Open Journal of Epidemiology
Vol. 2 No. 2 (2012) , Article ID: 19108 , 7 pages DOI:10.4236/ojepi.2012.22006
The psychiatric profile of the U.S. patient population across age groups
![]()
1Postgraduate year one (PGY1) resident, Internal Medicine, Kingsbrook Jewish Medical Center, Brooklyn, USA
2Faculty Member, Kuban State Medical University, Krasnodar, Russia
3Personal Life Consultant, PARLEY Personal Life Consulting Services, Macon, USA
Email: *mswalid@yahoo.com
Received 10 January 2012; revised 2 March 2012; accepted 15 March 2012
Keywords: Psychiatric; Diagnosis; Hospital Discharges; Hospital Charges
ABSTRACT
Introduction: As the U.S. population undergoes continuous shifts the population’s health profile changes dynamically resulting in more or less expression of certain psychiatric disorders and utilization of healthcare resources. In this paper, we analyze national data on the psychiatric morbidity of American patients and their summated cost in different age groups. Methods: The latest data (2009) on the number of hospital discharges and national bill (hospital charges) linked with psychiatric disorders were extracted from the Nationwide Inpatient Sample (NIS). Results: National data shows that mood disorders are the largest diagnostic category in terms of percentage of psychiatric-related discharges in the 1 - 17 years age group. The proportion decreases gradually as age progresses while delirium, dementia, amnestic and other cognitive disorders increase exponentially after 65 years of age. Schizophrenia and other psychotic disorders as well as alcohol and substance-related disorders peak in the working age groups (18 - 64 years). From an economic point of view, mood disorders in the 18 - 44 age group has the highest national bill ($5.477 billion) followed by schizophrenic and other psychotic disorders in the same age group ($4.337 billion) and mood disorders in the 45 - 64 age group ($4.310 billion). On the third place come schizophrenic and other psychotic disorders in the 45 - 64 age group ($3.931 billion). Conclusion: This paper illustrates the high cost of psychiatric care in the U.S., especially the large fraction of healthcare money spent on working-age patients suffering from mood disorders. This underlines psychiatric cost-efficiency as a vital topic in the current healthcare debate.
1. INTRODUCTION
The population of the United States (U.S.) is a vibrant population with constant influx of new immigrants and continuous internal restructuring due to fluctuations in birth and death rates and dynamic ethnic shifts. Latest data shows that life expectancy in the U.S. was 77.9 in 2007 [1], reached 78.2 in 2009 [2] and is projected to be around 80.1 in 2020 [3]. Furthermore, 39.4 million people 60 years and older (July 2008) live in the U.S. [1]. By 2030, the number of U.S. adults aged 65 or older is predicted to reach about 71 million [4].
As a collateral manifestation of these demographic changes, the population’s health profile changes and the resultant utilization of healthcare resources responds to more or less expression of certain diagnostic categories, including psychiatric disorders. In this paper, we analyze national data on the psychiatric morbidity of American patients and their summated cost in different age groups in order to draw attention to the importance of costanalysis in psychiatric research. Determining the most cost-effective interventions for psychiatric disorders represents one key consideration into the broader task of public health decision-making and priority-setting with regard to investing resources in mental health [5-7].
2. METHODS
The latest data (2009) on the number of discharges and amount of expenses linked with psychiatric disorders were extracted from an online query system that grants access to the largest set of publicly available all-payer health care databases—Nationwide Inpatient Sample (NIS) of the Healthcare Cost and Utilization Project (HCUP), the Agency for Healthcare Research and Quality (AHRQ).
We studied the diagnostic and economic psychiatric profile of American patients in relationship to age, which we defined as the spectrum of discharges or national expenses associated with different psychiatric categories across age groups. Psychiatric diagnoses were clustered into a manageable number of clinically meaningful categories according to the Clinical Classifications Software (CCS) developed at the AHRQ.
The HCUPnet presents hospital charges associated with the principal diagnosis (the condition that is the chief reason for the hospital stay, as determined after evaluation during this stay) and uses the term “national bill” for summated hospital charges on a national level. Expenses going to physician consultation services are not provided by that website.
3. RESULTS
National data shows that mood disorders are the largest diagnostic category in terms of the total number of hospital discharges in the 1 - 17 years age group (Figure 1). Since the 18 - 44 age group is the largest age group of the population it has the largest numbers of patients with mood disorders (436,268), psychotic disorders (201,274) and substance-related disorders (137,204). Hospital discharges referable to alcoholrelated disorders are highest in absolute numbers (Figure 2) in the 45 - 64 age group (135,164) then in the 18 - 44 age group (110,897).
Percentagewise, mood disorders constitute the largest psychiatric diagnosis related to hospital discharges in the 1 - 17 years age (Figure 3). The mood disorders proportion decreases gradually as age progresses while delirium, dementia, amnestic and other cognitive disorders increase exponentially after 65 years of age. Moreover, attentiondeficit, conduct, and disruptive behavior disorders and impulse control disorders are specific to the younger age group. On the other hand, schizophrenia and other psychotic disorders as well as alcohol and substance-related disorders peak in the working age groups (18 - 64 years).
From an economic point of view, mood and psychotic disorders in working-age patients take the biggest toll on the healthcare budget (Figure 4). Mood disorders in the 18 - 44 age group has the highest national bill ($5.477 billion) followed by schizophrenic and other psychotic disorders in the same age group ($4.337 billion) and mood disorders in the 45 - 64 age group ($4.310 billion). On the third place come schizophrenic and other psychotic disorders in the 45 - 64 age group ($3.931 billion). Otherwise, alcohol-related disorders in the 45 - 64 age group cost the healthcare budget $2.327 billion and screening for mental disorders and substance abuse in the same age group costs $2.228 billion; though the cost of substance-related disorders is highest in the 18 - 44 age group and amounts to $1.624 billion. Unsurprisingly, delirium, dementia, amnestic and other cognitive disorders
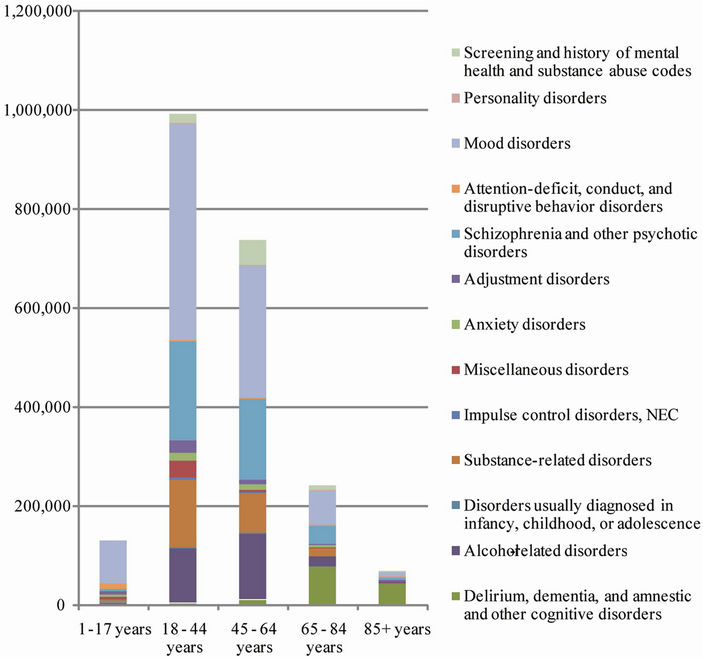
Figure 1. Number of discharges related to psychiatric categories in different age groups.
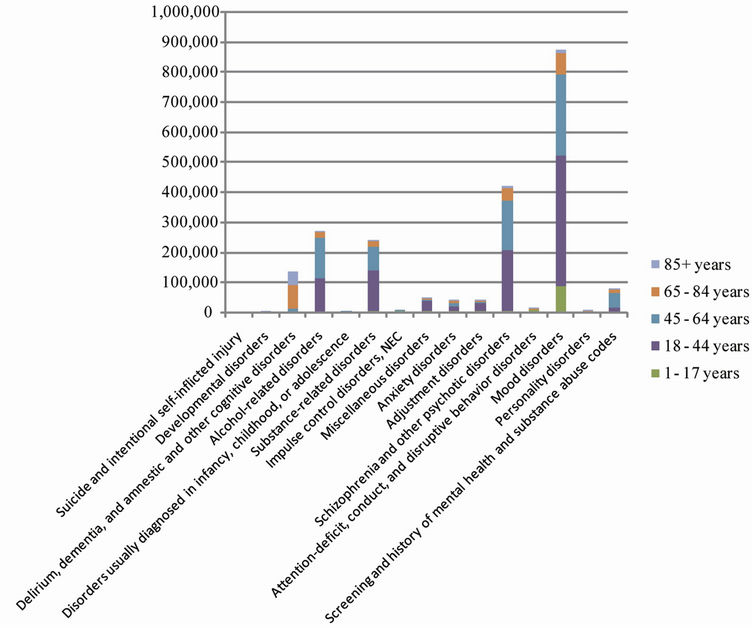
Figure 2. Number of discharges of different age group patients per psychiatric category.
have the highest bill in the 65 - 84 age group totaling $1.725 billion.
Studying the national bill trends of mood disorders and cognitive disorders in certain age groups we find that from 1997 to 2009 the national bill of mood disorders increased 2.4 fold (from 2,236,550,148 to 5,477,797,677) in the 18 - 44 age group and 3.6 fold (1,197,429,873 to 4,310,815,222) in the 45 - 64 age group. On the other hand, in the senior age groups the increase tempo in national bill of cognitive disorders from 1997 to 2009 was nearly similar in the 65 - 84 and 85+ age groups. Thus, the national bill of cognitive disorders in the early-old age group increased 2.2 fold from $753,565,509 in 1997 to $1,725,414,702 in 2009 and in the 85+ age group the increase was 2.7 fold from $315,357,553 in 1997 to $873,628,602 in 2009 (Figure 5).
4. DISCUSSION
Psychiatric illnesses are common and can be costly and debilitating. Mood disorders (depression and bipolar disease) in particular are frequently encountered. In the U.S, approximately 9.1% of the population meets the diagnostic criteria for current depression while 4.1% meet the criteria for major depression [8]. Reflecting that reality, 10% of the population is reported to be on antidepressants—considered the most commonly prescribed medications in the U.S. [9]. Analysis of national data shows that a large fraction of healthcare money ($9.778 billion) is spent on working-age patients suffering from mood disorders (705 thousand). This makes screening protocols for psychiatric morbidities an economic necessity and an investment in the healthcare of the working population.
From their part, screening and history of mental health and substance abuse, despite representing a small percentage of hospital discharges, also consume a signifycant proportion of hospital resources to the benefit of working age and early-old age groups. Screening is a preliminary process of determining whether an individual does or does not warrant further attention at the current time in regard to a particular problem. Screening does not replace an official psychiatric assessment and therefore does not yield a diagnosis. It facilitates the early detection of people at immediate risk and assists in the identification of people with complicated history.
In this context, an Employer’s Guide to Workplace Substance Abuse: Strategies and Treatment Recommendations was developed by the National Business Group on Health (NGBH) to help employers understand substance abuse, the prevalence of this problem among working adults and the costs related to it [10]. The Substance Abuse and Mental Health Services Administration
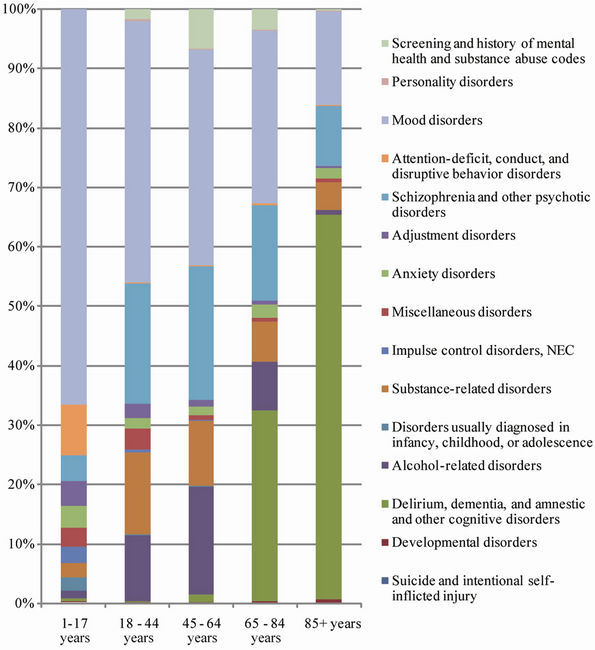
Figure 3. The diagnostic profile of American hospital discharges related to psychiatric morbidity.
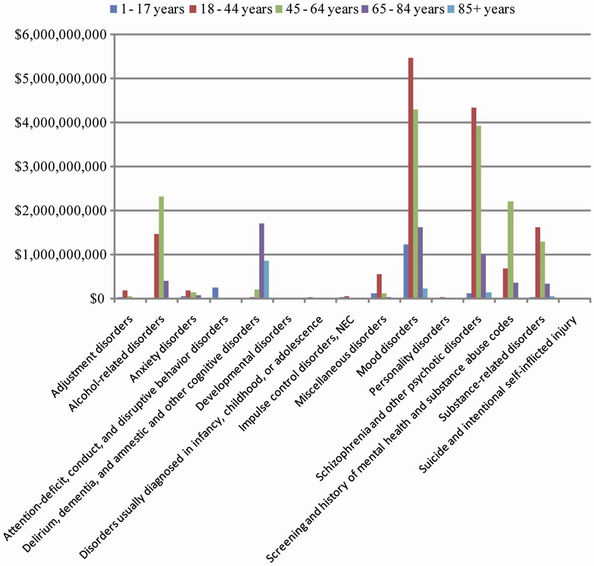
Figure 4. The economic profile of American hospital discharges related to psychiatric morbidity.
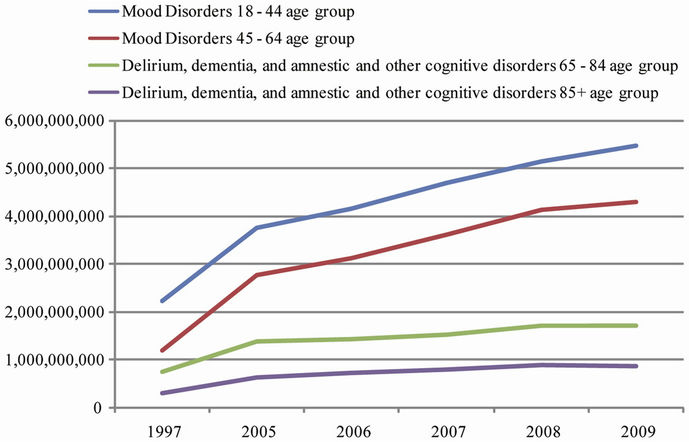
Figure 5. The increase in the national bill of mood and cognitive disorders in the American population.
(SAMHSA) data shows that 20 million adults were classified as having problems with substance dependence or abuse in 2007, approximately 12 million (60%) of them were employed full time [11]. Our study shows that substance-related disorders are a big problem in working age groups (18 - 64 years) with an incredible cost verging on $2.934 billion.
Additionally, it is estimated that more than half of the adult U.S. population drinks alcohol in a moderate or heavy way [12]; yet alcohol-related psychiatric disorders are not the leading psychiatric diagnosis connected with hospital discharges in the U.S. Alcohol abuse has immediate effects that can increase the risk of many harmful health conditions. The summated national hospital expenses attributed to alcohol-related disorders in all age groups in our study total $4.241 billion. In fact, alcohol abuse has far-reaching consequences on the productivity and social life of the individual. A study by the CDC [13] estimated that excessive alcohol consumption actually costs the United States $223.5 billion (2006). The costs largely resulted from losses in workplace productivity (72%), health care expenses (11%), legal and criminal justice expenses (9%), and motor vehicle accidents (6%).
The most dreaded cognitive disorder, Alzheimer’s disease, is at present the sixth leading cause of death in the U.S. [2]. The rate for Alzheimer’s disease increased dramatically due to improvements in diagnosis and awareness of the condition within the medical community. Currently, specialists believe that Alzheimer’s disease has an insidious course beginning long before family and friends notice a dramatic change in the patient’s memory and behavior [14]. By the time an official diagnosis is established, the person’s function is usually significantly impaired and resistant to rehabilitation.
In summary, this paper illustrates the high cost of psychiatric care in the U.S., especially the large fraction of healthcare money spent on working-age patients suffering from mood disorders which makes psychiatric costefficiency a vital topic in the current healthcare debate.
REFERENCES
- Google Public Data Explorer (2012) Population in the U.S. http://www.google.com/publicdata/explore?ds=kf7tgg1uo9ude_&met_y=population&idim=country:US&dl=en&hl=en&q=population+of+the+united+states
- Kochanek, K.D., Xu, J.Q., Murphy, S.L., et al. (2011) Deaths: Preliminary data for 2009. http://www.cdc.gov/nchs/data/nvsr/nvsr59/nvsr59_04.pdf
- Department of Economic and Social Affairs Population Division (2007) World population prospects: The 2006 revision. http://www.un.org/esa/population/ordering.htm
- National Center for Chronic Disease Prevention and Health Promotion (2009) Healthy aging: Improving and extending quality of life among older Americans. http://www.cdc.gov/nccdphp/publications/aag/pdf/healthy_aging.pdf
- Hutubessy, R., Chisholm, D. and Edejer, T.T. (2003) Generalized cost-effectiveness analysis for national-level priority-setting in the health sector. Cost Effectiveness and Resource Allocation, 2003, 1, 8. doi:10.1186/1478-7547-1-8
- Chisholm, D., Sanderson, K., Ayuso-Mateos, J.L. and Saxena, S. (2004) Reducing the global burden of depression: population-level analysis of intervention cost-effectiveness in 14 world regions. The British Journal of Psychiatry, 184, 393-403. doi:10.1192/bjp.184.5.393
- Chisholm, D., van Ommeren, M., Ayuso-Mateos, J.L. and Saxena, S. (2005) Cost-effectiveness of clinical interventions for reducing the global burden of bipolar disorder. The British Journal of Psychiatry, 187, 559-567. doi:10.1192/bjp.187.6.559
- Centers for Disease Control and Prevention (2010) Current depression among adults—United States, 2006 and 2008. Morbidity and Mortality Weekly Report, 59, 1229- 1235.
- Olfson, M. and Marcus, S.C. (2009) National patterns in antidepressant medication treatment. Archives of General Psychiatry, 66, 848-856. doi:10.1001/archgenpsychiatry.2009.81
- Slavit, W.I., Reagin, A. and Finch, R.A. (2009) An employer’s guide to workplace substance abuse: Strategies and treatment recommendations. Center for Prevention and Health Services, Washington DC.
- Department of Health and Human Services (2008) Results from the 2007 national survey on drug use and health: National findings. http://www.samhsa.gov/data/nsduh/2k7nsduh/2k7Results.htm
- Mann, D. (2010) More Americans drinking (alcohol). http://www.cnn.com/2010/HEALTH/07/20/americans.drinking.alcohol.study/index.html
- Bouchery, E.E., Harwood, H.J., Sacks, J.J., Simon, C.J. and Brewer, R.D. (2011) Economic costs of excessive alcohol consumption in the U.S., 2006. American Journal of Preventive Medicine, 41, 516-524. doi:10.1016/j.amepre.2011.06.045
- Galimberti, D. and Scarpini, E. (2011) Progress in Alzheimer’s disease. Journal of Neurology, 259, 201-211. doi:10.1007/s00415-011-6145-3
Appendix: Psychiatric Categories According to the Clinical Classification Software
Adjustment disorders 3090 3091 30922 30923 30924 30928 30929 3093 3094 30982 30983 30989 3099 Anxiety disorders 29384 30000 30001 30002 30009 30010 30020 30021 30022 30023 30029 3003 3005 30089 3009 3080 3081 3082 3083 3084 3089 30981 3130 3131 31321 31322 3133 31382 31383 Attention-deficit, conduct, and disruptive behavior disorders 31200 31201 31202 31203 31210 31211 31212 31213 31220 31221 31222 31223 3124 3128 31281 31282 31289 3129 31381 31400 31401 3141 3142 3148 3149 Delirium, dementia, and amnestic and other cognitive disorders 2900 29010 29011 29012 29013 29020 29021 2903 29040 29041 29042 29043 2908 2909 2930 2931 2940 2941 29410 29411 29420 29421 2948 2949 3100 3102 3108 31081 31089 3109 3310 3311 33111 33119 3312 33182 797 Developmental disorders 3070 3079 31500 31501 31502 31509 3151 3152 31531 31532 31534 31535 31539 3154 3155 3158 3159 317 3180 3181 3182 319 V400 V401 Disorders usually diagnosed in infancy, childhood, or adolescence 29900 29901 29910 29911 29980 29981 29990 29991 30720 30721 30722 30723 3073 3076 3077 30921 31323 31389 3139 Impulse control disorders, NEC 31230 31231 31232 31233 31234 31235 31239 Miscellaneous disorders 29389 2939 30011 30012 30013 30014 30015 30016 30019 3006 3007 30081 30082 3021 3022 3023 3024 30250 30251 30252 30253 3026 30270 30271 30272 30273 30274 30275 30276 30279 30281 30282 30283 30284 30285 30289 3029 3060 3061 3062 3063 3064 30650 30651 30652 30653 30659 3066 3067 3068 3069 3071 30740 30741 30742 30743 30744 30745 30746 30747 30748 30749 30750 30751 30752 30753 30754 30759 30780 30781 30789 3101 316 64840 64841 64842 64843 64844 V402 V403 V4031 V4039 V409 V673 Mood disorders 29383 29600 29601 29602 29603 29604 29605 29606 29610 29611 29612 29613 29614 29615 29616 29620 29621 29622 29623 29624 29625 29626 29630 29631 29632 29633 29634 29635 29636 29640 29641 29642 29643 29644 29645 29646 29650 29651 29652 29653 29654 29655 29656 29660 29661 29662 29663 29664 29665 29666 2967 29680 29681 29682 29689 29690 29699 3004 311 Personality disorders 3010 30110 30111 30112 30113 30120 30121 30122 3013 3014 30150 30151 30159 3016 3017 30181 30182 30183 30184 30189 3019 Schizophrenia and other psychotic disorders 29381 29382 29500 29501 29502 29503 29504 29505 29510 29511 29512 29513 29514 29515 29520 29521 29522 29523 29524 29525 29530 29531 29532 29533 29534 29535 29540 29541 29542 29543 29544 29545 29550 29551 29552 29553 29554 29555 29560 29561 29562 29563 29564 29565 29570 29571 29572 29573 29574 29575 29580 29581 29582 29583 29584 29585 29590 29591 29592 29593 29594 29595 2970 2971 2972 2973 2978 2979 2980 2981 2982 2983 2984 2988 2989 Alcohol-related disorders 2910 2911 2912 2913 2914 2915 2918 29181 29182 29189 2919 30300 30301 30302 30303 30390 30391 30392 30393 30500 30501 30502 30503 76071 9800 Substance-related disorders 2920 29211 29212 2922 29281 29282 29283 29284 29285 29289 2929 30400 30401 30402 30403 30410 30411 30412 30413 30420 30421 30422 30423 30430 30431 30432 30433 30440 30441 30442 30443 30450 30451 30452 30453 30460 30461 30462 30463 30470 30471 30472 30473 30480 30481 30482 30483 30490 30491 30492 30493 30520 30521 30522 30523 30530 30531 30532 30533 30540 30541 30542 30543 30550 30551 30552 30553 30560 30561 30562 30563 30570 30571 30572 30573 30580 30581 30582 30583 30590 30591 30592 30593 64830 64831 64832 64833 64834 65550 65551 65553 76072 76073 76075 7795 96500 96501 96502 96509 V6542 Suicide and intentional self-inflicted injury E9500 E9501 E9502 E9503 E9504 E9505 E9506 E9507 E9508 E9509 E9510 E9511 E9518 E9520 E9521 E9528 E9529 E9530 E9531 E9538 E9539 E954 E9550 E9551 E9552 E9553 E9554 E9555 E9556 E9557 E9559 E956 E9570 E9571 E9572 E9579 E9580 E9581 E9582 E9583 E9584 E9585 E9586 E9587 E9588 E9589 E959 V6284 Screening and history of mental health and substance abuse codes 3051 30510 30511 30512 30513 33392 3575 4255 5353 53530 53531 5710 5711 5712 5713 7903 V110 V111 V112 V113 V114 V118 V119 V154 V1541 V1542 V1549 V1582 V6285 V663 V701 V702 V7101 V7102 V7109 V790 V791 V792 V793 V798 V799
NOTES
*Corresponding author.

