Open Journal of Orthopedics
Vol.4 No.5(2014), Article ID:45722,6 pages DOI:10.4236/ojo.2014.45020
The Total Hip Arthroplasty in Ankylosing Spondylitis
Hatim Abid*, Mohammed Shimi, Abdelhalim El Ibrahimi, Abdelmajid El Mrini
Department of Osteoarticular Surgery B4, HASSAN II Teaching Hospital, Fes, Morocco
Email: *hatim.abid1@gmail.com
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/


Received 19 March 2014; revised 26 April 2014; accepted 2 May 2014
ABSTRACT
Objectives: The assessment of the radio clinical results of sixty one total hip arthroplasties was performed among young and active patients, with follow-up for ankylosing spondylitis, in order to evaluate the effect of surgery on the quality of life of these patients. Methods: For the functional improvement of the patients, we relied on the scores of Devane, Harris and that of Postel Merle d’Aubeigné. The radiological analysis was based on the coxometry. Results: The study confirms the notable functional gain and consequently the improvement of the quality of life of the patients. However, the longevity of the implants remains difficult to envisage due to our limited and insufficient hindsight. Conclusion: The total hip arthroplasty transforms the life of the young patients’ carriers of the disabling coxitis on the stiffening spondylarthritis, by getting them the laziness and the mobility wished for.
Keywords:Inflammatory Coxitis, Ankylosing Spondylitis, Total Hip Prosthesis

1. Introduction
The coxofemoral attack during the ankylosing spondylitis (AS) is frequent, it is often bilateral and the natural evolution is done towards the osseous ankylosis. The latter results clinically in an articular stiffness at the origin of a severe disability on the level of the hip as well as on the level of the close articulations. Management of patients with ankylosing spondylitis is being disrupted on several points. It seems that the main reason is to take a greater awareness of the relative prevalence of this disease. The assessment of different treatment modalities is now facilitated through standardization of evaluation obtained internationally through the ASAS group (Assessment in Ankylosing Spondylitis) criteria. Non-steroidal anti-inflammatory drugs (NSAIDs) are still the bases of drug treatment. Recent studies show that specific inhibitors of cyclooxygenase type II are better tolerated in the digestive plane and just as effective as the conventional non-steroidal anti-inflammatory drugs. Therapeutic background as Thalidomide appears to be effective not only on peripheral articular manifestations, but also in patients with axial disease refractory to NSAIDs. At the stage of major functional disability, work stoppage rate in patients varies from 3% to 50% depending on the country, being above 20% in most studies. In this context of major functional change, the total hip arthroplasty transforms the life of patients, by getting them the indolence and the mobility wished for. However the problem which is posed after settles, after the gesture is the remote future of prostheses implanted to young and active subjects. We will try through this work, to evaluate the anatomoclinic results of a series of 61 patients’ follow-up for ankylosing spondylitis operated at the stage of ankylosis by total hip arthroplasty with the aim of appreciating the impact of surgical treatment on the quality of life of the patients.
2. Material and Methods
In order to evaluate our results and put the point on our experience, we conducted a retrospective study, spread over 4 years, interesting 61 cases and including all first-line arthroplasties carried out among patients with follow-up for ankylosing spondylitis at the stage of articular destruction and ankylosis. The analysis of the files enabled us to release the epidemiologic profile of our series and hospital length. For the clinical and functional assessment of the patients, we relied on different score: that of Devane (Figure 1), of Postel Merle d’Aubigné (PMA) and of Harris. The Radiological analysis was based only on coxometry only because of lack of profile incidence, on frontal radiographies. The measured parameters were normal values at the majority of the patients (Figure 2). Our patients were operated exclusively all under general anesthesia, by postero lateral approach. The intervention lasted in an average duration of 78.38 min with the installation of implant divided into cupules of 50 - 52 and 54 millimetre (mm) diameter for heads of 28 mm. The neck of the prosthesis was medium in 49 cases (Figure 3) with a tendency of cemented fixation. The torque of steel-polyethylene friction was predominant.
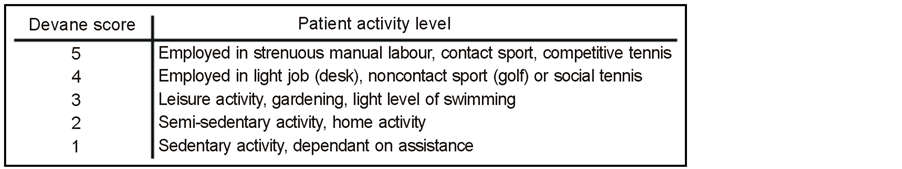
Figure 1. Devane score and the related activity.
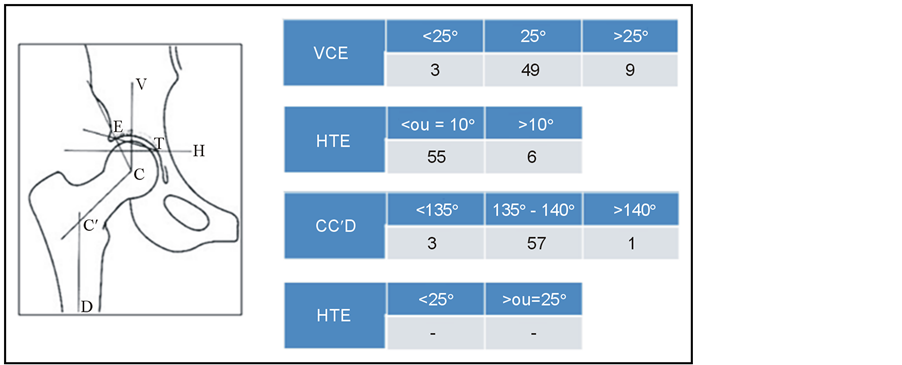
Figure 2. Distribution of patients according to the results of the preoperative coxometry. VCE: External femoral head coverage angle; HTE: Acetabular roof obliquity angle; CC’D: Center collum diaphysis angle.
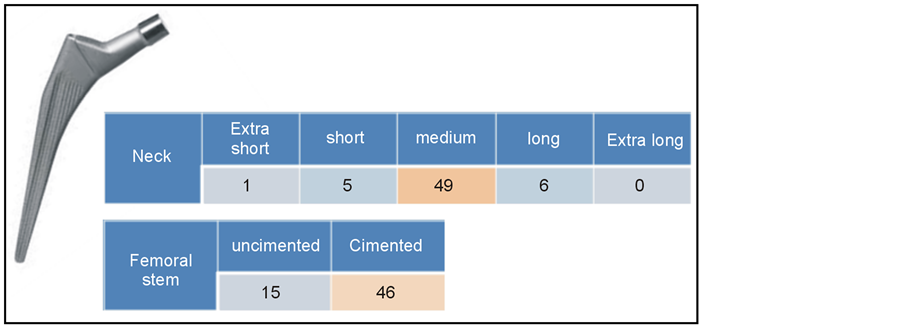
Figure 3. Distribution of patients according to the size of the neck and the type of fixation of prostheses.
3. Results
The average age of our patients at the time of the intervention was 31 years, with extremes of 20 and 55 years old. 80% of the operated were men with the implementation of 45 one sided implants, mainly of right side, and 8 prostheses in bilateral way. All our patients were operated under general anesthesia, despite the difficulties of intubation met in some patients with cervical spine stiffness. In 100% of the cases, we performed posterolateral approach of Moore. In the 75% of the cases, the prosthesis used was cemented. The reeducation was begun from the ablation of redans, and was delayed in the case of uncemented implant.
Our results were to the last recoil, which is 48 months, very encouraging with 90% excellent to good result. On the Clinical level, the average score of Postel Merle d’Aubeigne reached 16.57. The equality of the length of both lower limbs was restored in 55 cases with 5 lengthening inferior to 2 centimeters. No case of shortening of the member was observed. The post-operatively radiological analysis realized to our patients allowed to highlight from the files exploitable in this sense: the normal slope of the acetabular cupule in the frontal plan and the neutral position of the stalk relative to the anatomical axis of the thighbone in 42 cases (Figure 4). In terms of complications, we regret: 3 cases of peri prosthetic ossifications, 2 cases of deep vein thrombosis and 1 case of late dislocation.
4. Discussion
The coxites in ankylosing spondylitis arise at a young age. The possibility of early diagnosis as well as the radio-clinical and biological level must be able to benefit patients with medical treatment and functional rehabilitation that can recede long enough the time of surgery. However, the rapid stiffness or ankylosis in faulty position must push orthopedic surgeons to act and operate these patients as quickly as possible to avoid the big stage crippling deformities. In our series, the average age of operated patients was 36 years, it was of 31 years in the series of Cato [1] which included 18 total hip arthroplasties (THA), 35 in the series of Brinker [2] which included 20 THA, 38.9 years in the series of Tang [3] which included 95 THA and 47 in series of Joshi [4] which included 181 THA. With very encouraging therapeutic results reported by most authors, the young age of patients and the severity of infantile and juvenile forms should not be an obstacle to the prosthetic surgery.
It is in this sense that we operate our patients fairly quickly with deep conviction. In our series, we note a male predominance which joins that found in the literature with 60.8% of men in the series of Bisla [5] , 68% in the series of Joshi [4] and 96% for Tang [3] .
Concerning the choice of anesthetic technique for total hip arthroplasty, it is still individual for each patient; in fact no study has clearly demonstrated the benefit of regional anesthesia in comparison with general anesthesia in matter of mortality and postoperative morbidity [6] . In fact, the postoperative global prognosis is bound to the preoperative state of the patient and to its management per operative. However, no matter how the anesthetic technique is, the resuscitator may be faced with some difficulties due to the stiffness of the jaw and spinal ankylosis. In this regard, we had in our series two cases of difficult intubation conducted on rigid guide.
As for the coxofemoral surgical approach, it remains a personal choice of the operator. Joshi [4] used in his
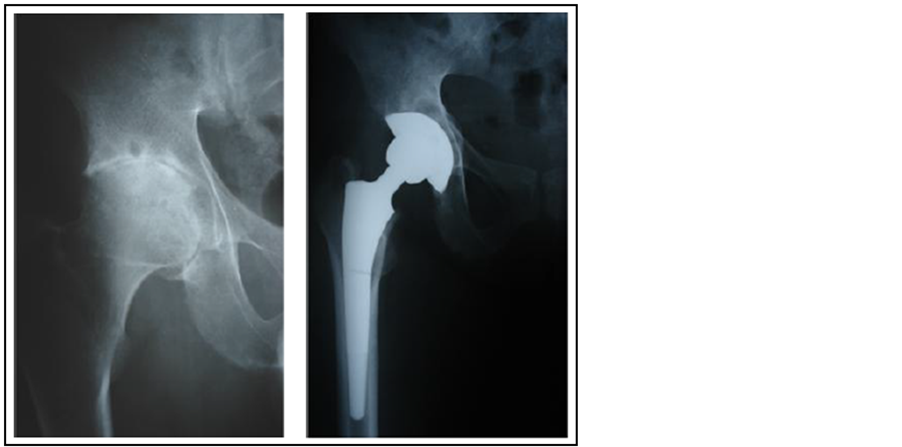
Figure 4. Postoperative control of a right THP (total hip prostheses).
series (181 THA) the external access with trochanterotomy in 91.7% of arthroplasties, while Brinker [2] approached his patients (20 THA) on 85% of the cases by Harding approach. In spite of the risk of later posterior dislocation, we used the posterolateral approach of Moore in all the arthroplasties quite as Tang [3] on a series of 95 THA and Caton [1] on 18 arthroplasties.
Until today, the choice of the prosthesis as part of ankylosing spondylitis item remains unclear. Cemented THA have more hindsight and the best results, they provide maximum primary stability in an altered bone capital. Besides, few publications were published about the use of uncemented THA during the inflammatory coxites be it rheumatoid arthritis or ankylosing spondylitis. In the series of Tang [3] (95 THA), the longevity of the cemented THA was 100% at 5 years and 96.8% at 10 years, while that of uncemented prostheses was approximately 95.5% at 5 and 10 years and fell sharply to 63.6% at 11 years. In our series, we used 50 cemented total hip prostheses.
In the literature, the evaluation of the functional results is made on the basis of Postel Merle d’ Aubigne’s quotation [7] which estimates the pain, hip mobility and the walking. In this sense, the maximum of improvement regards the postoperative pain parameter that reached in our series an average of 5.7/6 to 5.8 reported by Sochart [8] on a series of 43 THA. For mobility, the improvement was good but less spectacular with an average score of 5.2. As for walking, patients agreed in 88% of cases, their satisfaction that matched her quotes between 5 and 6. Overall, our results, although preliminary, are very encouraging and are consistent with those of international series with 90% good to excellent results. They reflect significantly improving the quality of life of patients essentially linked to the disappearance of pain, gain mobility and restoration of walking. However, the longevity of implants remains in our context which is always difficult to predict, for our limited and insufficient follow-up (Figure 5). It is important to call back in this context, the results of the multicenter study of Bonnomet and Glorion [9] holding as survival factors statistically better prostheses: A young age of implantation, the absence of surgical history on the hip, and the use of hard friction couple without distinction between the couple metal-metal and ceramic-ceramic. These couples optimize the longevity of implants by a rate of unimportant wear compared to that of the soft couples. Except the risk of ossification which seems more important, the other complications of the THA in this type of pathology do not seem to be influenced by the terrain [10] . Walker [11] reported on a series of 29 prostheses: 23% of ossification, 6.9% of unsealing, 3.7% of infection and 0% of dislocation this for recoil of 55.9 months. Kilgus [9] as for him found in his series of 53 PTH: 58% of ossification, 39.9% of unsealing, 0% of infection and 2% of dislocation for a follow-up of 76 months. In our series until the last recoil which is 48 months, we have had only 3 cases of periprosthetic ossifications with a rate of 5%. We allot this low incidence to our preventive attitude, based on the systematic prescription of non steroidal anti inflammatory drugs in the immediate postoperative period, and this for one week, referring to the result of the work of Vastel [12] in this direction.
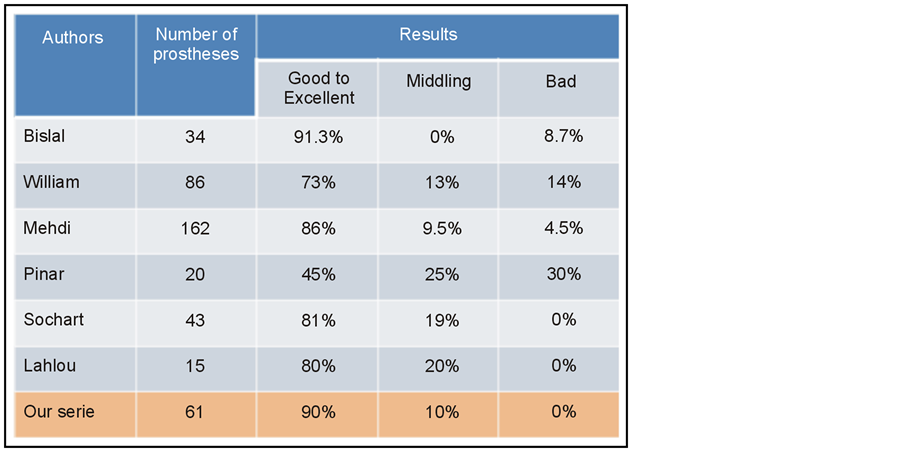
Figure 5. Comparative table of the functional result of the various series.
5. Conclusion
The advent of total hip prostheses has changed the future of patients with crippling coxites on ankylosing spondylitis. The short and medium-term results are brilliant and remarkable, but we cannot ignore their uncertain remote evolution bound to the risk of wear of materials especially with the resumption of an active life. For that purpose, we recommend the preferential use of the hard couples and the preoperative planning of the implementation to optimize at most the longevity of implants.
Funding
No benefits or funds were received in support of this study.
Conflict of Interests
The authors report no conflict of interests.
References
- Caton, J., Courpied, J.P., Ferreira, A., et al. (2004) Total Hip Arthroplasty. 4th Symposium Charnley International Lyon 2004, Lyon, 130-135, 77-78.
- Brinker, M., Rosenberg, A., Cox, D., et al. (1996) Primary Noncemented Total Hip Arthroplasty in Patients with Ankylosing Spondylitis: Clinical and Radiographic Results at an Average Follow-Up Period of 6 Years. The Journal of Arthroplasty, 11, 802-812. http://dx.doi.org/10.1016/S0883-5403(96)80180-X
- Tang, W.M. and Chice, K.Y. (2000) Primary Total Hip Arthroplastiy in Patients with Ankylosing Spondylitis. The Journal of Arthroplasty, 15, 52-58. http://dx.doi.org/10.1016/S0883-5403(00)91155-0
- Joshi, B., Markovic, L., Hardinge, K., et al. (2002) Total Hip Arthroplasty in Ankylosing Spondylitis: An Analysis of 181 Hips. The Journal of Arthroplasty, 17, 427-433. http://dx.doi.org/10.1054/arth.2002.32170
- Bisla, R., Ranawat, C. and Inglis, A. (1976) Total Hip Replacement in Patients with Ankylosing spondylitis with Involvement of the Hip. The Journal of Bone and Joint Surgery (American Volume), 58, 233-238.
- Chen, Y.Q., Ji, Z.Y., Sun, F.X., et al. (2008) Total Hip Arthroplasty for the Treatment of Ankylosing Spondylitis in 11 Cases. Journal of Clinical Rehabilitative Tissue Engineering Research, 12, 48.
- d’Aubigné, M. (1997) Quotation Calculated by the Function of the Hip. Revue de Chirurgie Orthopédique et Réparatrice de l’Appareil Moteur, 56, 481-486.
- Sochart, D.H. and Porter, M.L. (1997) The Long-Term Results of Charnley Low-Friction Arthroplasty in Young patients Who Have Congenital Dislocation, Degenerative Osteoarthrosis, or Rheumatoid Arthritis. The Journal of Bone and Joint Surgery (American Volume), 79, 1599-1617.
- Kilgus, D.J., Namba, R.S., Gorek, J.E., et al. (1990) Total Hip Replacement for Who Have Ankylosing Spondylitis. The Importance of the Training of Heterotopic Bone and of the Durability of Fixation of Cemented Components. The Journal of Bone and Joint Surgery (American Volume), 72, 834-839.
- Williams, E., Taylor, A.R., Arden, G.P., et al. (1977) Arthroplasty of the Hip in Ankylosing Spondylitis. The Journal of Bone and Joint Surgery (American Volume), 59, 393-397.
- Walker, L.G. and Cement, B. (1991) Total Hip Arthroplasty in Ankylosing Spondylitis. Clinical Orthopaedics and Related Research, 262, 198-204.
NOTES
*Corresponding author.

