Open Journal of Anesthesiology
Vol.3 No.5(2013), Article ID:34937,9 pages DOI:10.4236/ojanes.2013.35058
Teaching Ultrasound Imaging for Central Line Placement—A Resident’s Perspective
![]()
Loyola University Medical Center, Anesthesiology, Maywood, USA.
Email: *jmukher@lumc.edu
Copyright © 2013 Jayanta Mukherji et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received April 22nd, 2013; revised May 26th, 2013; accepted June 19th, 2013
Keywords: Ultrasound-Guided Technique; Vascular Access; Guidelines; Resident’s Perception
ABSTRACT
The availability of ultrasound (US) devices has refined techniques for vascular access. The resident trainee’s ability to learn US techniques depends upon device availability, skills, and motivation of instructors. We hypothesized that hands-on teaching program of US techniques for vascular access would have a positive impact on the trainee’s perceptions. After IRB approval, PGY3 anesthesiology residents with limited prior experience in US-guided vascular access underwent close supervision by attending staff as they performed US-guided Internal Jugular Vein (IJV) central line placements. A total of 66 land mark (LM) and 75 US-guided IJV cannulation performed by 19 residents were supervised. Residents completing the study were more proactive with 68.4% agreeing to use US based techniques for an anticipated difficulty in accessing central lines. The graduating residents involved in the study all strongly agreed that US imaging for vascular access was within the scope of practice of all anesthesiologists, and that training guidelines be established and incorporated in their practice. Fifty eight percent of residents stated that their confidence and skill levels had significantly improved. Teaching US-guided techniques resulted in an increase employment of such techniques by graduating residents with no impediment attributed to knowledge deficits or inexperience. Residents were more proactive with using US for anticipated difficulty in IJV placement. A short neck, poor landmark, anticoagulation, morbid obesity favored US use by residents. Systematic teaching of US techniques is justified as it significantly improves the resident’s perceptions and confidence.
1. Introduction
Central venous cannulation (CVC) is one of the most commonly performed procedures used by anesthesiology residents. Traditionally anesthesiology residents in teaching institutions have relied on anatomical landmarks (LM), which was the standard practice available for securing central lines. However, with the rapid proliferation and easier availability of ultrasound devices there are now numerous applications available for vascular access. Numerous studies have demonstrated the advantages of utilizing ultrasound for central line placement [1,2]. The use of ultrasound (US) has been described as less traumatic and is associated with a higher successful insertion rate, an improved first-pass and lower complication rate [3].
Although the use of US has been endorsed by various medical organizations, such as the Agency for Health Care Research and Quality, not all physicians have transitioned to using US guidance routinely in clinical practice. The use of ultrasound guidance for vascular access has been less consistent and may vary depending upon availability of the device, experience and skills of the instructor and the motivation of the teaching program to supervise and provide hands-on instructions and feedback to residents. In our study, we hypothesized that a comprehensive teaching module that incorporates handson teaching of ultrasound techniques for vascular access would positively impact the trainee’s attitudes and skills in using US in their future practice. The aim of the study was to evaluate resident perceptions regarding the use of US for internal jugular vein (IJV) cannulation before and after completion of the teaching program. In the study, the PGY3 residents initially performed the LM technique for central line placement prior to attempting US-guided placement. This served as a baseline to objectively assess and compare their ability with the less familiar US technique.
2. Methods
The study was conducted after IRB approval of Loyola University Medical Ctr. Twenty anesthesiology residents at the beginning of their PGY3 year, were involved in the study. They had limited knowledge and experience with use of ultrasound devices for line placement and were sufficiently comfortable using traditional landmark guided approaches. All residents participating in the study first attended an ultrasound workshop focusing on principles of ultrasound, image and probe adjustment, longitudinal and transverse scanning of internal jugular vessels, and puncturing of vessels.
The residents then placed internal jugular (IJ) central lines in patients where a central line was indicated after induction of general anesthesia (GA). This was performed on at least three or more occasions using traditional anatomical landmarks (LM CVC) with palpation and Seldinger technique. During performance of LM CVC the neck of patient was rotated to the opposite side and the patient was placed in trendelenburg position. A seeker needle was used initially after locating carotid artery pulsations and attempting the needle stick lateral to the pulsation. An introducer needle with cannula was used to access the vein and followed the same trajectory of the seeker needle when dark venous blood was aspirated. In all procedures final confirmation of venous cannulation was obtained by the transduction of the cannula.
Each resident then performed at least three or more US-guided IJV line placements (US CVC) which were closely supervised by a designated anesthesiology attending in the OR. Residents were trained in dynamic (real time) US CVC placements using a sonosite (MicroMaxx®), which allowed visualization to guide the needle into the vein. The sonosite probe was lowered in a sterile sheath after application of sterile gel. A seeker needle was not used in US CVC. Only a needle introducer was used after identifying the vein on US in a transverse axis. The US CVC was placed either using a one-person technique (one hand to hold the US probe and other to place the line) or a two-handed technique (one operator to hold the US probe and one operator to place the line) depending on the discretion of the resident. Once a blood flash was obtained the CVC was placed using the Seldinger technique similar to the LM CVC method. The time required to setup the US machine and set up the probe was not recorded. The attending anesthesiologist had the discretion to stop the procedure at any time the procedure performed was deemed unsafe or technically incorrect.
If the resident was unable to insert the central line with multiple attempts the placement would be considered a failure and the procedure would be attempted at a different site or converted to a US CVC method.
All IJV (both LM CVC and US CVC) were placed under anesthesiology attending supervision. The procedure was timed with a stopwatch with the start time recorded as the time the needle first penetrated the skin. The procedure end-times were recorded as time to successful venous cannulation, and time to successful placement of the central venous catheter. Other particulars included the nature of surgery, patient characteristics, type of central line placed, position of the neck, number of attempts made with introducer needle, incidence of complications such as arterial puncture, neck hematoma, degree of difficulty in CVC placement and the time taken for venipuncture and central line placement.
Each resident also completed a questionnaire before beginning their US training for vascular access and at the time of graduation from residency. The questionnaire recorded their perceptions regarding US CVC and includeed their valid indications for using US, overall difficulty using US CVC, obstacles to using US-guided techniques in their clinical practice, specific clinical conditions prompting the use of US CVC, and their general perceptions regarding the need for a curriculum for US training for vascular access. Changes in their perception before and after undertaking the US study were noted.
3. Statistical Considerations
The main outcome of interest is change in ‘perception’ measure on a Likert scale [1-5] from baseline (before training). We anticipate that the average perception score at baseline will be 3.5 and it will change to 4.5. A paired t-test will be used for comparison of the two time points, adjusting for baseline score. Other outcome measures corresponding to the aims of the study will be analyzed. The measures include learning skills (time it takes to perform the procedure), number of attempts, and change in clinical practice (measure in 1.5 Likert scale).
4. Results
A total of twenty PGY 3 residents were supervised and received hands-on training for the US study. Each resident first performed 3 LM CVC or more for a total of 66 LM cases and then completed 3 or more US CVC cases for a total of 75 cases. A total of 141 LM and US cases were supervised.
The patient was positioned after induction of GA in the trendelenburg position with the neck extended and rotated to the opposite direction prior to line placement in all cases. There was no difference in the incidence of trendelenburg positioning, neck extension and rotation in both LM groups and US. In our study the seeker needle was used first followed by the introducer needle for localizing the IJ in LM cases whereas in US cases only the introducer needle was used for the purpose of IJ access. In 69.7% of LM cases two or more attempts were made with the seeker needle to obtain a blood flash (Figure 1).
When the number of attempts made with the introducer needle was compared in both groups there was a higher incidence of patients in the LM group who required three (p = 0.016) or greater attempts (p = 0.073) (Figure 2).
The incidence of arterial punctures using an introducer needle demonstrated a higher trend in the LM group although it was not statistically significant. (p = 0.078 for single arterial puncture). Failure of CVC placement necessitated a change in the site of line placement and this was not different in between the groups. Other complications such as the incidence of neck hematoma following attempted or successful line placement had a similar incidence (p = 0.818) and no pneumothorax was reported. A fairly significant percentage of cases 49% in the US group requested help from a supervisor for
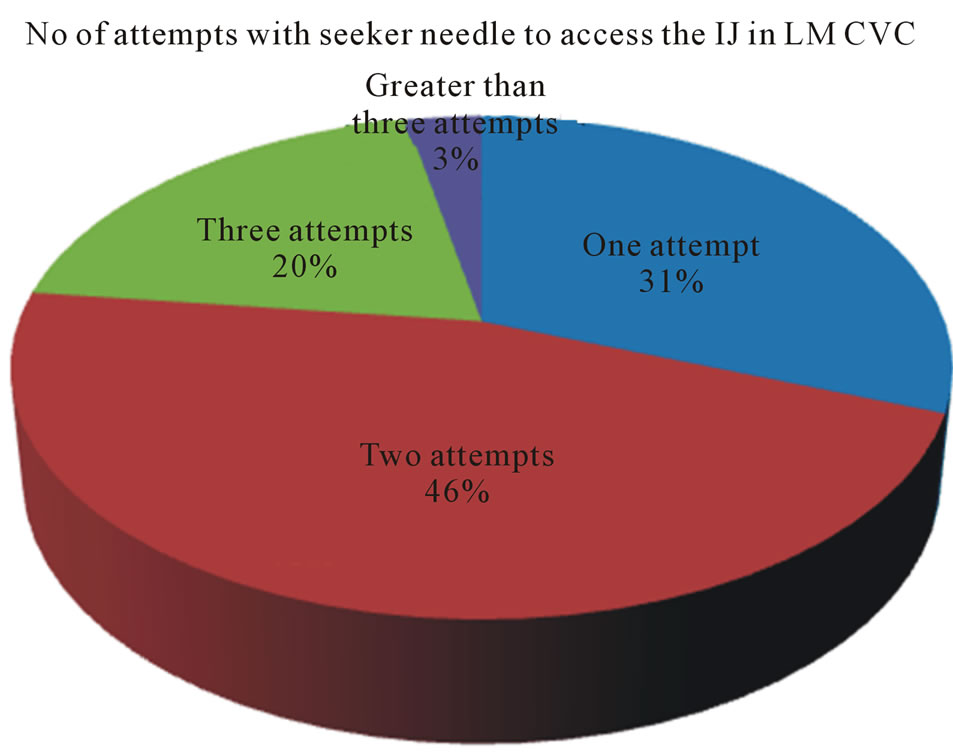
Figure 1. Number of attempts with seeker needle to access the IJ in LM CVC.
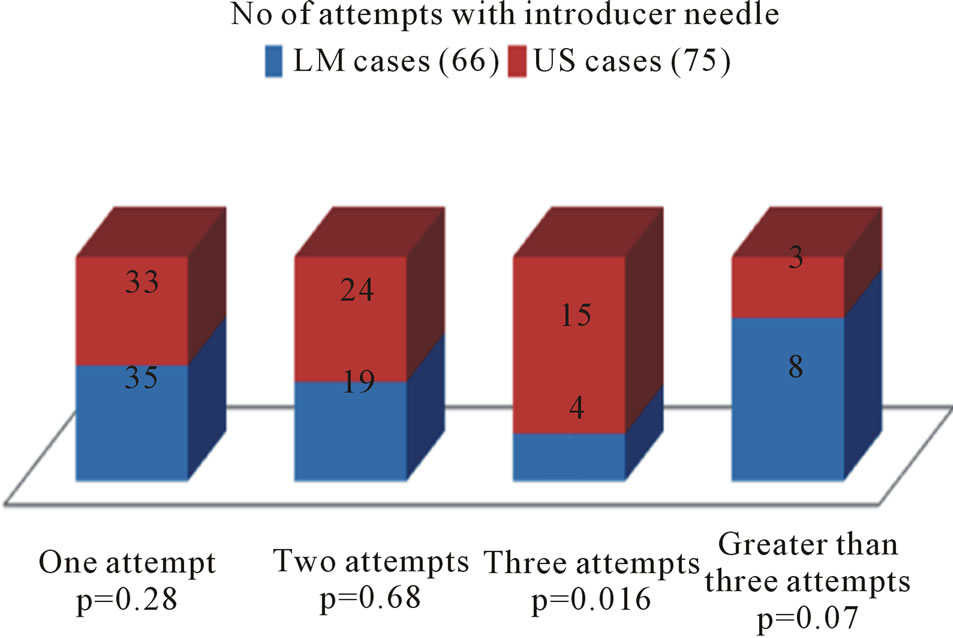
Figure 2. Number of attempts with introducer needle.
successful CVC placement and this was significantly more than in the LM group (24%). (p = 0.02) (Figure 3).
During the learning process of US CVC residents encountered difficulty in identifying the IJ using US in 16% of cases. However, the difficulty was primarily confined during their learning encounters on the first two occasions (9%). With identification of IJ its relationship with the carotid artery was noted a majority of time (45%) the IJ was positioned anterolateral to the carotid artery.
Although all CVC placements were confirmed by transducing the vessel, the US probe was used to check the presence of the guidewire in the IJ. However, the guidewire could be clearly located in the IJ lumen in only 58.6% of cases on a preliminary exam. Additional information obtained from US examination was the presence of intravascular clots in the IJ (Figure 4).
During the process of analyzing physical neck characteristics, we identified neck characteristics and obesity as possible factors, which is likely to make CVC placement difficult. These included poor anatomical landmarks such as a less prominent sternocleidomastoid (SCM), a short neck (measured from hyoid cartilage to jugular notch) and BMIs (above 30). The above-mentioned physical characteristics, which were presumed to make CVC placement more demanding, were comparable in both groups (Figure 5).
The time taken for venipuncture (measured from start
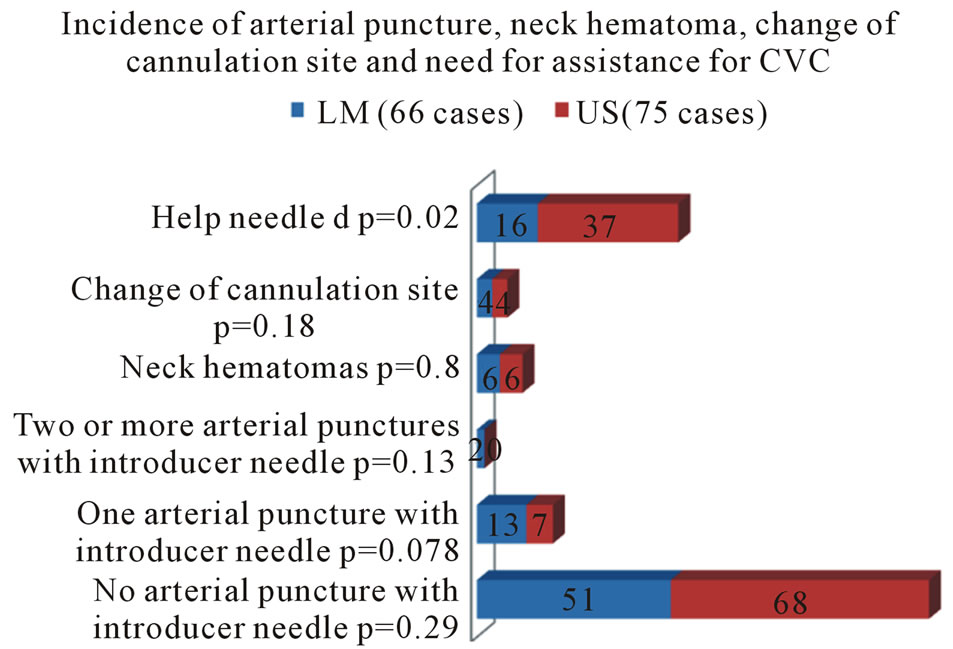
Figure 3. Incidence of arterial puncture, neck hematoma, change of cannulation site and need for assistance for CVC.
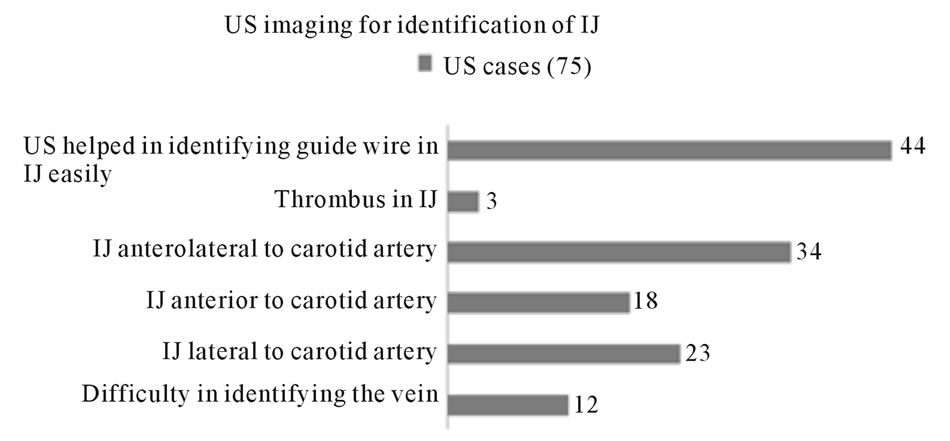
Figure 4. US imaging for identification of IJ.
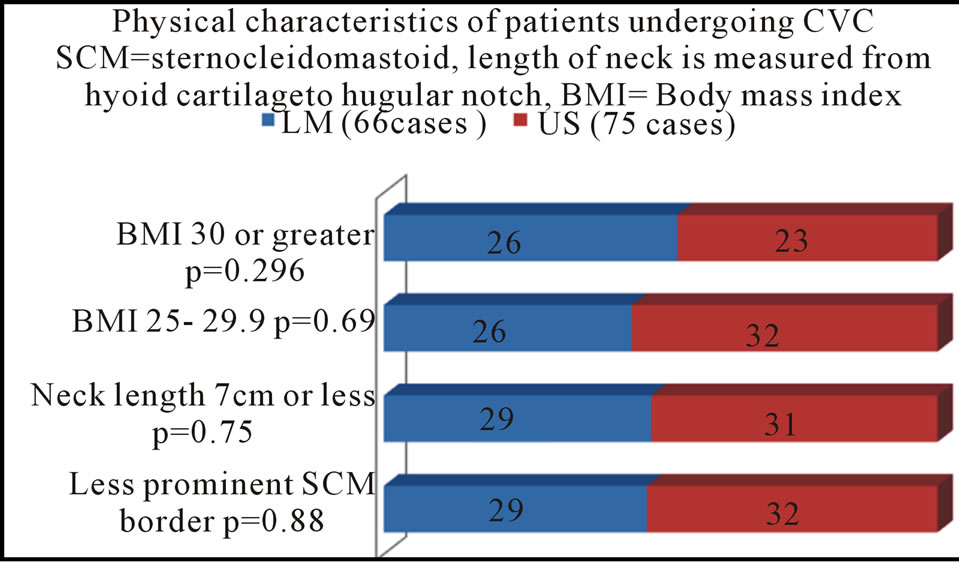
Figure 5. physical characteristics of patients undergoing cvc.
of needle stick to successful placing the cannula and for completion of CVC placement (measured from start of needle stick to successful placement of CVC) was compared. The majority of venipunctures were obtained in less than 1 minute (LM 45%, US 48%) and in most cases total time taken for CVC placement was between 2 to 3 minutes (LM 41%, US 41%). Analysis showed no statistical difference or time advantage.
Residents documented the degree of difficulty in placing CVC, which was based on a Likert scale. The majority of line placements were perceived to be extremely easy (1.5 or less) in both LM (41%) and US groups (43%). In other categories, which included easy (2.0), difficult (2.5 to 3) and considerably difficult (3.5 or greater) there was no difference between groups.
The residents’ perception of the grade of difficulty was compared with physical neck characteristic such as short neck (less than 7 cm), obesity with BMI exceeding 30 or greater, multiple attempts with introducer needle exceeding more than 2, presence of neck hematoma and total time to place CVC exceeding three minutes. The cases regarded by residents as difficult and considerably difficult were analyzed for both LMCVC and US CVC cases (Figure 6).
We noted that the physical characteristics of the patients graded difficult by residents were not different with respect to use of LM or US technique. 41% and 44% of patients graded difficult LM and US procedures respectively had a BMI ≥ 30, and a short neck (less than 7cm) featured in 35% of difficult LM and 38% of difficult US procedures. 36% of graded difficult LM cases, as compared to 61% of graded difficult US cases exceeded 3 minutes for duration of CVC placement (p = 0.024).
In patients categorized considerably difficult for CVC placement by LM method, we noted that 75% of them had an increased duration of CVC placement (>3 minutes), 63% had inadvertent arterial punctures, and 50% possessed shorter necks. Whereas patients in the
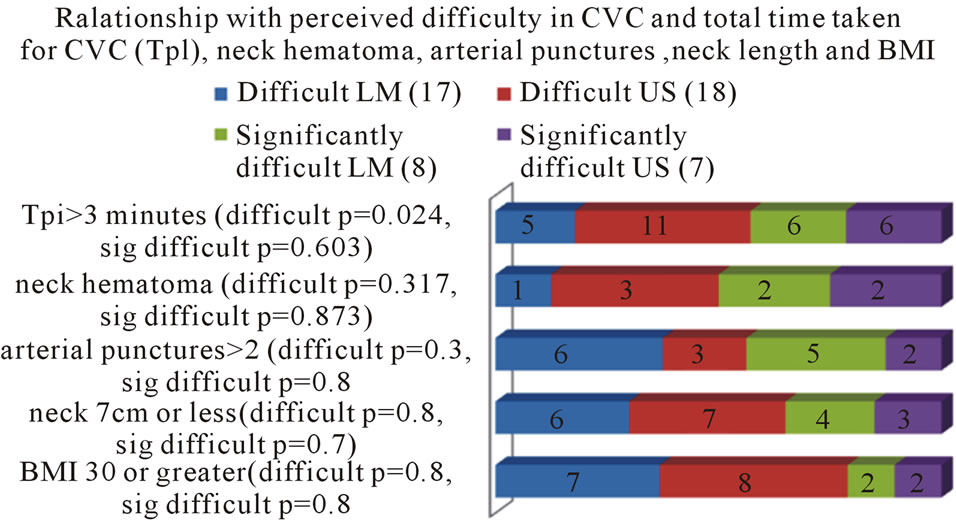
Figure 6. Relationship with perceived difficulty in CVC and total time taken for CVC (Tpl), neck hematoma, arterial punctures, neck length and BMI.
considerably difficult CVC placement category by US method, 86% of them needed a longer duration (> 3 minutes) for CVC placement, and 43% had short necks. Surprisingly only a smaller percentage 25% and 28% of patients graded considerably difficult LM and US cases respectively by residents had an associated BMI ≥ 30 (Figure 6).
4.1. Resident’s Perceptions Regarding US Guided CL Placements Based on Questionnaires
75 US guided internal jugular vein cannulations were performed and 19 residents participated in the questionnaire. Questionnaires were completed before the study and at the time of graduation from residency. Prior to the study, the majority of residents were involved in approximately 0 - 2 ultrasound-guided placements. By the time of graduation the residents had completed an average of 10 to 30 US guided central line placements with an overall increase in 30% since inception of the study.
4.2. When Would Residents Prefer Using US
Before the study, 52.6% of residents considered using US for anticipated difficult central line placement with 36.8% agreeing to use US only if they were unsuccessful with the landmark technique. Residents completing the study were more proactive with 68.4% agreeing to use US based techniques for anticipated difficulty in accessing central lines. Only 5.3% of residents considered using an US technique after they had exhausted their ability to place a central line with the landmark technique (Figure 7).
4.3. Overall Difficulty in Placing Central Lines Using US by Residents
The overall degree of difficulty in placing central lines using US was graded with a Likert Scale (1 [least difficult] to 5 [most difficult]). The residents perceived
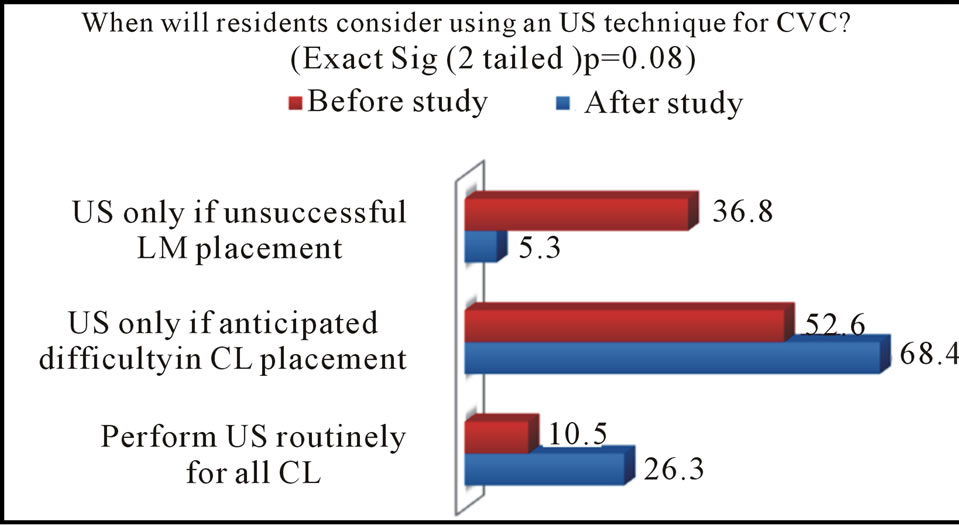
Figure 7. When will residents consider using an US technique for CVC?
an overall decrease in difficulty in placing CL using US technique with a decline in mean score from 2.34 to 2.079 (p = 0.37) (Figure 8).
4.4. Barriers to Implementing US in Clinical Practice
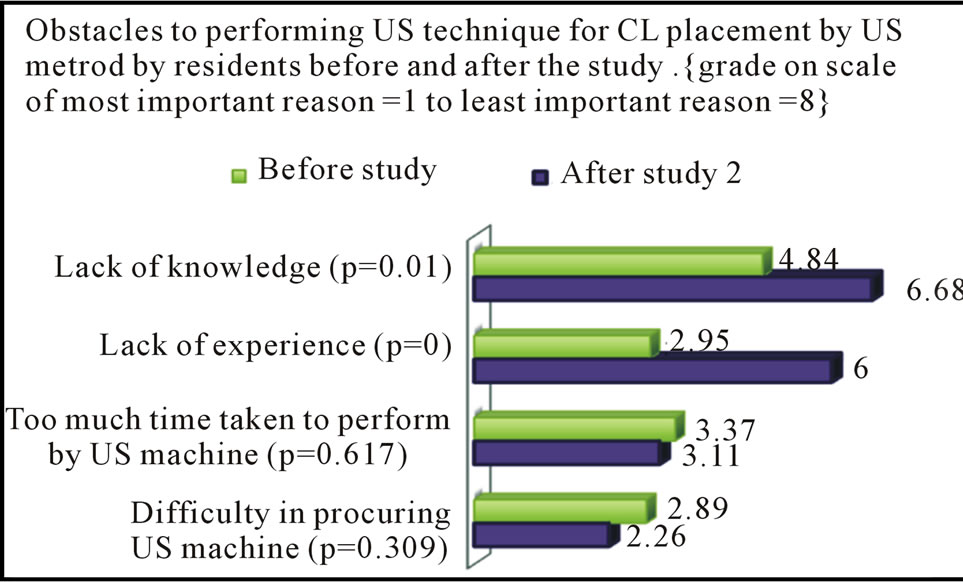
The residents also ranked various criteria anticipated as being an impediment to the placement of a CVC by US technique. These were graded from the most important reason (1) to the least important reason (8).
Prior to the study, residents accounted the following as the most important reasons for being dissuaded in placing central line by US: lack of knowledge with US in 26.4% of residents, lack of experience 52.6% of residents, difficulty in obtaining an US machine in the OR in 36.8% of residents, perceived time-consuming procedure by 10.5% residents, effort not worth the time with landmark techniques being quicker and easier by 5.2% residents. Post study, none of the residents considered impaired knowledge (p = 0.01) or inexperience as a barrier to the use of US machine.
There were no significant changes in resident’s perception with regards to other criteria incorporated as obstacles to the use of US. However, residents did acknowledge that US was a less worthwhile pursuit, as they were confident enough in placing CVC with the LM method (p = 0.01) (Figures 9(a), 9(b)). The foremost hindrance to performing US mediated line placements post-study were related to difficulty in quick procurement of an US machine as reported by 42% of residents.
Headings, or heads, are organizational devices that guide the reader through your paper. There are two types: component heads and text heads.
4.5. Clinical Conditions Prompting the Use of US Technique
The graduating residents involved in the study cited the following clinical conditions as substantial reasons for employing an US based technique for vascular access:
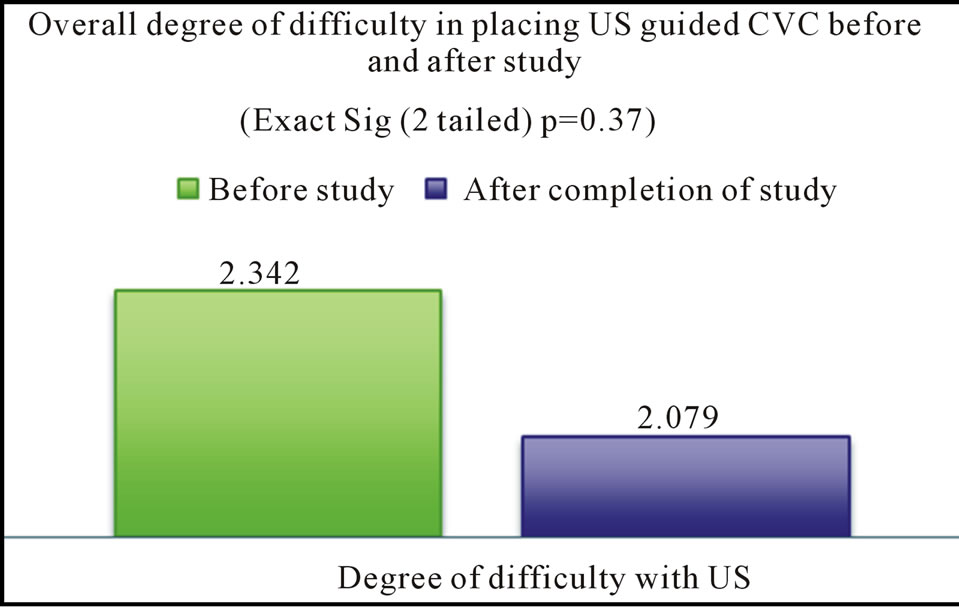
Figure 8. Overall degree of difficulty in placing US guided CVC before and after study.
 (a)
(a)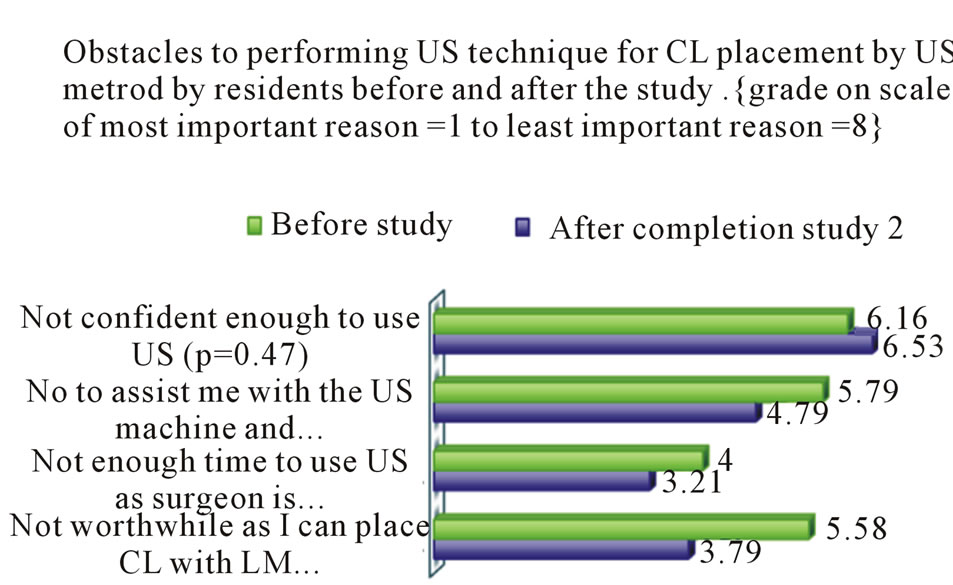 (b)
(b)
Figure 9. (a): Obstacles to performing US technique for CL placement by US method by residents before and after the study; (b): Obstacles to performing US technique after CL placement by US method by residents before and after the study.
short neck (58% residents), neck contractures (57.9% of residents), poor landmarks (74% of residents), anticoagulated patients (68.4% of residents), morbidly obese patients (68.4% of residents), orthopneic patients with inability to lie flat (79% of residents). Following the study there was no difference in the proactive use of US for CVC placement.
4.6. Resident Attitudes Reflected by the Degree of Agreement or Disagreement to General Statements
The graduating residents involved in the study all strongly agreed that US imaging for vascular access was within the scope of practice of all anesthesiologists, and that training guidelines be established and incorporated in their practice. They were of one accord with no changes in perception seen after the study (Paired Samples Test p = 1.0).
More residents after the study considered learning US guided vascular access a useful tool and would be using it in their clinical practice. (Figure 10).
Most residents disagreed with the statement that the US guidance method for vascular access should be used in all patients (Paired Samples Test p = 0.107).
Regarding the use of US in specific patient populations most residents were equivocal about using it routinely for vascular access in patients undergoing cardiac, trauma or transplant surgery (Paired Samples Test p = 0.578).
They somewhat disagreed that the US guidance method for vascular access be only reserved for vascular access if it was inaccessible by LM method (Paired Samples Test p = 0.772).
There was more support post-study for routinely using US routinely in patients where difficult vascular access is anticipated (Figure 11).
Post-study the residents collectively disagreed that US use should be disregarded in view of it being time consuming and technically difficult (Paired Samples Test p = 0.083).
After the study no residents harbored the view that learning US guided technique for central line insertion was a waste of time and may not be useful in their future practice (Paired Samples Test p = 0.042).
4.7. Confidence and Skill Level of Residents Performing US Guided Vascular Assess after Completion of the Study
There was a positive statement from residents with 58% of residents stating that their confidence and skill levels were significantly improved. No resident was impacted negatively at the conclusion of the study.
5. Discussion
The motivation for teaching US guided techniques for IJ cannulation stems from the fact that LM based techniques are not necessarily safe and have been listed with numerous complications. These include accidental arterial punctures (6.3% to 9.4%) which may lead to neck hematomas (0.1% to 2.2%), hemothorax, pneumothorax (0.1% to 0.2%) and injuries to cervico-thoracic ganglion, and phrenic nerves [13-16]. Alternative techniques using
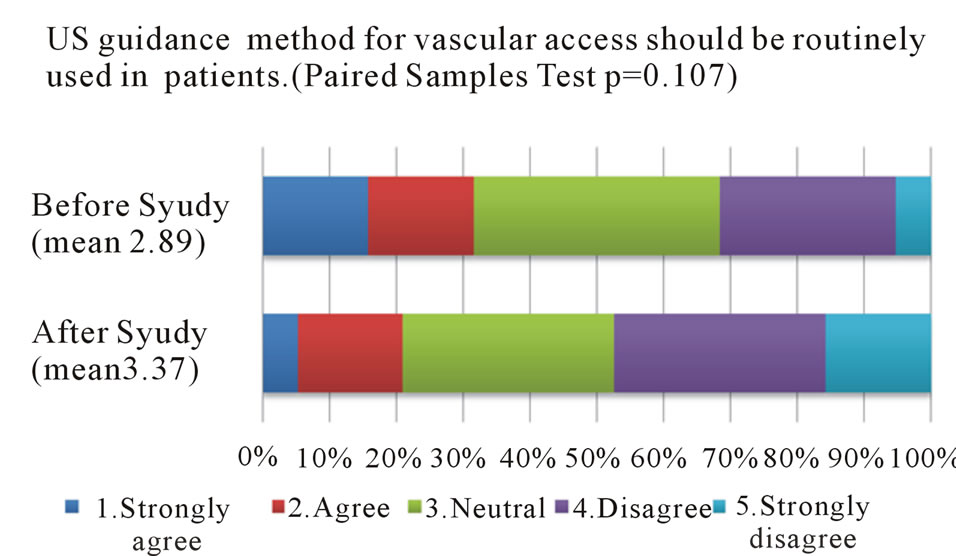
Figure 10. US guidance method for vascular access should be routinely used in all patients (paired samples test p = 0.107).
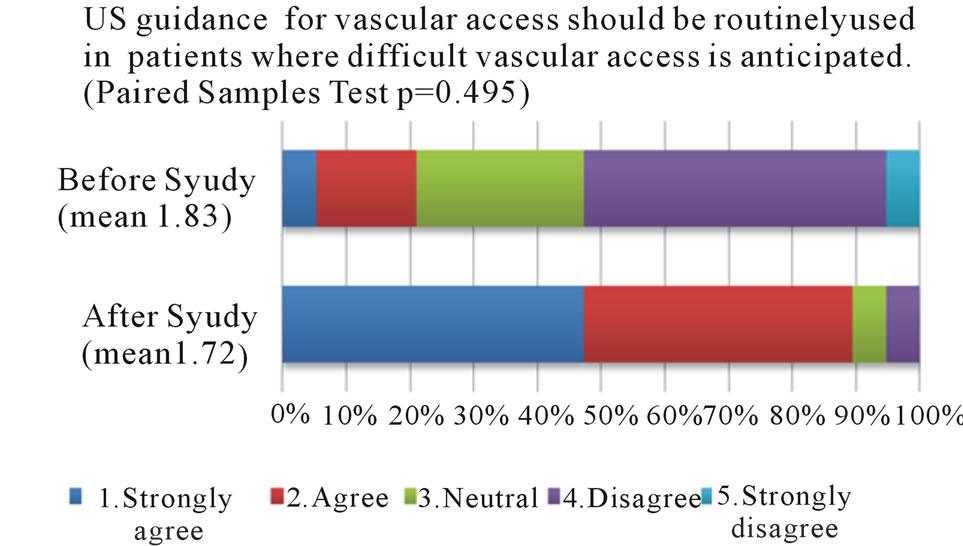
Figure 11. Ultrasound guidance for vascular access should be routinely used in patients where difficult vascular access is anticipated (paired samples test p = 0.495).
US have afforded a higher success rate with decreased attempts and less carotid artery punctures for IJ CVC placement [3,16].
We hypothesize that a systematic, focused approach to teaching of US guided vascular access techniques to anesthesiology residents will result in an change in perception, improve confidence and increase knowledge, judgment and skill levels associated with the employment of such techniques.
Ultrasound imaging and its application for vascular access are being widely adopted by various specialties. The use of US is now within the scope of practice of anesthesiologists and although not widely adopted is now gaining increased acceptance for vascular access [5,6].
A 7.5 mHz linear array transducer was used to identify vascular structures and provided good resolution and adequate penetration. Although color doppler was available it was not used for our study. This study was undertaken as there were no previous training guidelines for resident education and not all anesthesiologists have incorporated CVC placement with US routinely in their practice. Didactic lectures and bedside training with emphasis on US principles, image acquisition and interpretation, eye hand coordination to steady the image was initiated.
Each PGY 3 resident was very familiar with the landmark (LM) technique, but had minimal to no experience or had sporadically used US for CVC placement. For purposes of our study they initially performed three or more LM CVC placements followed by three or more US CVC placements. This allowed us to compare details regarding LM placement including complications with their newfound US CVC techniques. Gaining a procedural skill is usually numbers based. Therefore comparison of LM over US-based techniques in residents while in training may not be truly representative as there is more time to improve their confidence, and skill sets with US. Feller-Kopman recommends 2 hrs of didactics, 2 hrs of exposure to and familiarity with knobology, normal vascular anatomy, and hands-on simulation with vascular access models with 5 - 7 proctored procedures on vascular access models/ simulators. In our study we did not employ models or simulators. Each resident performed at least three US CVC placements that were closely supervised. Twenty residents performed a total of 75 US studies. Even after completing the documented US CVC placements, residents in their fourth year continued to maintain their US experience and this was reflected in their questionnaire completed at the time of graduation.
A rapid learning curve for US CVC placements was noted in PGY3 residents already familiar with LM CVC techniques. Difficulty in imaging the IJ was initially encountered by residents in only 16% of cases and this was mainly confined to their first two cases. Various parameters were measured in both LM CVC and US CVC cases. In both LM and US cases there were no differences in patient factors, which were considered to be adverse such as shorter neck (less than 7 cm), less prominent sternocleidomastoid and BMI ≥ 30. Intravascular volume status, patient positioning and head rotation are factors that can influence the procedure of cannulation [18,19]. In both LM and US groups similar percentages of patients were positioned with neck extension and rotation greater than 15 degrees and trendelenberg exceeding 30 degrees.
A seeker needle was used only for LM cases with 3 or more attempts being required for 23% of LM cases. The number of attempts with the introducer needle needed to aspirate blood was documented in both LM and US based techniques. With US CVC techniques a higher percentage of cases required three attempts when compared to LM CVC cases. However, there was a trend showing a larger percentage of LM CVC cases requiring greater than 3 attempts when compared to US CVC cases. We anticipate that as the residents move up on the learning curve they will gain more dexterity with US leading to a drop in the number of attempts with the introducer needle.
Also, no differences were noted with adverse events related to arterial punctures with introducer needles, the incidence of neck hematomas or need to change cannulation site. Change of site was employed if there was a neck hematoma or if cannulation of IJ was unsuccessful. US imaging of IJ conferred advantages by allowing visualization of vascular structures in real-time. We observed the close relationship of the IJ with the carotid artery with the vein being anterolateral to the artery in 45% of cases performed. Differences have been reported regarding the position of the IJV in relation to the common carotid artery and a constant anatomic position of the IJV does not exist [7]. Using US would have more appeal when the vein overlies the artery, as direct visualization would avoid inadvertent arterial punctures after penetrating through the vein. In our study intra-vascular clots were visualized in 4% of cases, which precluded use of the site.
We used only the short axis view, as this was easier to learn for beginners than a technique using longitudinal scans. Cross-scan views also provided a better view of the surrounding structures but puncturing a vessel is a possibility as the hyperechoic signal from the needle does not provide the operator any clue regarding the location of the tip of the needle. These limitations in US guided techniques were reported in a study by Blaivas et al. who observed residents with limited US experience placing US-guided catheters in a human torso mannequin using a cross sectional approach [17]. In their study 64% of residents accidentally penetrated the posterior wall of the IJ and in 5 cases the carotid artery was mistakenly penetrated. In addition, to more experience with USguided catheters, using alternate US guidance techniques such as visualization of vein and needle in a longitudinal axis was also suggested.
When times to venipuncture and successful placement of the US catheter were compared, there were no statistical difference seen with the LM and US based CVC techniques. In the majority of patients in LM (45%) and US (48%) cases, the IJ was accessible by venipuncture in less than a minute. In 41% of both LM and US cases there were no differences seen in successful IJC placement, which was achieved between 2 to 3 minutes. A prospective observational cohort study by Froehlich et al. evaluating US guided CVC placement in a pediatric ICU setting noted a similar success rates and time to placement [8]. They however recorded fewer numbers of attempts (p = 0.001) and less inadvertent arterial punctures (p = 0.03) with US base CVC. Numerous other studies conducted with US guided catheter placements have shown that US assistance has reduced the mean number of attempts to cannulate the vein as well as a significant time reduction in the procedure [9-12]. No advantages were accrued in our study with regard to time management as a significant number of residents needed help from attending anesthesiologist for US CVC when compared to LM CVCs (p = 0.002). Help was sought in 49.3% of cases performed by US. This was anticipated as the residents were inexperienced and needed familiarity with handling of the US transducer and operating the introducer needle simultaneously.
After performing an IJV placement, residents evaluated the grade of difficulty of central line placement using a Likert scale. We noted that LM or US cases perceived as “difficult” or “significantly difficult” by residents showed no differences when compared with patient’s anatomic characteristics, BMI > 30, neck length less than 7 cm. Also when compared with procedural difficulties such as arterial punctures on 2 occasions or neck hematomas, both US and LM based techniques showed similar grades of difficulty. However, a higher percentage of ‘difficult cases’ in the US group required a longer time (exceeding 3 minutes) for placement of central line when compared to the LM group (p = 0.024).
A systematic focused approach to teaching US guided vascular access techniques resulted in an increase in the employment of such techniques by graduating residents. By gaining familiarity with US device, principles and technique all residents assumed increased confidence with no impediment attributed to knowledge deficits or inexperience with US.
However, most residents did not favor the routine use of US in vulnerable populations undergoing cardiac, trauma or transplant surgery. In fact a sizeable number of residents (68.4%) would reserve its use for anticipated difficulty in central line placement. The majority of residents agreed that underlying conditions such as a short neck, poor landmarks with neck contractures, anticoagulation, and morbid obesity would be significant reasons prompting them to use US techniques.
The study resulted in residents being more proactive in using US and not considering its use by default if conventional landmark placement was unsuccessful. Evaluations both before and after the study showed that 42% of residents considered US use as a time consuming process. Even if the residents achieved proficiency in technique there were other delays to contend with. Most delays were related to the logistics of procuring US machine in a timely manner, and preparation time with application of a sterile sheath for the probe as well as powering and optimal setting of the US machine. These were valid reasons for forgoing this technique in favor of a landmark method during routine central line placements. A majority of residents (58%) agreed that a systematic curriculum of teaching US techniques significantly improved their level of confidence and function with US based techniques.
We have demonstrated that systematic supervision and teaching of residents does increase exposure, and improve confidence and competence. We however cannot assume that the complication rate from US guided CVC will be lowered. Martin et al. noted that the complication profile was not affected by ultrasound use, patient factors, or resident year in training. There was a higher complication rate associated with procedures performed at night that may be caused by resident fatigue or unavailability of senior supervision [20]. This suggests that there are other variables beyond teaching US which could adversely influence the complication rates in CVC.
REFERENCES
- A. G. Randolph, D. J. Cook, C. A. Gonzales and C. G. Pribble, “Ultrasound Guidance for Placement of Central Venous Catheters: A Meta-Analysis of the Literature,” Critical Care Medicine, Vol. 24, No. 12, 1996, pp. 2053- 2058. doi:10.1097/00003246-199612000-00020
- D. Hind, N. Calvert, R. McWilliams, A. Davidson, S. Paisley, C. Beverley and S. Thomas, “Ultrasonic Locating Devices for Central Venous Cannulation: Meta-Analysis,” British Medical Journal, Vol. 327, No. 7411, 2003, p. 361. doi:10.1136/bmj.327.7411.361
- J. Leung, M. Duffy and A. Finckh, “Real-Time Ultrasonographically-Guided Internal Jugular Vein Catherization in the Emergency Department Increases Success Rates and Reduces Complications: A Randomized, Prospective Study,” Annals of Emergency Medicine, Vol. 48, No. 5, 2006, pp. 540-547. doi:10.1016/j.annemergmed.2006.01.011
- D. Feller-Kopman, “Ultrasound-Guided Internal Jugular Access A Proposed Standardized Approach and Implications for Training and Practice,” Chest, Vol. 132, No. 1, 2007, pp. 302-309. doi:10.1378/chest.06-2711
- S. Howard, “A Survey Measuring the Impact of NICE Guidance 49: The Use of Ultrasound Locating Devices for Placing Central Venous Catheters,” 2004. http://www.nice.org.uk/pdf/Final_CVC_placement_survey_report.pdf
- S. Ruesch, B. Walder and M. Tramer, “Complications of Central Venous Catheters: Internal Jugular Versus Subclavian Access: A Systematic Review,” Critical Care Medicine, Vol. 30, No. 2, 2002, pp. 454-460. doi:10.1097/00003246-200202000-00031
- M. Salman, M. Potter, M. Ethel, et al., “Recurrent Laryngeal Nerve Injury: A Complication of Central Venous Catheterization: A Case Report,” Angiology, Vol. 55, No. 3, 2004, pp. 345-346. doi:10.1177/000331970405500316
- M. Ohlgisser and M. Heifetz, “An Injury of the Stellate Ganglion Following Introduction of a Canula into the Inner Jugular Vein (Horner’s Syndrome),” Anaesthesist, Vol. 33, No. 7, 1984, pp. 320-321.
- S. T. Verghese, W. A. McGill, R. I. Patel, et al., “Comparison of Three Techniques for Internal Jugular Vein Cannulation in Infants,” Pediatric Anesthesia, Vol. 10, No. 5, 2000, pp. 505-511. doi:10.1046/j.1460-9592.2000.00554.x
- T. D. Girard and J. M. Schectman, “Ultrasound Guidance during Central Venous Catheterization: A Survey of Use By House Staff Physicians,” Journal of Critical Care, Vol. 20, No. 3, 2005, pp. 224-229. doi:10.1016/j.jcrc.2005.06.005
- P. Armstrong, R. Sutherland and D. Scott, “The Effect of Position and Different Maneuvers on Internal Jugular Vein Diameter Size,” Acta Anaesthesiologica Scandinavica, Vol. 38, 1994, pp. 229-231. doi:10.1111/j.1399-6576.1994.tb03879.x
- C. Sulek, N. Gravenstein, R. Blackshear, et al., “Head Rotation During Internal Jugular Vein Cannulation and the Risk of Caratid Artery Puncture,” Anesthesia & Analgesia, Vol. 82, No. 1, 1996, pp. 125-128.
- T. Maecken and T. Grau, “Ultrasound Imaging in Vascular Access,” Critical Care Medicine, Vol. 35, Suppl. 5, 2007, pp. S179-S185.
- M. Blaivas, L. Brannam and E. Fernandez, “Short-Axis Versus Long-Axis Approaches for Teaching UltrasoundGuided Vascular Access on a New Inanimate Model,” Academic Emergency Medicine, Vol. 10, No. 12, 2003, pp. 1307-1311. doi:10.1111/j.1553-2712.2003.tb00002.x
- C. D. Froehlich, M. R. Ridby, E. S. Rosenberg, R. Li, et al., “Ultrasound-Guided Central Venous Catheter Placement Decreases Complications and Decreases Placement Attempts Compared with the Landmark Technique in Patients in a Pediatric Intensive Care Unit,” Critical Care Medicine, Vol. 37, No. 3, 2009, pp. 1090-1096. doi:10.1097/CCM.0b013e31819b570e
- L. Oguzkurt, F. Tercan, G. Kara, D. Torun, O. Kizilkilic and T. Yildirim, “US-Guided Placement of Temporary Internal Jugular Vein Catheters: Immediate Technical Success and Complications in Normal and High-Risk Patients,” European Journal of Radiology, Vol. 55, No. 1, 2005, pp. 125-129.
- B. G. Denys, B. F. Uretsky and P. S. Reddy, “Ultrasound Assisted Cannulation of the Internal Jugular Vein: A Prospective Comparison to the External Landmarkguided Technique,” Circulation, Vol. 87, No. 5, 1993, pp. 1557- 1562. doi:10.1161/01.CIR.87.5.1557
- D. L. Mallory, W. T. McGee, T. H Shawker, et al., “Ultrasound Guidance Improves the Success Rate of Internal Jugular Vein Cannulation: A Prospective, Randomized Trial,” Chest, Vol. 98, No. 1, 1990, pp. 157-160. doi:10.1378/chest.98.1.157
- C. A. Troianos, D. R. Jobes and N. Ellison, “Ultrasoundguided Cannulation of the Internal Jugular Vein: A Prospective, Randomized Study,” Anesthesia & Analgesia, Vol. 72, No. 6, 1991, pp. 823-826. doi:10.1213/00000539-199106000-00020
- M. J. Martin, F. A. Husain, M. Piesman, P. S. Mullenix, S. R. Steele, C. A. Andersen and G. N. Giacoppe, “Is Routine Ultrasound Guidance for Central Line Placement Beneficial? A Prospective Analysis,” Journal of Current Surgery, Vol. 61, No. 1, 2004, pp. 71-74. doi:10.1016/j.cursur.2003.07.010
NOTES
*Corresponding author.

