Open Journal of Pediatrics
Vol. 2 No. 4 (2012) , Article ID: 25225 , 3 pages DOI:10.4236/ojped.2012.24042
Re-expansion pulmonary edema in a boy with spontaneous pneumothorax during an influenza B virus infection*
![]()
Department of Pediatrics, Niigata City General Hospital, Niigata, Japan
Email: twata@hosp.niigata.niigata.jp
Received 27 July 2012; revised 23 August 2012; accepted 6 September 2012
Keywords: Reexpansion Pulmonary Edema; Influenza Virus; Pulmonary Complication
ABSTRACT
Re-expansion Pulmonary Edema (RPE) is an uncommon complication following rapid re-expansion of the lungs, and the most common disorder associated with RPE is spontaneous pneumothorax. The majority of patients with RPE associated with pneumothorax have been adults; only 4 cases have been reported in children. We present a patient who developed RPE after treatment of spontaneous pneumothorax that occurred during an influenza B virus infection. His condition improved only with oxygen supplementation and intravenous corticosteroids. Infection with influenza B virus leads to increased production of lung epithelial oxidants, which might have contributed to the development of RPE in our patient.
1. INTRODUCTION
Re-expansion Pulmonary Edema (RPE) is an uncommon complication that occurs when a collapsed lung is rapidly re-expanded after evacuation of air or fluid from the pleural space [1]. Although it is possible for RPE to occur in every type of chronically collapsed lung that can be re-expanded, the most common disorder associated with RPE is spontaneous pneumothorax [2]. The majority of patients with RPE associated with pneumothorax have been adults [1]; only 4 cases have been reported in children [3-5]. We report a patient who developed RPE after treatment of spontaneous pneumothorax that occurred during an influenza B virus infection.
2. PATIENT REPORT
A previously healthy, 6-year-old boy was admitted to our hospital after 2 days of cough, dyspnea and high-grade fever. On admission, the patient was febrile with a body temperature of 39.6˚C, and his oxygen saturation was 94% while breathing ambient air.
Physical examination showed tachypnea and diminished breath sounds over the left hemi-thorax. A nasopharyngeal swab tested positive for influenza B on a rapid influenza antigen detection test. Routine laboratory tests were normal except for a slightly elevated C-reactive protein concentration. Chest radiography revealed a left-sided pneumothorax (Figure 1(a)). His symptoms improved immediately after placement of a chest tube with application of a negative pressure of 10 cm H2O. However, after 30 minutes, the patient again exhibited tachypnea and his oxygen saturation decreased to 88%. Chest auscultation revealed left-sided inspiratory crackles. Repeat chest radiography showed a fully expanded left lung, but also left-sided pulmonary edema (Figure 1(b)).
The patient was diagnosed with RPE occurring after treatment of pneumothorax. He was administered oxygen supplementation (5 L/min via face mask) and intravenous corticosteroids. His condition gradually improved over the next 2 days, and after an additional 3 days, his pneumothorax and RPE completely resolved. The patient was discharged after the chest tube was removed, without further sequelae. The patient remained well over a 6 months follow-up period.
3. DISCUSSION
RPE has been reported after rapid evacuation of large pneumothorax or large pleural effusion [4]. The clinical features of RPE include the following: a collapsed lung over period of 3 days or more; an evacuation volume of 2000 ml or more; a period of less than 1 hour from re-expansion to the onset of RPE; and the pulmonary edema is classified as permeability pulmonary edema [2]. Risk factors for RPE include the degree of lung collapse and a rapid re-expansion [1]. The symptoms of RPE range from asymptomatic presentation to cardiopulmonary insufficiency [4] and the reported mortality rate has ranged from 0% to 20% [1].
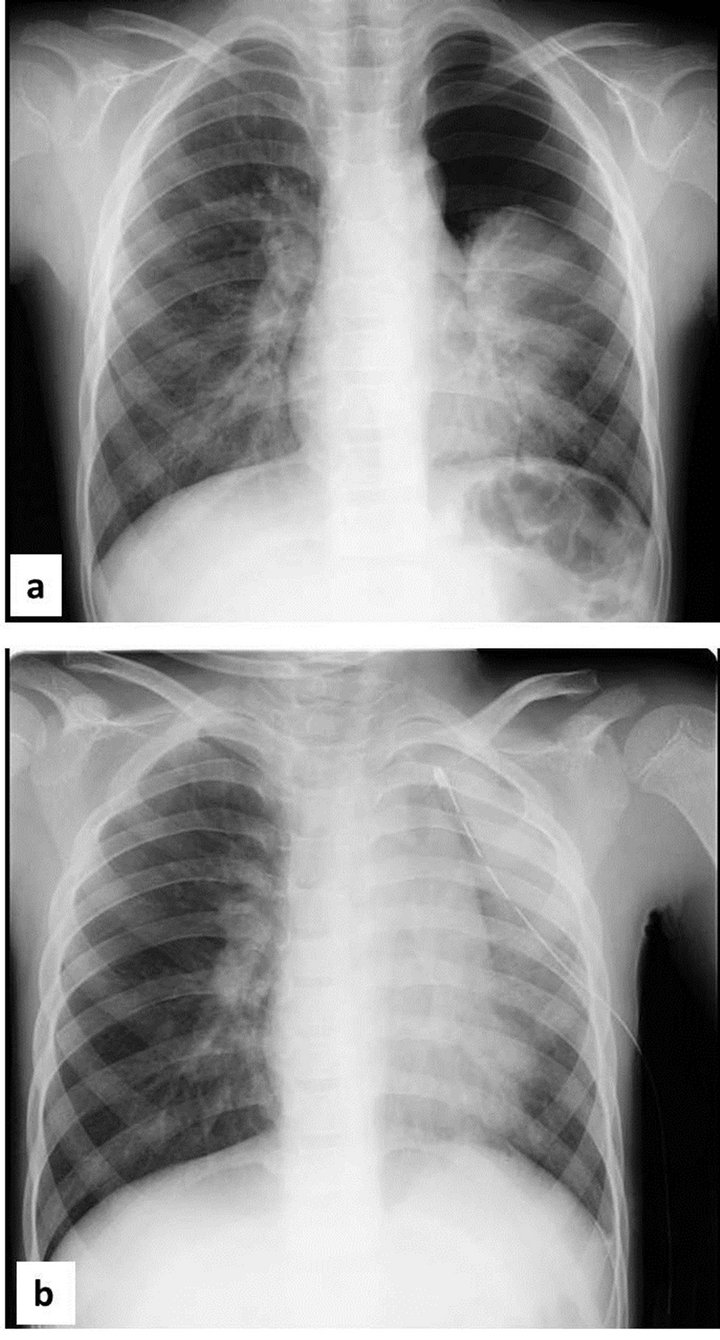
Figure 1. (a) Chest radiograph on admission showing spontaneous pneumothorax of the left lung; (b) Chest radiograph after insertion of the chest tube showing reexpansion pulmonary edema of the left lung.
Despite the fact that the rate of occurrence of RPE after drainage of a pneumothorax varies from 14.4% to 27%, there have only been 4 reports from the pediatric population [3-5]. Pediatric cases of RPE with diseases other than pneumothorax are also rare; RPE has been reported in children with pleural effusion due to nephrotic syndrome [6] or non-Hodgkin’s lymphoma [7,8], with reinflation of a retracted lung following patent ductus arterious ligation [9] or following general anesthesia [10], and with pleural empyema [11].
Treatment for RPE remains supportive, using oxygenation, positive-pressure mechanical ventilation and utilization of positive end-respiratory pressure, diuresis and hemodynamic support. In addition, the use of prostaglandin analogs or corticosteroids has been also reported [1,2,12]. However, the best treatment is to avoid rapid lung re-expansion [2].
Although the precise pathogenic mechanism for the development of RPE remains unclear, the common endpoint in the pathological process is probably enhanced endothelial permeability caused by a combination of alveolar-capillary membrane disruption and ischemia-reperfusion-mediated injury [1,2]. Oxygen radicals and interleukin 8 (IL-8) have also been reported to be contributing factors in the development of RPE [1,2].
In our patient, RPE occurred following treatment of pneumothorax associated with influenza B virus infection. Infection with influenza virus leads to increased production of lung epithelial oxidants, which directly and/or via IL-8 expression results in injury to the lung epithelial cells [13]. Influenza virus induction of these mediators might have contributed to the development of RPE in our patient.
REFERENCES
- Neustein, S.M. (2007) Reexpansion pulmonary edema. Journal of Cardiothoracic and Vascular Anesthesia, 21, 887-891. doi:10.1053/j.jvca.2007.01.014
- Sohara, Y. (2008) Reexpansion pulmonary edema. Annals of Thoracic and Cardiovascular Surgery, 4, 205-209.
- Henderson, A.F., Banham, S.W. and Moran, F. (1985) Reexpansion pulmonary edema: A potentially serious complication of delayed diagnosis of pneumothorax. British Medical Journal, 291, 593-594. doi:10.1136/bmj.291.6495.593
- Lai, S.H., Wong, K.S., Liao, S.L. and Hsia, S.H. (2002) Re-expansion pulmonary edema in an adolescent girl. Pediatric Emergency Care, 18, 297-299. doi:10.1097/00006565-200208000-00015
- Taha, S., Bartelmaos, T., Kassas, C., Khatib, M. and Baraka, A. (2002) Complicated negative pressure pulmonary oedema in a child with cerebral palsy. Paediatr Anaesth, 12, 181-186. doi:10.1046/j.1460-9592.2002.00814.x
- Jardine, D.S. (1991) Reexpansion pulmonary edema. American Journal of Diseases of Children, 145, 1092-1093. doi:10.1001/archpedi.1991.02160100024016
- Özlü, O., Kiliç, A. and Cengizlier, R. (2000) Bilateral reexpansion pulmonary edema in a child: A reminder. Acta Anaesthesiologica Scandinavica, 44, 884-885. doi:10.1034/j.1399-6576.2000.440717.x
- Pietsch, J.B., Whitlock, J.A., Ford, C. and Kinney, M.C. (1999) Management of pleural effusions in children with malignant lymphoma. Journal of Pediatric Surgery, 34, 635-638. doi:10.1016/S0022-3468(99)90093-3
- Chiang, M.C., Lin, W.S., Lien, R. and Chou, Y.H. (2004) Reexpansion pulmonary edema following patent ductus arteriosus ligation in a preterm infant. Journal of Perinatal Medicine, 32, 365-367. doi:10.1515/JPM.2004.068
- Kira, S., Tozawa, K., Sato, M., Fukunaga, T. and Suzuki, M. (2012) Suspected reexpansion pulmonary edema during emergence from general anesthesia in a child with developmental dysplasia of the hip. Paediatr Anaesth, 22, 591-592. doi:10.1111/j.1460-9592.2012.03859.x
- Paksu, M.S., Paksu, S., Akgün, M., Kalayci, A.G. and Baysal, K. (2011) Bilateral re-expansion pulmonary edema associated with pleural empyema: A case report. European Journal of Pediatrics, 170, 1205-1207. doi:10.1007/s00431-011-1441-6
- Trachiotis, G.D., Vricella, L.A., Aaron, B.L. and Hix, W.R. (1997) As originally published in 1988: Reexpansion pulmonary edema. Update in 1997. The Annals of Thoracic Surgery, 63, 1206-1207. doi:10.1016/S0003-4975(97)00193-8
- Knobil, K., Choi, A.M., Weigand, G.W. and Jacoby, D.B. (1998) Role of oxidants in influenza virus-induced gene expression. American Journal of Physiology, 274, L134- L142.
NOTES
*Conflict of interest: There is no conflict of interest with regard to this manuscript.

