American Journal of Operations Research
Vol.04 No.04(2014), Article ID:47675,7 pages
10.4236/ajor.2014.44018
Elimination of Post-Operative Complications in Penetrating Keratoplasty by Deploying Six Sigma
İbrahim Şahbaz1, Mehmet Tolga Taner2*, Üzeyir Tolga Şahandar3, Gamze Kağan4, Engin Erbaş5
1Department of Opticianry, Uskudar University, Istanbul, Turkey
2Department of Healthcare Management, Uskudar University, Istanbul, Turkey
3Isparta State Hospital, Isparta, Turkey
4Department of Occupational Health and Safety, Uskudar University, Istanbul, Turkey
5Institute of Health Sciences, Uskudar University, Istanbul, Turkey
Email: *mehmettolga.taner@uskudar.edu.tr
Copyright © 2014 by authors and Scientific Research Publishing Inc.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/



Received 23 May 2014; revised 25 June 2014; accepted 2 July 2014
ABSTRACT
This paper shows how a public eye and research hospital in Turkey initiated Six Sigma principles to reduce the number of complications occurring after penetrating keratoplasty surgeries. Data were collected for nine years. To analyse the complications among 55 patients (59 eyes) under- went penetrative keratoplasty, main tools of Six Sigma’s Define-Measure-Analyze-Improve-Control (DMAIC) improvement cycle such as SIPOC table and Failure, Mode and Effect Analysis (FMEA) were implemented. Sources and root causes of eleven types of complications were identified and reported. For a successful penetrating keratoplasty surgery patient’s anatomy, suitability of donor cornea, experience of ophthalmic surgeon, sterilization and hygiene, and performance of the equipment were determined to be the “critical-to-quality” factors. The complication with the highest hazard score was found to be the glaucoma. The process sigma level of the process was measured to be 3.1418. The surgical team concluded that all types of post-operative complications should be significantly reduced by taking the necessary preventive measures.
Keywords:
Six Sigma, Ophthalmology, Penetrating Keratoplasty Surgery, Post-Operative Complications

1. Introduction
Corneal eye disease is the fourth most common cause of blindness after cataracts, glaucoma and age-related ma- cular degeneration, affecting more than 10,000,000 people worldwide. Since the first successful human corneal transplant performance in 1905, the cornea transplants have become the most successful and the most common solid tissue transplant with 600,000 procedures performed in the United States over the past 40 years and [1] [2] . In 2013, more than 47,361 corneal transplants were performed in the United States resulting in nearly $6 billion in total net benefits over the lifetime of the recipients [3] .
Penetrating Keratoplasty (PKP) is a standard full thickness transplant that involves the surgical removal of the central two-thirds of the damaged cornea. With changes in medical and surgical management, one expects a de- crease in the number of complications after PKP surgery. Although the surgical procedure restores vision and also relieves pain and suffering caused by injured and diseased cornea with high success rate, studies continue to show many post-operative complications such as wound leaks, malpositioning of the donor cornea, suture ex- posure and infections, infiltration of immune due to suture, persistent epithelial defect, filamentary keratitis, pri- mary endothelial insufficiency, glaucoma, cataract, acute choroidal detachment, epithelial down growth, fix di- lated pupils, refractive changes, graft infections, recurrent disease, shallow anterior chamber, graft rejection, hypotony, cystoid macular edema, endophtalmitis and sympathetic ophthalmia [1] [4] - [11] . In addition, residual astigmatism after PKP surgery may limit postoperative visual function and be the cause of decreased patient sa- tisfaction in the presence of a clear graft [12] . When these complications occur, proper and prompt management is essential. Preventative measures will result in earlier visual rehabilitation and greater long-term graft survival.
PKP surgery shows an overall positive prognosis in the long term [13] . Therefore, ophthalmic surgeons are in a critical position and must be aware of all types of complications that may occur, how to avoid them and how to manage them to ensure the best possible outcomes.
The use of Six Sigma, as a quality improvement method, can improve the surgical safety, efficiency and ac- curacy of many ophthalmic surgeries [14] . In this study, the development a Six Sigma infrastructure in a Turkish public eye and research hospital to improve the PKP surgery process will be shown. In addition, sigma level of each type of complication will be calculated and reported.
2. Method
Six Sigma Methodology
As a quality improvement method, Six Sigma can be employed in order to eliminate complications encountered during and after many ophthalmic surgeries [15] . Originally initiated by Motorola, Honeywell and General Electric [16] , Six Sigma is a powerful performance improvement tool that is improving the outcomes of modern healthcare processes today [17] . Although it was initially introduced in manufacturing processes, it is being im- plemented in diagnostic imaging processes [18] - [20] , emergency room [21] , paramedic backup [22] , laboratory [23] , cataract surgery [15] radiology [24] , surgical site infections [25] , Intra Lase surgery [26] , LASIK surgery [27] , strabismus surgery [28] , intravitreal injections [29] , cataract surgery in patients with pseudoexfoliation syndrome [30] , pars plana vitrectomy [31] , phacoemulsification cataract surgery [32] , and stent insertion [14] as an effective way to improve quality, performance and productivity.
A Six Sigma process produces 3.4 defects per one million opportunities (DPMO) [33] . To eliminate defects, Six Sigma makes use of a structured methodology called DMAIC to find the root causes behind problems and to reach near perfect processes [34] . DMAIC can analyze and modify complicated time-sensitive healthcare pro- cesses involving multiple specialists and treatment areas by identifying and eliminating root causes of defects, errors or complications and thus minimizing healthcare process variability [17] [33] .
To achieve this, normal distribution underlies Six Sigma’s statistical assumptions [22] . An empirically-based 1.5 sigma shift is introduced into the calculation [22] . DPMO is calculated from Equation (1) as follows:
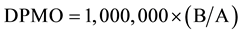 (1)
(1)
where A is the total number of PKP surgeries performed and B is the total number of post-operative complica- tions occurred.
The higher level of sigma after the initiation of Six Sigma indicates a lower rate of post-operative complica- tions and a more efficient process.
3. Analysis
Application of DMAIC for PKP Surgery
The eye care center decided that Six Sigma is the best way to achieve their goals. A surgical team was assembled and trained in the methodology. Committed and consistent leadership to overcome the complications was as- sured by this team. The surgical team firstly generated a SIPOC (Supplier, Input, Process, Output and Customer) Table for penetrative keratoplasty surgery process (Table 1).
The surgical team defined three postoperative performance objectives, namely improved visual acuity, excel- lent prognosis and clear cornea. They also defined a “complication” as any unwanted outcome inhibiting the pa- tient to be cured and stable which compounds the illness and decreases the patient’s quality of life or prolongs the planned hospital stay [14] . To achieve the performance objective, the surgical team first determined the Criti- cal-to-Quality (CTQ) factors by brainstorming. The CTQ factors were those factors that may have an influence on the objective.
The surgical team determined the metrics to measure existing process. The metrics to be chosen for a Six Sigma study were:
1) Total number of PKP surgeries performed in the eye care center,
2) Number of post-operative complications.
Data were collected for a period of 9-year on 23 females and 32 males [35] . In this period, PKP surgeries were performed on 59 eyes. Patients were aged between 8 and 78 with an average of 45.08. Complications had been noted as they occurred. The surgical team followed up the patients for 12 months and identified eleven types of complications and classified them as how soon they occur, i.e. acute and/or sub-acute and/or chronic (Table 2). Sources (Table 3) and root-causes (Table 4) of these complications were tabulated by type.
Table 1. SIPOC table for PKP surgery.
Table 2. Post-operative complications experienced.
Table 3. Sources of post-operative complications.
Table 4. Root-causes of post-operative complications.
The incidence of complications depended on multiple sources of variables. Measurement variables, surgeon variables, staff variables, patient variables and equipment variables were all evaluated when attempting to assess the root-cause of a complication (Table 3 and Table 4).
The surgical team analyzed the occurrence frequency of each complication (Table 4) and related them with the root-causes on Table 3. The analysis revealed that Types I, II and III were the three most frequently occur- ring complications in the PKP surgeries. Then, the CTQs are classified as “vital few factors” and “trivial many factors” according to how frequent they caused the complications. The “vital few” factors, i.e. the factors that had the most impact on the success of PKP surgery were determined to be patient’s anatomy and donor cornea. The other factors, i.e. experience of ophthalmic surgeon, sterilization and hygiene, and equipment were found to be the “trivial many” factors.
4. Discussion
The surgical team calculated the current DPMO and sigma levels for each complication type (Table 5). The process sigma level, calculated as the arithmetic average of eleven complications, was found to be 3.1418.
The highest sigma level was obtained for Types X and XI. The lowest sigma level was found to be belong to Type I. Having sigma levels lower than 4.00, all types of complications were alarming to be significantly re- duced.
Risk assessment of PKP surgeries was achieved by FMEA. Utilization of the FMEA involved break down the process into individual steps: potential failure modes (i.e. complications), severity score, probability score, ha- zard score, criticality and detection, so that the surgery team could look at key drivers in the process based on the past experience.
Complication trends and their consequences over a 9-year period had been monitored and recorded. Surgical team prioritized the complications according to how serious their consequences were (i.e. severity score), how frequently they occurred (i.e. probability score) and how easily they could be detected. Hazard analysis was em- ployed in order to identify failure modes and their causes and effects. The surgery team determined the severity of each complication and assigned scores for them. The severity of each complication was scored from 1 to 4 (Table 6).
For each complication type, the hazard score was calculated by multiplying the severity score with the proba- bility score. Consequently, an FMEA table was drawn (Table 7). Among the complications, Type I yielded the highest hazard score. Types VI and VII were equally hazardous complications and so were Types VIII and IX. According to FMEA, Type X was the least hazardous complication.
The surgical team developed preventative measures for each type of complication in order to bring the overall process under control. They implemented a corrective action plan to reduce and/or eliminate the complications (See Appendix).
5. Conclusions
In this study, authors identified and reported eleven types of post-operative complications encountered after PKP surgeries. These complications were almost always related to events that had occurred during surgery. The process sigma level of the overall process (i.e. cataract surgeries made in 9 years) was measured to be 3.1418.
Many complications were related to the suitability of the donor cornea and patient’s anatomy. Other root- causes were determined to be experience of ophthalmic surgeons, performance of equipment, and hygiene and
Table 5. Cumulative frequency, DPMO and sigma levels.
Table 6. Severity scores.
Table 7. FMEA table.
sterilization. The complication rates were reduced as ophthalmic surgeons gained experience and was trained on how to identify, minimize or eliminate the sources and root-causes of the complications. Sterilization of the op- erating room, equipment and instruments as well as the regular maintenance and calibration of the equipment were also essential.
Nonetheless, the surgical team concluded that the risks associated with PKP surgery could be minimized by taking the necessary preventative measures with appropriate preoperative, intraoperative and postoperative care.
Cite this paper
İbrahimŞahbaz,Mehmet TolgaTaner,Üzeyir TolgaŞahandar,GamzeKağan,EnginErbaş, (2014) Elimination of Post-Operative Complications in Penetrating Keratoplasty by Deploying Six Sigma. American Journal of Operations Research,04,189-196. doi: 10.4236/ajor.2014.44018
References
- 1. Krachmer, J.H., Mannis, M.J. and Holland, E.J. (2005) Cornea. 2nd Edition, Elsevier, Mosby.
- 2. Al-Yousuf, N., Mavrikakis, I., Mavrikakis, E. and Daya, S.M. (2004) Penetrating Keratoplasty: Indications over a 10-Year Period. British Journal of Ophthalmology, 88, 998-1001.
http://dx.doi.org/10.1136/bjo.2003.031948 - 3. EBAA (Eye Bank Association of America) (2013) Cost-Benefit Analysis of Corneal Transplant.
http://www.restoresight.org/wp-content/uploads/2013/10/Lewin-Study-Executive-Summary-.pdf - 4. Muraine, M., Christian, S. and Laure, W. (2003) Long Term Results of Penetrating Keratoplasty. Graefe’s Archive for Clinical and Experimental Ophthalmology, 681-699.
- 5. Severin, M. and Bartz-Schmidt, K.U. (2000) Penetrating Keratoplasty: Diagnosis and Treatment of Postoperative Complications. Springer-Verlag GmbH, Berlin.
http://dx.doi.org/10.1007/978-3-642-59684-1 - 6. Sayl1k, M. and Akarçay, K. (2002) Penetrating Keratoplasty: Indications and Postoperative Rehabilitation. Seminar Notes of Assistant Ophthalmic Surgeons, Istanbul.
- 7. Ing, J.J., Ing, H.H., Nelson, L.R., Hodge, D.O. and Bourne, W.M. (1998) Ten-Year Postoperative Results of Penetrating Keratoplasty. Ophthalmology, 105, 1855-1865.
http://dx.doi.org/10.1016/S0161-6420(98)91030-2 - 8. Tavakkoli, H. and Sugar, J. (1994) Microbial Keratitis Following Penetrating Keratoplasty. Ophthalmic Surgery, 25, 356-360.
- 9. Kloess, P.M., Stulting, R.D., Waring, G.O. and Wilson, L.A. (1993) Bacterial and Fungal Endolpthaimitis after Penetrating Keratoplasty. American Journal of Ophtalmology, 115, 309-316.
- 10. Stemberg, P., Meredith, T.A., Steward, M.A. and Kaplan, H.J. (1990) Retinal Detachment in Penetrating Keratoplasty Patients. American Journal of Ophthalmology, 109, 148-152.
- 11. Foulks, G.N. (1987) Glaucoma Associated with Penetrating Keratoplasty. Ophthalmology, 94, 871-874.
http://dx.doi.org/10.1016/S0161-6420(87)33542-0 - 12. Wade, M., Steinert, R.F., Garg, S., Farid, M. and Gaster, R. (2013) Results of Toric Intraocular Lenses for Post-Penetrating Keratoplasty Astigmatism. Ophthalmology, 121, 771-777.
http://dx.doi.org/10.1016/j.ophtha.2013.10.011 - 13. Fasolo, A., Capuzzo, C., Fornea, M., Franch, A., Birattari, F., Carito, G., Cucco, F., Prosdocimo, G., Sala, M., Delle-Noci, N., Primavera, V., Frigo, A., Grigoletto, F., Ponzin, D. and Cortes Study Group (2011) Risk Factors for Graft Failure after Penetrating Keratoplasty: 5-Year Follow-Up from the Corneal Transplant Epidemiological Study. Cornea, 30, 1328-1335.
http://dx.doi.org/10.1097/ICO.0b013e318206895a - 14. Taner, M.T., Kagan, G., Celik, S., Erbas, E. and Kagan, M.K. (2013) Formation of Six Sigma Infrastructure for the Coronary Stenting Process. International Review of Management and Marketing, 3, 232-242.
- 15. Taner, M.T. (2013) Application of Six Sigma Methodology to a Cataract Surgery Unit. International Journal of Health Care Quality Assurance, 26, 768-785.
http://dx.doi.org/10.1108/IJHCQA-02-2012-0022 - 16. Mehrjerdi, Y.Z. (2011) Six Sigma: Methodology, Tools and Its Future. International Journal of Assembly Automation, 31, 79-88.
http://dx.doi.org/10.1108/01445151111104209 - 17. Taner, M.T., Sezen, B. and Antony, J. (2007) An Overview of Six Sigma Applications in Healthcare Industry. International Journal of Health Care Quality Assurance, 20, 329-340.
http://dx.doi.org/10.1108/09526860710754398 - 18. Antony, J. and Banuelas, R. (2002) Key Ingredients for the Effective Implementation of Six Sigma Program. Measuring Business Excellence, 6, 20-27.
http://dx.doi.org/10.1108/13683040210451679 - 19. Antony, J., Antony, F.J., Kumar, M. and Cho, B.R. (2007) Six Sigma in Service Organisations: Benefits, Challenges and Difficulties, Common Myths, Empirical Observations and Success Factors. International Journal of Quality and Reliability Management, 24, 294-311.
http://dx.doi.org/10.1108/02656710710730889 - 20. Taner, M.T., Sezen, B. and Atwat, K.M. (2012) Application of Six Sigma Methodology to a Diagnostic Imaging Process. International Journal of Health Care Quality Assurance, 25, 274-290.
http://dx.doi.org/10.1108/09526861211221482 - 21. Miller, M.J., Ferrin, D.M. and Szymanski, J.M. (2003) Simulating Six Sigma Improvement Ideas for a Hospital Emergency Department. Proceedings of the IEEE Winter Simulation Conference, New Orleans, 7-10 December 2003, 1926-1929.
- 22. Taner, M.T. and Sezen, B. (2009) An Application of Six Sigma Methodology to Turnover Intentions in Healthcare. International Journal of Health Care Quality Assurance, 22, 252-265.
http://dx.doi.org/10.1108/09526860910953520 - 23. Nevalainen, D., Berte, L., Kraft, C., Leigh, E., Picaso, L. and Morgan, T. (2000) Evaluating Laboratory Performance on Quality Indicators with the Six Sigma Scale. Archives of Pathology and Laboratory Medicine, 124, 516-519.
- 24. Cherry, J. and Seshadri, S. (2000) Six Sigma: Using Statistics to Reduce Process Variability and Costs in Radiology. Radiology Management, 22, 42-49.
- 25. Pexton, C. and Young, D. (2004) Reducing Surgical Site Infections through Six Sigma and Change Management. Patient Safety and Quality Healthcare, 1, 1-8.
- 26. Sahbaz, I., Taner, M.T., Eliacik, M., Kagan, G. and Erbas, E. (2014) Adoption of Six Sigma’s DMAIC to Reduce Complications in IntraLase Surgeries. International Journal of Statistics in Medical Research, 3, 126-133.
http://dx.doi.org/10.6000/1929-6029.2014.03.02.6 - 27. Taner, M.T., Kagan, G., Sahbaz, I., Erbas, E. and Kagan, S.B. (2014) A Preliminary Study for Six Sigma Implementation in Laser in Situ Keratomileusis (LASIK) Surgeries. International Review of Management and Marketing, 4, 24-33.
- 28. Taner, M.T., Sahbaz, I., Kagan, G., Atwat, K. and Erbas, E. (2014) Development of Six Sigma Infrastructure for Strabismus Surgeries. International Review of Management and Marketing, 4, 49-58.
- 29. Sahbaz, I., Taner, M.T., Eliacik, M., Kagan, G., Erbas, E. and Enginyurt, H. (2014) Deployment of Six Sigma Methodology to Reduce Complications in Intravitreal Injections. International Review of Management and Marketing, 4, 160-166.
- 30. Sahbaz, I., Taner, M.T., Kagan, G., Sanisoglu, H., Durmus, E., Tunca, M., Erbas, E., Kagan, S.B., Kagan, M.K. and Enginyurt, H. (2014) Development of a Six Sigma Infrastructure for Cataract Surgery in Patients with Pseudoexfoliation Syndrome. Archives of Business Research, 2, 15-23.
http://dx.doi.org/10.14738/abr.22.173 - 31. Sahbaz, I., Taner, M.T., Sanisoglu, H., Kar, T., Kagan, G., Durmus, E., Tunca, M., Erbas, E., Armagan, I. and Kagan, M.K. (2014) Deployment of Six Sigma Methodology to Pars Plana Vitrectomy. International Journal of Statistics in Medical Research, 3, 94-102.
http://dx.doi.org/10.6000/1929-6029.2014.03.02.3 - 32. Sahbaz, I., Taner, M.T., Kagan, G., Sanisoglu, H., Erbas, E., Durmus, E., Tunca, M. and Enginyurt, H. (2014) Deployment of Six Sigma Methodology in Phacoemulsification Cataract Surgeries. International Review of Management and Marketing, 4, 123-131.
- 33. Buck, C. (2001) Application of Six Sigma to Reduce Medical Errors. Annual Quality Congress Proceedings, Charlotte, 11-15 April 2001, 739-742.
- 34. Park, S.H. and Antony, J. (2008) Robust Design for Quality Engineering and Six Sigma. World Scientific Publishing, New Jersey.
http://dx.doi.org/10.1142/6655 - 35. Sahandar, U.T. (2005) Our Penetrating Keratoplasty Results, Istanbul. Doctor of Medicine Thesis.
Appendix
NOTES
*Corresponding author.



