Open Journal of Stomatology
Vol.4 No.7(2014), Article
ID:47911,19
pages
DOI:10.4236/ojst.2014.47045
Face Adaptation in Orthodontics
Maen Mahfouz
Department of Orthodontics and Pediatric Dentistry, Arab American University, Jenin, Palestine
Email: maennmahfouz@gmail.com
Copyright © 2014 by author and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 6 May 2014; revised 20 June 2014; accepted 3 July 2014
ABSTRACT
Bilateral Controversy in orthodontic science is widely present in different patterns; one of the most common is the debate between early versus late orthodontic treatment. This paper is going to demonstrate two clinical cases of class III malocclusion which are treated orthodontically, one in early mixed dentition and the other in permanent dentition. The face is highly capable to adapt to the changes achieved by orthodontics provided the earlier treatment begins, the more the face adapts to our standards; the later treatment begins, the more our standards have to adapt to the face.
Keywords:Face, Adaptation, Orthodontics

1. Introduction
“The earlier treatment begins, the more the face will adapt to your standards; the later treatment begins, the more your standards will have to adapt to the face.”—C. Gugino. (Recent Concepts)—The 20th Century [1] .
i-orthodontic/orthopedic treatment is treatment before the eruption of the full permanent dentition. The idea of treatment of the primary or mixed dentition in a child patient is a totally new concept for many dentists who have learned conventional orthodontic treatment. Even for the dentist who wants to treat child patients, many are at total loss when confronted with whether or not to intervene, when to begin treatment, how to treat various adverse growth patterns, what records are needed and how to form a precise diagnosis for the various findings [2] .
If you are now providing orthodontic treatment, you probably know there are two opposing schools of thought. One philosophy has supported not initiating treatment until the permanent dentition is either complete or close to complete. This school of thought asserts that treatment is easier when most growth has been completed and treatment can avoid needing to compensate for the unexpected variations in growth that may occur earlier. Attempts may be utilized to try to capture the last little bit of growth remaining, by treating the so called “growth spurt” [2] .
The opposing philosophy has been taught and supported by many over the years. What used to be called “early treatment” is now realized to be iOrtho.-Interception orthodontics and orthopedics, and has potential benefits that outweigh traditional “Late” Treatment after growth is concluded. This philosophy has been well established by the bioprogressive group of Ricketts, Gugino, Bench, and Langlade as well as many others including Doyle, Frankel, Graber and McNamara [4] -[12] . These folks propose consideration of the consequences of the many disadvantages to waiting for the permanent dentition, such as: the lack of ability to eliminate or change adverse growth and the functional matrix, and the loss of opportunity to guide not only orofacial development but development of the occlusion [2] .
It is commonly believed that successful camouflage treatment for class III malocclusion can be achieved by proclination of maxillary incisors, retrusion of mandibular incisors, and downward and backward rotation of mandible.
When an increased lower anterior face height is associated with this malocclusion, surgical intervention is the treatment of choice, because any orthodontically induced mandibular clockwise rotation will increase the vertical facial dimensions and, consequently, cause lip incompetence [3] . For patients reluctant to undergo surgery or who are satisfied with their facial appearance, an alternative is to treat with dentoalveolar compensation without correcting the underlying skeletal deformity.
This paper is going to show the difference in face adaptation in orthodontics regarding the timing of orthodontic treatment by demonstrating two clinical cases of class III malocclusion which are treated orthodontically, one in early mixed dentition and the other in permanent dentition. The face is highly capable to adapt to the changes achieved by orthodontics provided the earlier treatment begins, the more the face adapts to our standards; the later treatment begins, the more our standards have to adapt to the face.
2. Case History #1
A 7-year-old boy attended to my private orthodontic clinic with chief compliant of lower anterior teeth overlapping of upper anterior teeth. He was in early mixed dentition stage. In the extraoral, the patient profile was straight while lip profile was reversed giving the appearance of class III (Figures 1-3).
In the intraoral examination revealed a forward shift of the mandible, with a marked class III molar relationship and an anterior crossbite (Figures 4-6).
Diagnosis: The clinical examination revealed retruded upper lip with protruded lower lip giving the view of deficient mid face as seen in class III. The upper incisors retroclined and spaced while lower incisors slightly proclined. An anterior crossbite in the presence of a forward mandibular displacement and functional shift to the left side due to premature contact between upper and lower central incisors, Class III malocclusion with reverse overjet and negative deep overbite. The starting point in diagnosis and treatment of this case was by establishing centric relation through guiding the mandible into centric relation rather than centric occlusion and then initial contact with the teeth occurs so an edge to edge anterior incisor contact with posterior open bite indicating Pseudo Class III (Figures 1-7).

Figure 1. Frontal-extraoral view.

Figure 2. Smile view.
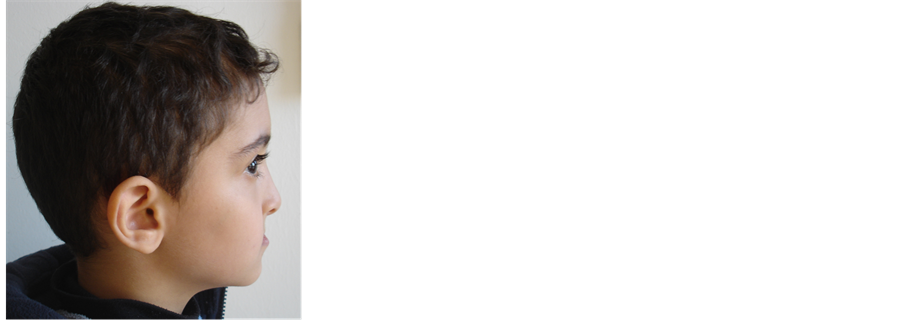
Figure 3. Profile view.
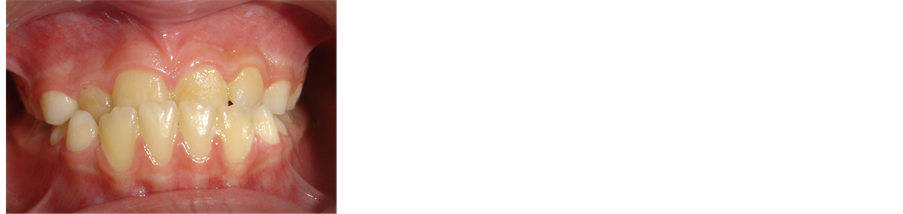
Figure 4. Frontal-intraoral view.
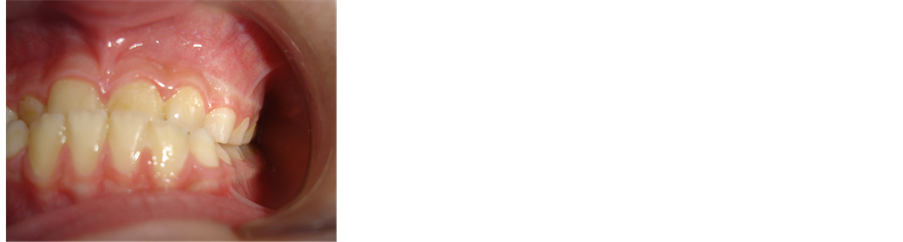
Figure 5. Left side—intraoral view.

Figure 6. Right side—intraoral view.

Figure 7. Initial contact between teeth in centric relation.
Cephalometric analysis indicated a mild Class III malocclusion characterized by a little mandibular protrusion, maxillary retroclined incisors (ANB = −1 degree, Wits= −6 mm, I-SN = 100 degree) (Figure 8, Figure 9 and Table 1).
Treatment Objectives: forward movement of 11 maxillary incisors, eliminating functional shift, mandibular displacement, premature contact, enhancing normal lip profile, achieving class I molar relationship and canine relationship with ideal overjet and overbite.
Treatment plan: fixed orthodontic treatment by using protrusive arch wire for the forward movement of 11 without raising the bite.
Treatment procedure: Treatment started so a bondable tubes placed on the buccal surfaces of upper first permanent molars on both sides with brackets (slot 22) placed on the labial surface of the upper central incisors. Then placement of upper Niti arch wire rectangular (0.016 × 0.022) (Protrusive Arch Wire) was customized to the arch form of the patient A gable bend was made mesial to the bondable tubes on first permanent molars. The exposed part of arch wire coated with sleeve to prevent irritation to cheek (Figure 10, Figure 11).
After two weeks orthodontic evaluation has been done of the retroclined upper central incisors which were orthodontically adjusted so the patient could bite in the new situation. The total treatment time was two weeks and the appliance was removed on the end of the second week (Figure 12, Figure 13).
A 2 years’ follow up for this case with good stability of occlusion, optimal functional and aesthetical states. Final superimpositions showed improvements in ANB and Wits values (+1 degree, −1 mm) respectively. The slight maxillary incisor protrusion coupled with the clockwise mandibular rotation produced an overall improvement of the patient’s aesthetic appearance (Figures 14-19).
3. Case History #2
A 14-year-old boy attended to my private orthodontic clinic with chief compliant of reverse anterior overbite and an unaesthetic smile. He was in permanent dentition stage. In the extraoral, the patient profile was straight, while lip profile was reversed giving the appearance of class III (Figures 20-22).
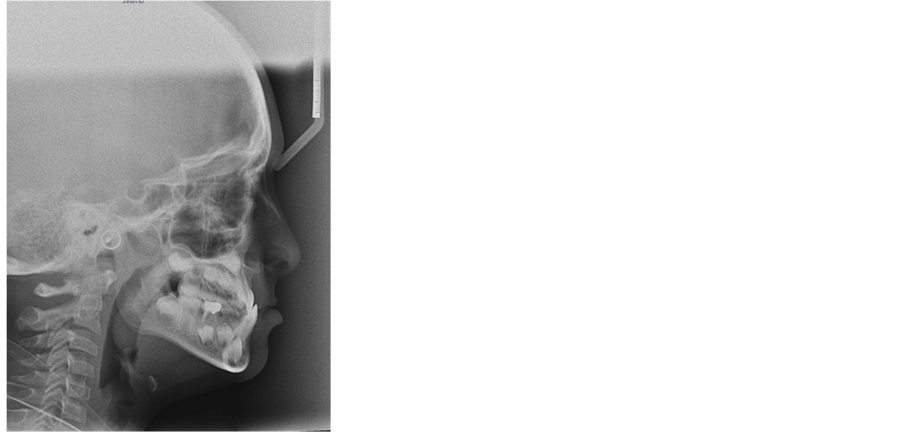
Figure 8. Lateral cephalometric radiograph.

Figure 9. Cephalometric analysis—pretreatment.
Table 1. Cephalometric measurements of the patient case #1.
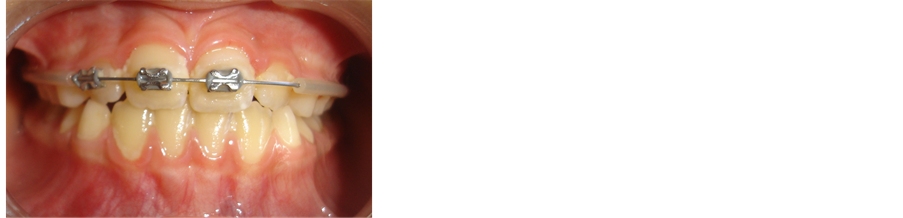
Figure 10. Intraoral view of protrusive arch wire.
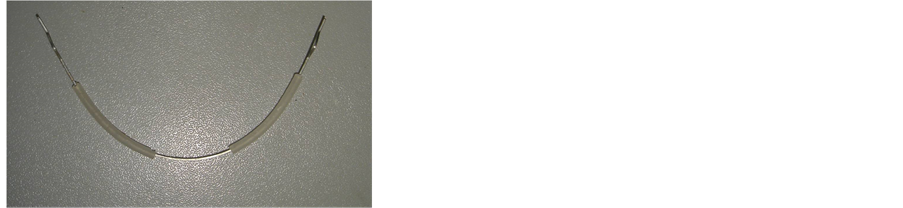
Figure 11. Protrusive arch wire.

Figure 12. Intraoral view—post-treatment.

Figure 13. Intraoral view—post-treatment.
In the intraoral examination revealed marked Angle’s Class III molar relationship with anterior and posterior crossbite, reverse overjet, no overbite and upper dental midline shift to left side 4 mm (Figures 23-25).
Diagnosis:
The clinical examination revealed asymmetrical tapered constricted upper dental arch, moderate crowding, upper anterior teeth in an edge to edge with lower anterior teeth and upper left 2, left 5 and right 5 in crossbite. while, lower arch is symmetrical ovoid dental arch, with mild crowding. Upper dental midline shift to left side 4 mm, the upper incisors proclined while lower incisors slightly proclined. An anterior crossbite in the presence of a posterior crossbite bilaterally, Class III malocclusion with reverse overjet and negative overbite (Figures 23-25).

Figure 14. Lateral profile view—posttreatment after two weeks.

Figure 15. Lateral-profile view—posttreatment after 2 years.

Figure 16. Frontal-extraoral view after 2 years.

Figure 17. Frontal-intraoral view after 2 years.
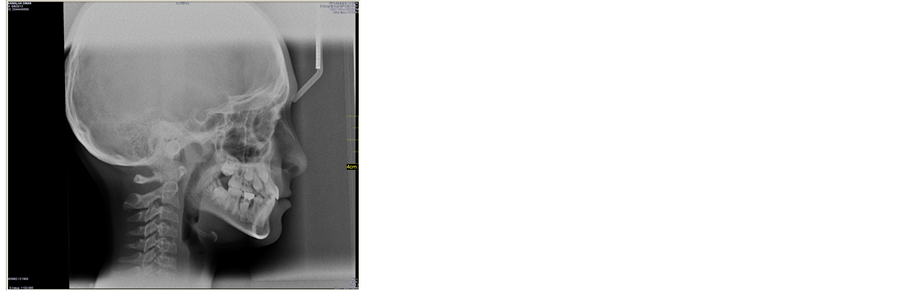
Figure 18. Post-treatment lateral cephalometric radiographs.
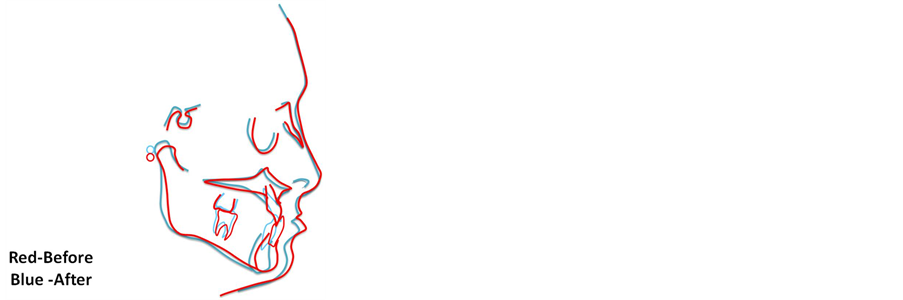
Figure 19. Cephalometric superimposition.
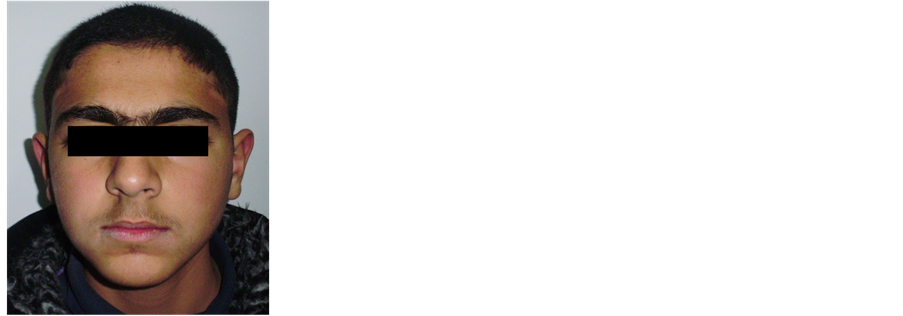
Figure 20. Frontal-extraoral view.

Figure 21. Smile view.

Figure 22. Profile view.

Figure 23. Frontal—intraoral view.

Figure 24. Left side—intraoral view.
Cephalometric analysis indicated a mild Class III malocclusion characterized by a little Maxillary retrusion (ANB = 0 degree after Eastman’s correction, Wits = −8 mm) (Figure 26 and Figure 27).
Treatment Objectives:
1) To establish Class I canine relationships;

Figure 25. Right side—intraoral view.
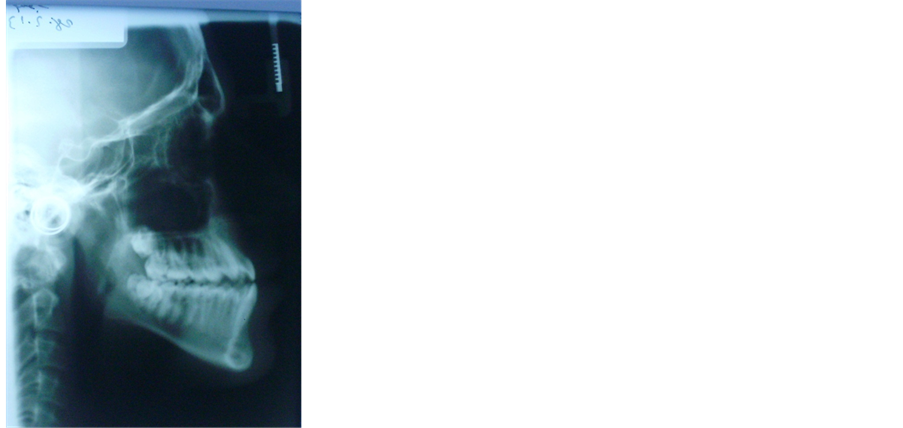
Figure 26. Lateral cephalometric radiograph.
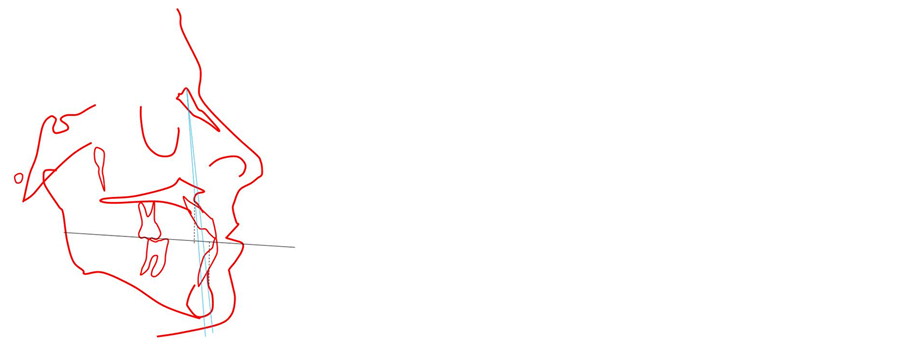
Figure 27. Cephalometric analysis— pretreatment.
2) To achieve good intercuspation between upper and lower teeth;
3) To align arches;
4) To correct overbite, overjet and midlines;
5) To provide an aesthetic smile.
Treatment plan: To meet most of these treatment objectives we decided on a nonsurgical treatment protocol fixed orthodontic treatment.
Treatment procedure:
Maxillary and mandibular fixed appliances (standard edgewise 0.022-inch) were used. After initial leveling and alignment with round wires in both arches, a 0.016 × 0.022 inch Niti arch wire was used for protrusion of the upper incisors. For settling of occlusion box elastics were used. Fixed appliance treatment was completed in 15 months (Figures 28-33).
The treatment plan was a satisfactory non-surgical alternative, and the treatment objectives were achieved (Figures 34-40 and Table 2). A Class I canine relationship was established with good alignment. Some occlusal adjustment was needed to finalize the occlusion. A positive overjet was established and the overbite was somewhat reduced. Tooth position was controlled while the mandibular incisors were retracted resulting in improved incisor inclination after treatment. The maxillary incisors were proclined significantly resulting in better upper
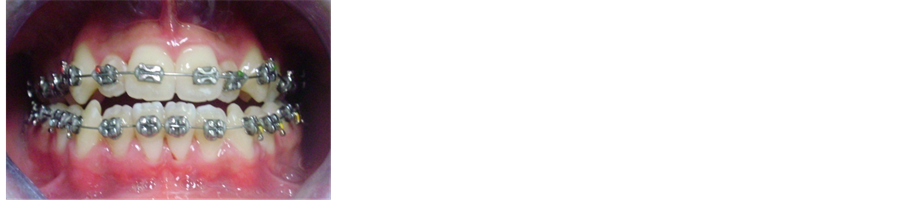
Figure 28. Intraoral view—at the beginning of treatment.
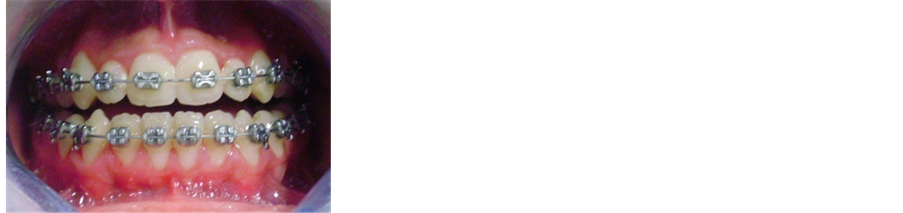
Figure 29. Intraoral view—during treatment.

Figure 30. Intraoral view—during treatment.
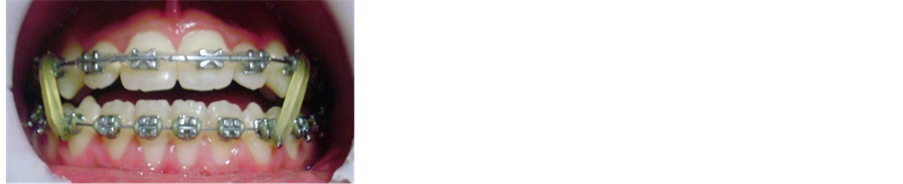
Figure 31. Intraoral view—during treatment.

Figure 32. Intraoral view—during treatment.

Figure 33. Intraoral view—during treatment.
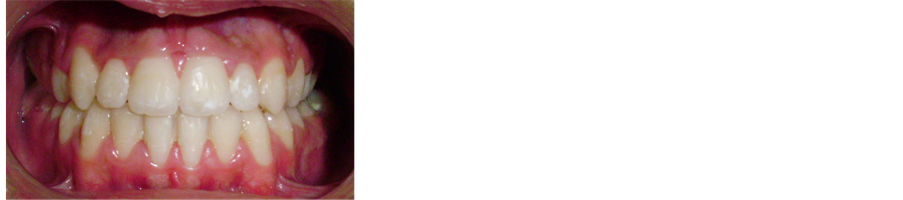
Figure 34. Intraoral view—post-treatment after 15 months.

Figure 35. Right side—intraoral view-posttreatment.
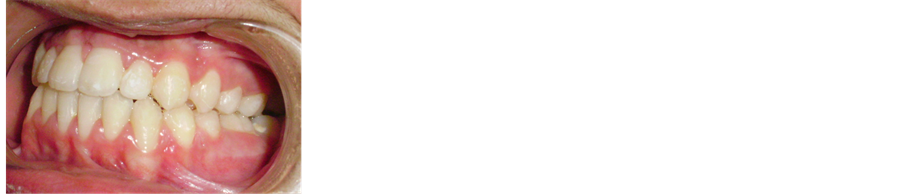
Figure 36. Left side—intraoral view— post-treatment.

Figure 37. Smile view—post-treatment after 15 months.
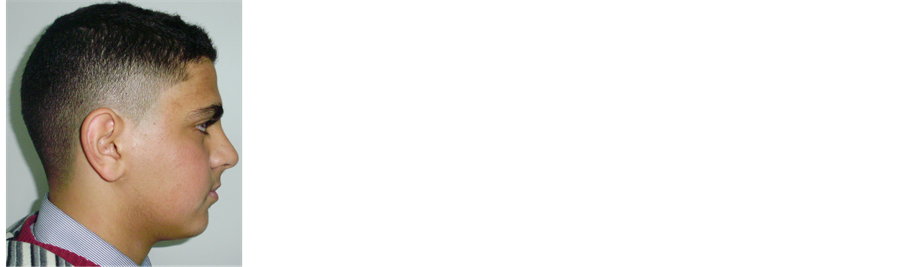
Figure 38. Lateral profile view—posttreatment after 15 months.
lip prominence and an improved facial profile. Correction of the malocclusion was accomplished with dentoalveolar changes only.
Final superimpositions showed improvements in ANB and Wits values (+2 degree, −1 mm) respectively. The slight maxillary incisor protrusion coupled with the clockwise mandibular rotation produced an overall improvement of the patient’s aesthetic appearance (Figures 34-41 and Table 2).
4. Discussion
We know that modern medical thought is, that it is better to prevent than to cure. Certainly dentistry has its hallmark, prevention of disease. Yet for generations dentistry has viewed orthodontic treatment differently. Conventionally, Orthodontics has been provided in the permanent dentition. Orthodontic treatment should be in harmony with modern medicine and dentistry. We should not treat the signs and symptoms—we should treat the causes; we should prevent [2] .
Table 2. Cephalometric measurements of the patient case #2.

Figure 39. Post-treatment lateral cephalometric radiographs after 15 months.

Figure 40. Cephalometric analysis— post treatment.
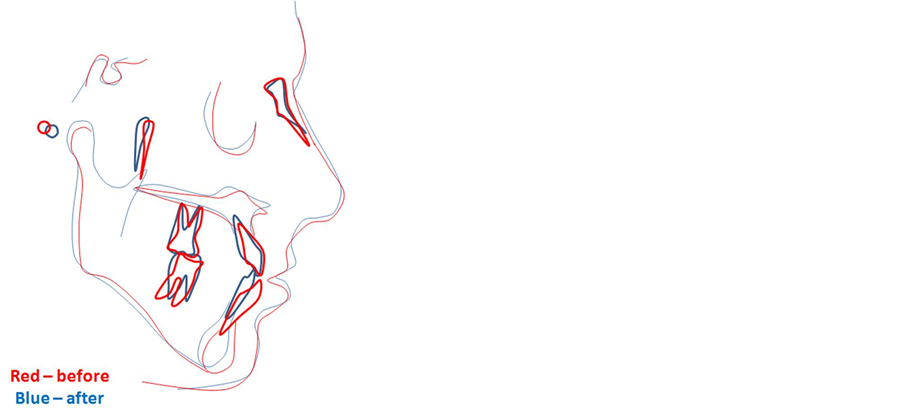
Figure 41. Cephalometric superimposition.
Over 50 years ago Melvin Moss introduced the functional matrix theory which said simply “form follows function”. Studies have tested his theory, and we now know that indeed, the environment (function) is an important factor in the resultant growth and development of the child.
We know that with habits tongue position and mouth breathing, adverse growth occurs, often excess vertical growth, though not always and malocclusion and less than pleasing esthetics are borne [13] .
We know neuronal function underlies abnormal development of the cranial synchondroses and midface retrusion follows [14] [15] . The functional matrix is at the heart of malocclusion and of lessened esthetics. We should be at the front of prevention.
We know that 20% - 35% of adult patients have signs and symptoms of occlusal dysfunction [16] many of them having had orthodontic treatment in permanent dentition. We know that the younger the child the faster and more the growth.
In order to determine whether it is appropriate in a given patient to provide orthodontic treatment in the primary or mixed dentition and or permanent dentition one must have understanding of craniofacial growth and development (morphogenesis), and of craniofacial pathogenesis(adverse development/malocclusion). So the clinical implication of the earlier orthodontic treatment is more pronounced as in the case #1 is reflected at the level of the face as lip profile after treatment and has greater skeletal and dental effects as showing in Table 1 in comparison to the later orthodontic treatment as in the case #2 which has longer duration of treatment and has greater dental effect than skeletal effect as showing in Table2
In the presented case #1, as the upper central incisors are retroclined, so there is premature contact which avoided by forward mandibular displacement associated with functional shift to the left to achieve more comfortable bite in centric occlusion(functional adaptation). In contrast there is an edge to edge relationship between upper and lower teeth with posterior open bite which is not comfortable in centric relation.
In the presented case #1, the method used to eliminate the premature contact was not occlusal adjustment by selective grinding which involves the selective reshaping of tooth surfaces that interfere with normal jaw function, it was an orthodontic occlusal adjustment by correction of the position of the retroclined upper central incisors to procline them forward by using the protrusive arch wire [1] [17] [18] .
In the presented case #2, the orthodontic treatment of an adult patient with a skeletal Class III malocclusion, increased anterior facial height, negative overjet, and bilateral posterior crossbite is presented. A non-surgical treatment alternative has produced results comparable with those that could be achieved surgically, then it should be considered and can be the treatment of choice for some patients while the surgical correction of Class III malocclusion can be undertaken in a variety of ways, e.g. a bilateral sagittal split osteotomy to retract the mandible or a Le Fort I procedure to advance the maxilla, or a combination of these. However, the associated surgical risks and complications must be considered, as well as the increased expense [1] [19] [20] .
The changes contributing most to the correction were maxillary incisor proclination, and the extrusion and bodily retrusion of the mandibular incisors with concurrent alveolar remodeling. These changes produced a counterclockwise rotation of the occlusal plane as expected [21] . Obviously, a surgical approach would have produced even better occlusal and esthetic results [22] [23] .
The clinical significance of this topic the earlier treatment begins the rapid correction occurs and the more the face adapts to our standards especially improving the esthetic and functional requirements for development and growth which is still working as in case #1 while the later treatment begins the longer duration required and the more our standards have to adapt to the face especially for patient reluctant to undergo surgery as in case #2.
5. Conclusions
1) Orthodontic treatment should be in harmony with modern medicine and dentistry. We should not treat the signs and symptoms—we should treat the causes; we should prevent.
2) The earlier treatment begins, the more the face will adapt to your standards; the later treatment begins, the more your standards will have to adapt to the face.
Acknowledgements
First and foremost I would like to thank my family: Dad “Mohammad Naeem Mahfouz “Mom “Wedad Jarrad” Brother Allam Mahfouz, Sisters, Hanin Mahfouz, Suha Mahfouz, Bayan Mahfouz, Wife Yara Mansour and my kids, Omar Mahfouz, Noor Mahfouz and Sara Mahfouz for their valuable great support, guidance and advice.
References
- Mahfouz, M. (2014) The Current Concepts of Orthodontic Discrepancy Stability. Open Journal of Stomatology, 4, 184-196. http://dx.doi.org/10.4236/ojst.2014.44028
- Chris Baker, R.N. (2012) I Ortho: Should I Provide Interception Orthodontic Treatment? Journal of the American Orthodontic Society, July-August Issue, 78-79.
- Bilodeau, J. (1995) Vertical Considerations in Diagnosis and Treatment: A Surgical Orthodontic Case Report. American Journal of Orthodontics and Dentofacial Orthopedics, 107, 91-100. http://dx.doi.org/10.1016/S0889-5406(95)70160-5
- Ricketts, R.M. (1976) Bioprogressive Therapy as an Answer to Orthodontic Needs. Part I. American Journal of Orthodontics, 70, 241-268. http://dx.doi.org/10.1016/0002-9416(76)90332-8
- Ricketts, R.M. (1976) Bioprogressive Therapy as an Answer to Orthodontic Needs. Part II. American Journal of Orthodontics, 70, 359-397. http://dx.doi.org/10.1016/0002-9416(76)90111-1
- Ricketts, R.M. (1960) The Influence of Orthodontic Treatment on Facial Growth and Development. Angle Orthodontist, 30, 103-133.
- Ricketts, R.M., Bench, R.W., Gugino, C.F., Hilgers, J.J. and Schulhof, R.J. (1979) Bioprogressive Therapy. Rocky Mountain Orthodontics, Denver.
- Langlade, M. (1973) Therapeutique Orthodontique. Maloine, Paris.
- Fränkel, R. (1969) The Treatment of Class II, Division 1 Malocclusion with Functional Correctors. American Journal of Orthodontics, 55, 265-275.
- Graber, T.M. (1972) Orthodontics: Principles and Practice. W.B. Saunders, Philadelphia.
- Graber, T.M. and Vanarsdal, R.L. (1994) Orthodontics Current Principles and Techniques. 2nd Edition, Mosby, St. Louis.
- McNamara Jr., J.A. (1986) Utility Arches. Journal of Clinical Orthodontics, 20, 452-456.
- Linder-Araonson, S. and Woodside, D.G. (1979) The Growth in the Sagittal Depth of the Bony Nasophayrnx in Relation to Some Other Facial Variables. In: McNamara, J.A., Ed., Naso-Respiratory Function and Craniofacial Growth, Monograph No.9 Craniofacial Growth Series, Center of Human Growth and Development, The University of Michigan, Ann Arbor.
- Gerstenfeld, L.C. and Shapira, F.D. (1996) Expression of Bone Specific Genes by Hypertrophic Chondrocytes: Implication of the Complex Functions of the Hypertrophic Chondrocyte during Endochondral Bone Development. Journal of Cellular Biochemistry, 62, 1-9. http://dx.doi.org/10.1002/(SICI)1097-4644(199607)62:1<1::AID-JCB1>3.0.CO;2-X
- Kyrkanides, S., Moore, T., Miller, J.H. and Tallents, R.H. (2011) Melvin Moss’ Functional Matrix Theory—Revisited. Orthodontic Waves, Official Journal of the Japanese Orthodontic Society, 70, 1-7.
- EACD: European Academy of Craniomandibular Disorders. http://www.eacmd.org/patient.php
- Mahfouz, M. (2014) Pseudo Class III Treatment in 2-Year-Old Children. Open Journal of Stomatology, 4, 10-13. http://dx.doi.org/10.4236/ojst.2014.41003
- Mahfouz, M. (2014) Pseudo Class III Correction in Early Mixed Dentition by Using Protrusive Arch Wire. Journal of Orthodontic Research, Sep-Dec Issue, in press.
- Popp, T.W., Gooris, C.G.M. and Schur, A.J. (1993) Nonsurgical Treatment for a Class III Dental Relationship: A Case Report. American Journal of Orthodontics and Dentofacial Orthopedics, 103, 203-211.
- Gelgör, I.E. and Karaman, A.I. (2005) Non-Surgical Treatment of Class III Malocclusion in Adults: Two Case Reports. Journal of Orthodontics, 32, 89-97. http://dx.doi.org/10.1179/146531205225020952
- Lin, J. and Gu, Y. (2003) Preliminary Investigation of Nonsurgical Treatment of Severe Skeletal Class III Malocclusion in the Permanent Dentition. The Angle Orthodontist, 73, 401-410.
- Bilodeau, J. (1996) Correction of a Severe Class III Malocclusion That Required Orthognathic Surgery: A Case Report. Seminars in Orthodontics, 2, 279-288. http://dx.doi.org/10.1016/S1073-8746(96)80028-4
- Dwyer, P. (1998) Orthodontic and Orthognathic Surgical Correction of A Severe Class III Malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics, 113, 125-132. http://dx.doi.org/10.1016/S0889-5406(98)70284-7


