Open Journal of Anesthesiology
Vol.2 No.4(2012), Article ID:22227,3 pages DOI:10.4236/ojanes.2012.24023
A Case Study in the Use of Capsaicin in the Treatment of Neuropathic Chest Wall Pain and Post-Thoracotomy Intercostal Neuralgia
![]()
Department of Anesthesiology and Interventional Pain, LSU Health Science Center School of Medicine, Shreveport, USA.
Email: crob16@lsuhsc.edu
Received May 31st, 2012; revised July 21st, 2012; accepted August 12th, 2012
Keywords: Post-Thoracotomy Neuralgia; Capsaicin; Qutenza®
ABSTRACT
Off label use of Quetenza® (capsaicin 8%) patch in relieving post-thoracotomy neuropathic pain proved temporarily effective, but to a degree indicating limited usefulness in a clinical setting. A 57 year-old male with chronic post-thoracotomy pain was treated with 8% capsaicin topically. Pre-procedure pain was rated as 8 on a 10 point scale, the 30 minute post procedure pain was reported as 2 - 3 on a 10 point scale. Neuralgia was completely resolved for the initial 48 hours post-procedure, then returned gradually over the next 5 days. Because pain transmission pathways are the same in post herpetic and post traumatic neuralgias, the use of 8% capsaicin merits additional study.
1. Introduction
A 57 year-old male with chronic post-thoracotomy pain was treated with 8% Qutenza® in an off label topical application. Qutenza® patch contains 8% capsaicin (640 mcg/cm2), with each patch containing a total of 179 mg of capsaicin. It has FDA approval for use in the treatment of postherpetic neuralgia [1].
The goal was to evaluate the effectiveness of Qutenza® for the treatment of neuropathic chest wall pain. Though the initial benefit reported by the patient was excellent, the duration of the response was limited.
1.1. Patient History and Treatment Modalities
The patient is a 57 year-old male previously diagnosed with chronic left chest wall pain and post-thoracotomy (intercostal) neuralgia. The patient was thrown while training a horse April 17, 2010, resulting in fracture of the left transverse process from T6-L5, fracture of spinous process at T4 and T8-T12, fracture at the right inferior endplate of L4 and L5, left clavicle fracture, comminuted left scapular fracture, left pneumothorax, splenic laceration, and multiple left rib fractures (flail chest) (Figure 1). The patient was managed surgically with a left thoracotomy for rib-plating 4-9, chest tube placement, and mechanical ventilation (Figure 2). Subsequent treatment is subject to acceptable modalities mandated in accordance with Workman’s Compensation rules.
1.2. Examination
When seen fourteen months post trauma and surgical intervention, the patient reported a pain score of 8 on a scale of 10, describing it as constant with variable intensity. The pain was qualified as sharp, stabbing, aching (spasmodic), and burning, with radiation from the posterior thorax to the midaxillary and anterior chest wall. Examination of the affected area revealed allodynia and hyperalgesia. Pain management therapies at initial contact included medications: Lortab 10 mg/325 mg one tab
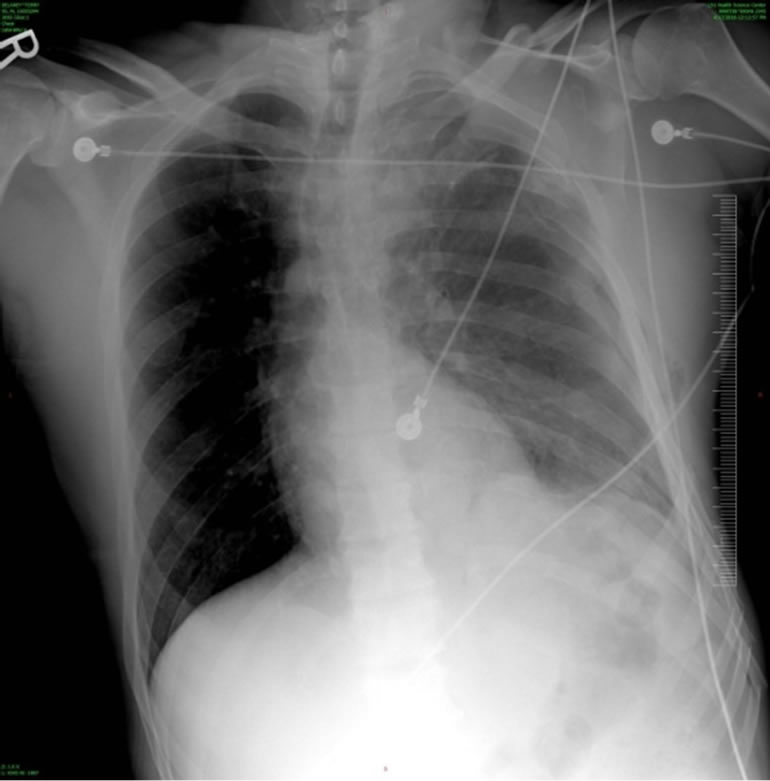
Figure 1. Pre-operative flail chest and pneumothorax.

Figure 2. Post-operative repair.
po prn tid (by mouth, as needed, three times daily), Lyrica 100 mg po tid, amitriptyline 50 mg po at bedtime (Cymbalta administration was denied by Workman’s Compensation manager), and physical therapy. Although the treatment modalities were beneficial, symptoms continued to be progressive and problematic for the patient.
2. Intervention
Interventional options were extensively discussed with the patient and included ON-Q pump placement, intercostal nerve block, and possible spinal cord stimulation. The patient deferred these modalities due to a reported needle phobia. Therefore a high dose 8% capsaicin patch (trade name Qutenza®) was chosen as a trial due to its topical application and consequent avoidance of needles, as well as its feasibility due to reimbursement from Workman’s Compensation.
2.1. Treatment Rationale
Qutenza® (capsaicin) 8% patch is indicated for the treatment of neuropathic pain associated with postherpetic neuralgia. Transient receptor potential vanilloid type 1 (TRPV1) is involved in the peripheral and central mechanisms of visceral sensitization in man. Because capsaicin is known to selectively bind with TRPV1, Qutenza® was selected for trial in an off label administration in postthoractomy neuralgia [2-6].
2.2. Procedure, Materials and Methods
Written informed consent was obtained from the patient. With the patient in a sitting position, the affected region on the left thorax, axilla and anterior chest wall were delineated with a marker. These areas were then cleansed and prepped with chlorohexidine scrub. Regional hair was removed with scissors and paper tape. Lidocaine 4% (EMLA) cream was then applied generously to an approximate 7-inch × 9-inch area on the left thorax, near the incision site. This pre-treatment was administered to reduce the discomfort associated with the application of Qutenza® patch (8% capsaicin). The EMLA cream remained on the affected area for 75 minutes then removed by cleansing with mild soap and water and the skin dried. After the skin preparation was complete, the Qutenza® patch containing 8% capsaicin was cut, tailored, and fitted to the affected area on the left thorax/chest wall. The patch was then covered and secured in place with circumferentially applied gauze dressing for 65 minutes. After completion of the 65-minute application time, the Qutenza® patch was removed. The area was cleansed with cleansing gel provided with the patch, then the remainder wiped off. The skin was then gently washed and dried (Figure 3).
3. Results
The patient reported immediate relief. Pre-procedure pain score was 8 on a 10-point scale; the 30-minute post procedure pain score was 2-3 on the 10-point scale. When seen for evaluation one week post-procedure, the patient reported complete pain relief for the initial 48 hours. The symptoms then gradually returned to the pre-procedure level in the subsequent five days.
4. Discussion
Capsaicin has been proven to be very effective in treating post-herpetic neuralgia. Currently, compound NGX- 4010, 8% topical capsaicin (Qutenza®) is FDA approved for treatment of post-herpetic neuralgia. A single onehour application can provide up to three months of relief

Figure 3. Post capsaicin therapy.
for those suffering from PHN. This therapy is well tolerated, non-invasive and provides a much-needed therapeutic option for those suffering from this type of chronic pain.
Briefly, the mechanism of action of this drug is thought to lie in its ability to selectively stimulate unmyelinated C-fibers and cause the release and subsequent reversible depletion of substance P and possibly other neurotransmitters [7].
While the mechanism of post-thoracotomy pain and resulting intercostal neuralgia is quite different from that of post herpetic neuralgia (physical trauma versus infective), the pain transmission pathways remain the same. It was our hope in this trial that capsaicin would also alleviate the pain associated with this type of neuralgia. While the 8% capsaicin treatment provided a profound reduction in pain for this patient, the results were shortlived, lasting only approximately 48 hours. A literature search for the use of 8% capsaicin for the treatment of intercostal neuralgia did not reveal any results and therefore we wish to bring attention to its potential use for this type of pain.
While further research is necessary regarding the use of capsaicin for this purpose, it holds promise as a potential treatment and at least warrants further study as a therapeutic option in intercostal neuralgia.
REFERENCES
- Prescribing Information, Package Insert, “Qutenza® (Capsaicin) 8% Patch”, Initial US Approval, 2009.
- M. M. Backonja, “High-Concentration Capsaicin for the Treatment of Post-Herpetic Neuralgia and Other Types of Peripheral Neuropathic Pain,” European Journal of Pain Supplements, Vol. 4, No. 2, 2010, pp. 170-174. doi:10.1016/S1754-3207(10)70529-0
- M. M. Backonja, G. A. Irving, L. R. Webster and J. K. Tobias, “Tolerability of Qutenza (NGX-4010), an 8% Capsaicin Patch, for Postherpetic Neuralgia, (A299),” 2010. http:/asaabstracts.com
- C. M. Campbell, R. R. Edwards, C. Carmona, M. Uhart, G. Wand, A. Carteret, Y. K. Kim, J. Frost and J. N. Campbell, “Polymorphisms in the GTP Cyclohydrolase Gene (GCH1) Are Associated With Ratings of Capsaicin Pain,” Pain, Vol. 141, No. 1-2, 2009, pp. 114-118. doi:10.1016/j.pain.2008.10.023
- P. Anand, “Peripheral and Central Mechanisms of Visceral Sensitization in Man,” Neurogastroenterology Motility, Vol. 19, No. 1, 2007, pp. 29-46. doi:10.1111/j.1365-2982.2006.00873.x
- R. Gerwin, “Myofascial and Visceral Pain Syndromes: Visceral-Somatic Pain Representations,” Clinical Neurobiology of Fibromyalgia and Myofascial Pain, Hayworth Press Inc., 2002, pp. 165-175.
- C. H. M. Rains, “Topical Capsaicin. A Review of Its Pharmacological Properties and Therapeutic Potential in Post-herpetic Neuralgia, Diabetic Neuropathy and Osteoarthritis,” Drugs Aging, Vol. 7, No. 4, 1995, pp. 317- 328.

