International Journal of Clinical Medicine
Vol.1 No.2(2010), Article ID:3222,4 pages DOI:10.4236/ijcm.2010.12007
Hyponatremia is Associated with Increased Severity of Disease in Critically Ill Children with Bronchiolitis
![]()
1University of Connecticut School of Medicine, Farmington, USA; 2Department of Critical Care, Connecticut Children’s Medical Center, Hartford, USA.
Email: ccarrol@ccmckids.org
Received August 6th, 2010; revised September 11th, 2010; accepted October 11th, 2010.
Keywords: Hyponatremia, Bronchiolitis, Pediatrics, Critical Care
ABSTRACT
INTRODUCTION: Hyponatremia is the most common electrolyte abnormality seen in the intensive care unit (ICU), and is associated with increased morbidity and mortality. Critically ill children with bronchiolitis are at risk of developing hyponatremia, due to impaired renal free water excretion and exogenous sources of excess free water intake. We hypothesize that the development of hyponatremia is associated with a more complicated clinical course in critically ill children with bronchiolitis. METHODS: A retrospective case-control study was conducted that included all children admitted to the ICU with bronchiolitis over a two year period (n = 59). Patients were divided into two clinical groups: those that were hyponatremic (serum sodium < 136 mmol/L) during their ICU stay and those that remained normonatremic (serum sodium ≥ 136 mmol/L). RESULTS: Forty-three children (73%) developed hyponatremia while in the ICU. Hyponatremic children were intubated more often than normonatremic children (OR 16.7; 95% CI 4.1-68.5); however, hyponatremia rarely developed before intubation (2%). Hyponatremic children also had a longer ICU length of stay (209 ± 137 hrs vs. 130 ± 85 hrs, p = 0.01). In a subset of intubated children (n = 44), thirty-eight (88%) developed hyponatremia. These intubated children had a lower mean serum sodium concentration (132.8 mmol/L vs. 137.3 mmol/L, p < 0.0001) than non-intubated children. CONCLUSIONS: Hyponatremia is a common comorbidity in children admitted to the ICU with bronchiolitis, and is associated with increased illness severity, as evidenced by a higher frequency of intubation and a longer ICU length of stay.
1. Introduction
Bronchiolitis is a common childhood illness. Hospitalization is required in approximately 1% of affected children, primarily because of dehydration, inadequate oral intake, or respiratory insufficiency. Between 10-15% of hospitalized children will require intensive care due to impending respiratory failure [1,2]. Predicting which patients will have a benign clinical course versus a more severe constellation of symptoms is difficult [3].
Hyponatremia is the most common electrolyte abnormality seen in the intensive care unit (ICU), with an incidence as high as 30% in some reports [4,5]. Hyponatremia develops in the setting of impaired renal free water excretion combined with an exogenous source of excess free water intake. In critically ill children, impaired renal free water excretion can be caused by acute kidney injury or the actions of the anti-diuretic hormone arginine vasopressin (AVP). AVP release is triggered by osmotic stimuli such as hyperglycemia or uremia, and by non-osmotic stimuli such as hypovolemia, hypercapnia, pain, and anxiety [6]. Sources of free water intake in this population include hypotonic intravenous fluids, gavages tube feeds, and humidified air in the ventilator circuit [6,7]. These factors are common in children admitted to the ICU with respiratory diseases.
A specific association between respiratory illnesses such as bronchiolitis and asthma and increased circulating levels of AVP has been well documented [1,5,8,9]. Hyperinflation of the lungs, a hallmark of these illnesses, reduces blood flow to the right atrium and stimulates the release of AVP from the posterior pituitary [5,8]. Patients who develop respiratory failure require mechanical ventilation and the use of intravenous fluids or nasogastric tube feeds to provide maintenance fluids and nutrition. These patients are not permitted to self-regulate serum osmolality and effective circulating volume via the thirst response, which can lead to hyponatremia. Prior studies of critically ill patients have suggested a link between hyponatremia and increased ICU length of stay (LOS) or in-hospital mortality; however, this has not been demonstrated in children with bronchiolitis [4,6,10]. We hypothesized that critically ill children with bronchiolitis and hyponatremia will have more severe underlying pathophysiology, and thus will have increased severity of illness.
2. Methods
We conducted a retrospective case-control study of all children admitted to the pediatric intensive care unit at Connecticut Children's Medical Center with a diagnosis of bronchiolitis between January 1, 2005 and December 31, 2006. The Institutional Review Board at Connecticut Children's Medical Center approved this study, and the criteria for informed consent were waived due to its retrospective nature. Children were included in this study if they 1) were admitted to the ICU with bronchiolitis, 2) had a serum sodium concentration measured on the first day of hospital admission, and 3) had at least two serum sodium concentrations measured while in the ICU. Children were identified from a previously existing database maintained for quality improvement using the search terms “bronchiolitis,” “respiratory syncytial virus,” “acute bronchiolitis,” “respiratory syncytial virus bronchiolitis,” and “viral bronchiolitis.” There were no exclusion criteria for this study. Children were classified as hyponatremic if they had at least one measured serum sodium concentration less than 136 mmol/L. Children were classified as normonatremic if all measured serum sodium concentrations were greater than or equal to 136 mmol/L. Ethnicity, gender, age, history of prematurity, intravenous fluid intake, and initial severity of illness were analyzed as independent risk factors for the development of hyponatremia. Hypotonic fluids were considered to be less concentrated than 0.45% normal saline. Pediatric Risk of Mortality (PRISM) scores were calculated to determine initial severity of illness upon admission to the ICU [11]. Primary outcomes included the need for intubation, length of mechanical ventilation, ICU LOS and total hospital LOS.
Statistical analysis was performed using the JMP statistical software package (version 7.0.2; Cary, NC) along with statistical consultation from the Office of Research at Connecticut Children’s Medical Center. Categorical variables, normally distributed continuous variables, and non-normally distributed continuous variables were compared using Pearson’s chi-square, student's T-test, and Wilcoxon signed-rank tests, respectively. Fisher's exact test was used when there were fewer than 5 cases within a category. The Shapiro-Wilk test was used to assess normality. A p-value of less than 0.05 was considered statistically significant for all tests. Normally distributed variables are reported as mean ± standard deviation, and non-normally distributed variables are reported as median (range). Odds ratios are reported with 95% confidence intervals (CI).
3. Results
Fifty-nine children were included in the study. Fortythree of these children (73%) developed hyponatremia while in the ICU. There were no significant differences in the baseline characteristics between the group of children who were normonatremic and the group of children who developed hyponatremia (Table 1). A significantly higher proportion of patients in the hyponatremic group required mechanical ventilation (Table 2), although the actual amount of ventilatory time was not significantly different between groups. Hyponatremic patients had a longer ICU LOS (Table 2 and Figure 1) and showed a trend toward a longer total hospital LOS, but this did not reach statistical significance (Table 2). As expected, the hyponatremic group had a significantly lower mean initial serum sodium concentration (Table 2). Additionally, a higher proportion of hyponatremic patients received hypotonic intravenous fluids prior to the development of their lowest measured serum sodium concentration, but this did not reach statistical significance (Table 2). Ethnicity, gender, age, history of prematurity, and PRISM scores were not independently associated with the development of hyponatremia.
A separate analysis of all children that required intubation (n = 44) demonstrated that thirty-eight (88%) developed hyponatremia (OR 16.7; 95% CI 4.1-68.5). In all but one patient, hyponatremia developed after intubation. These intubated children had a lower mean serum sodium concentration (132.8 mmol/L vs. 137.3 mmol/L, p < 0.0001) than non-intubated children.
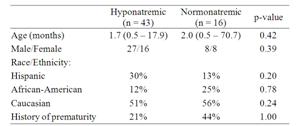
Table 1. Hispanic, African-American, and Caucasian. Demographic information.
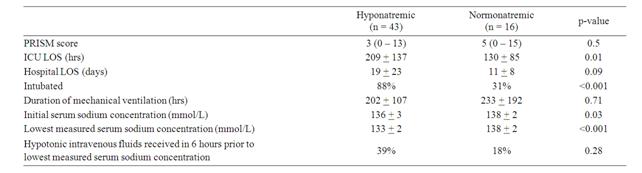
Table 2. Outcomes data.
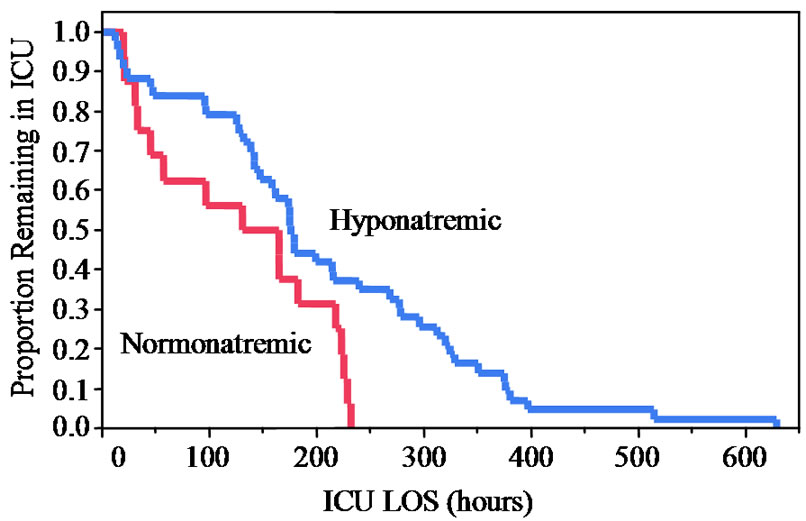
Figure 1. Kaplan-Meier Curve of ICU LOS
4. Discussion
Bronchiolitis is a common illness with a wide spectrum of clinical severity, making it difficult to predict which patients will have a more complex clinical course. In this small retrospective cohort of children with bronchiolitis, we found an association between hyponatremia and both an increased frequency of intubation and longer ICU LOS.
Interestingly, in both the hyponatremic group and the normonatremic group, mean initial serum sodium concentrations were normal (≥136 mmol/L). Only 39% of patients in the hyponatremic group received hypotonic intravenous fluids in the 6 hour period prior to their lowest measured serum sodium concentration. This could reflect a lack of fluid restriction in these patients. It has previously been shown that patients with elevated circulating levels of AVP who receive isotonic intravenous fluids at “maintenance” rates can develop hyponatremia. When under the influence of AVP and presented with a high urine flow rate, the distal nephron extracts free water and excretes the majority of the salt load in the urine, thereby returning hypotonic fluid to the circulation and generating hyponatremia [12]. Alternatively, these children could have received hypotonic fluids via nasogastric tube feeds; this information was not readily available in the clinical database.
Although a higher proportion of the hyponatremic group was intubated, they did not require longer ventilatory times than the normonatremic group. Likewise, in the separate analysis of intubated patients, those with hyponatremia had similar ventilatory requirements as those without. This was somewhat unexpected. Once intubated, we anticipated that hyponatremic patients would require more ventilatory support, as the hyponatremia may reflect either an underlying state of fluid overload or excess AVP release due to more severe pulmonary disease. These findings suggest that the development of hyponatremia may be associated with intubation, but does not reflect a pathophysiologic state that prolongs ventilatory requirements.
This study has several limitations, the most significant of which is its retrospective nature. Although we tried to correct for confounders that may have influenced the results, we probably did not account for all such factors. For example, we did not have data on the use of diuretics in our cohort, which could influence the development of hyponatremia and reflect a higher disease severity. We did not have data on nasogastric tube feeds, to determine if they were a significant source of hypotonic fluid intake. In addition, the retrospective nature of this study limited the number of serial serum sodium concentrations available for review, and made the timing of the measurements less uniform. We did not measure AVP levels or document impaired free water excretion using urinary solute studies. Finally, due to the study design, we are only able to show associations and not causations. In future prospective studies, these factors should be accounted for.
In conclusion, we found an association between the development of hyponatremia and both an increased rate of intubation and a longer ICU LOS. Additionally, the incidence of hyponatremia in this cohort (73%) was over twice that reported in other population studies of critically ill children [5,8,10,13]. Given the significant complications that could result from acute hyponatremia, clinicians should be aware of the increased risk for hyponatremia in children with bronchiolitis, especially after intubation. This study substantiates the need for larger and more complete prospective studies of children with bronchiolitis, as well as other respiratory illnesses, in order to better define the association between hyponatremia and illness severity.
REFERENCES
- H. A. Van Steensel-Moll, E. Van der Voort, A. P. Bos, P. H. Rothbarth and H. J. Neijens, “Respiratory Syncytial Virus Infections in Children Admitted to the Intensive Care Unit,” Pediatrics, vol. 44, 1989, pp. 583-588.
- K. Ventre, M. Haroon and C. Davicon, “Surfactant Treatment for Bronchiolitis in Critically Ill Infants,” Cochrane Database of Systematic Reviews, Vol. 3, 2006.
- M. Stretton, S. J. Ajizian, I. Mitchell and C. J. L. Newth, “Intensive Care Course and Outcome of Patients Infected with Respiratory Syncytial virus,” Pediatr Pulmonol, vol. 13, 1992, pp. 143-150.
- A. Upadhyay, B. L. Jaber, N. E. Madias, et al., “Incidence and prevalence of hyponatremia,” American Journal of Medicine, vol. 119, No. 7, July 2006, pp. 30-35.
- M. Eisenhut, “Extrapulmonary Manifestations of Severe Respiratory Syncytial Virus Infection-systematic Review,” Critical Care, Vol. 10, No. 4, 2006, p. 159.
- M. Halberthal, M. Halperin and D. Bohn, “Acute Hyponatraemia in Children Admitted to Hospital: Retrospective Analysis of Factors Contributing to Its Development and Resolution,” British Medical Journal, vol. 322, 2001, pp. 780-782.
- A. Sladen, M. Laver and H. Pontoppidan, “Pulmonary Complications in Mechanical Ventilation,” The New England Journal Medicine, vol. 279, 1968, pp. 448-453.
- H. A. Van Steensel-Moll, J. A. Hazelzet, E. Vander Voort, H. J. Neijens and W. H. L. Hackeng, “Excessive Secretion of Antidiuretic Hormone in Infections with Respiratory Syncytial Virus,” Archives of Disease in Childhood, Vol. 65, 1990, pp. 237-1239.
- R. P. Rivers, M. L. Forsling and R. P. Olver, “Inappropriate Secretion of Antidiuretic Hormone in Infants with Respiratory Illness,” Archives of Disease in Childhood, vol. 56, 1981, pp. 358-363.
- S. Singhi, “Hyponatremia in Hospitalized Critically Ill Children: Current Concepts,” The Indian Journal of Pediatrics, Vol. 71, No. 9, 2004, pp. 803-807.
- M. M. Pollack, K. M. Patel and U. E. Ruttimann, “PRISM III: An Updated Pediatric Risk of Mortality score,” Critical Care Medicine, Vol. 25, No. 4, 1996, pp. 743-752.
- A. Steele, M. Gowrishankar, S. Abrahamson, C. D. Mazer, R. D. Feldman and M. L. Halperin, “Postoperative Hyponatremia Despite Near-isotonic Saline Infusion: A Phenomenon of Desalination,” Annals of Internal Medicine, Vol. 126, No. 1, 1997, pp. 20-25.
- S. Hanna, S. M. Tibby, A. Durward and I. A. Murdoch, “Incidence of Hyponatraemia and Hyponatraemic Seizures in Severe Respiratory Syncytial Virus Bronchiolitis,” Acta Pediatrica, Vol. 92, No. 4, 2003, pp. 430-434.

