.doi.org/10.1007/BF01638061
- N. Pitteloud, J. S. Acierno Jr., A. U. Meysing, A. A. Dwyer, F. J. Hayes and W. F. Crowley Jr., “Reversible Kallmann Syndrome, Delayed Puberty, and Isolated Anosmia Occurring in a Single Family with a Mutation in the FGFR1 Gene,” Journal of Clinical Endocrinology and Metabolism, Vol. 90, No. 3, 2004, pp. 1317-1322. http://dx.doi.org/10.1210/jc.2004-1361
- S. Lamnek, “Qualitative Sozialforschung,” Beltz Verlag, Weinheim, 2010.
- J. Schulz, S. Kurz and J. Zelger, “Die GABEK-Methode als Ansatz zur Organisationsentwicklung,” Institut Technik und Bildung, Bremen, 2008.
- S. Kurz, J. Zelger and J. Schulz, “GABEK als Methode zur Kollegialen Organisationsentwicklung,” Senator für Bildung und Wissenschaft, Bremen, 2007.
- G. Lucius-Hoene and A. Deppermann, “Rekonstruktion Narrativer Identität: Ein Arbeitsbuch zur Analyse Narrativer Interviews,” Leske + Budrich, Opladen, 2004.
- J. A. O’Dea, “Body Image and Self Esteem,” In: T. F. Cash, Ed., Encyclopedia of Body Image and Human Appearance, Academic Press, Waltham, 2012, pp. 141-147.
- T. E. Davison, “Body Image in Social Contexts,” In: T. F. Cash, Ed., Encyclopedia of Body Image and Human Appearance, Academic Press, Waltham, 2012, pp. 243-249.
- V. King, “Adoleszenz/Jugend und Geschlecht,” Enzyklopädie Erziehungswissenschaft Online, Bd. Geschlechterforschung, hrsg. v. H. Faulstich-Wieland, Beltz Juventa, Weinheim, 2009, pp. 1-42.
- R. Winter and G. Neubauer, “Körper, Männlichkeit und Sexualität: Männliche Jugendliche Machen ‘Ihre’ Adoleszenz,” In: V. King and K. Flaake, Eds., Männliche Adoleszenz: Sozialisation und Bildungsprozesse zwischen Kindheit und Erwachsensein, Campus Verlag, Frankfurt, 2005, pp. 207-227.
NOTES

*Corresponding author.
1The publication of the quantitative results is in preparation.
4The validity of the results depicted here is limited due to the sample size and qualitative research design. Additional deepening studies with a research design that is more strongly coordinated to the correlations between hormones and mind are needed to verify the validity of the findings.

